The Art and Science of Connection – by Kasley Killam, MPH
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We can eat well, exercise well, and even sleep well, and we’ll still have a +53% increased all-cause mortality if we lack social connection—even if we technically have support and access to social resources, just not the real human connection itself. And as we get older, it gets increasingly easy to find ourselves isolated.
The author is a social scientist by profession, and it shows. None of what she shares in the book is wishy-washy; it has abundant scientific references coming thick and fast, and a great deal of clarity with regard to terms, something often not found in books of this genre that lean more towards the art than the science.
On which note, for the reader who may be thinking “I am indeed quite alone”, she also offers proven techniques for remedying that; not in the way that many books use the word “proven” to mean “we got some testimonials”, but rather, proven in the sense of “we did science to it and based on these 17 large population-based retrospective cohort studies, we can say with 99% confidence that this is an effective tool to mediate improved social bonds and social health outcomes”.
To this end, it’s a very practical book also, and should bestow upon any isolated reader a sense of confidence that in fact, things can be better. A particular strength is that it also looks at many different scenarios, so for the “what if I…” people with clear reasons why social connection is not abundantly available, yes, she has such cases covered too.
Bottom line: if you’d like to live more healthily for longer, social health is an underrated and oft-forgotten way of greatly increasing those things, by science.
Click here to check out The Art And Science Of Social Connection, and get connected!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How (And Why) To Train Your Pre-Frontal Cortex
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Chapman’s Keys For Mental Focus
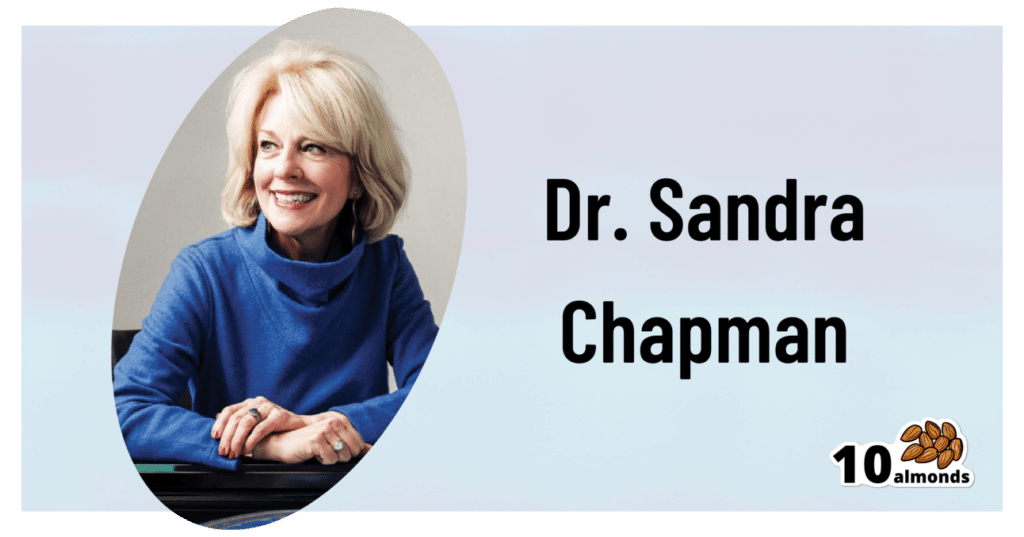
This is Dr. Sandra Chapman; she’s a cognitive neuroscientist, on a mission to, in her words, further our understanding of:
- what makes the brain stronger, faster and last longer
- what enhances human cognitive capacity, and
- what enhances the underlying brain systems across the lifespan.
To this end, she’s also the founder and Chief Director of the Center For Brain Health, where she has worked on her mission for the past 25 years (clocking up hundreds of peer-reviewed publications to her name), as well as being a professor of Behavioral and Brain Sciences at UT Dallas.
What does she want us to know?
Get your brain into gear
When it comes to your brainpower, it is “use it or lose it”, but it is also perfectly possible to use it and lose it.
Why?
Very often, what we are using our brains for is high-strain, low-yield stuff, such as multitasking, overthinking, or overthinking while multitasking. And to make it worse, we often do it without sufficient rest.
This is the equivalent of owning a Ferrari but trying to drive it in second and third gear at once by switching between the two as rapidly as possible. And doing that for 18 hours each day.
Suffice it to say, you’ll be going nowhere quickly.
An alternative “use” of brainpower is low-strain, low-yield stuff, such as having to pay close attention to a boring conversation. It’s enough to stop your mind from doing anything else, but not enough to actually stimulate you.
This is the equivalent of owning a Ferrari but keeping it idling. The wear and tear is minimal this time, but you’re not actually going anywhere either.
Better, of course, are the other two quadrants:
- low-strain, high-yield: consistently using our brain in relatively non-taxing ways that encourage its development
- high-strain, high-yield: here the Ferrari metaphor definitely fails, because unlike cars, our bodies (including our brains) are machines that benefit from judicious regular progressive overloading (but just by a bit, and with adequate recovery time between overloads).
See also: 12 Weeks To Measurably Boost Your Brain
How to do the “low-strain, low-yield” part
When it comes to “what’s the most important part of the brain to help in the face of cognitive decline?” the usual answer is either to focus on memory (hippocampi) or language (various parts, but for example Wernicke’s area and Broca’s area), since people most fear losing memory, and language is very important both socially and practically.
Those are indeed critical, and we at 10almonds stand by them, but Dr. Chapman (herself having originally trained as speech and language pathologist!) makes a strong case for adding a third brain part to the list.
Specifically, she advocates for strengthening the pre-frontal cortex, which is responsible for inhibition, task-switching, working memory, and cognitive flexibility. If that seems like a lot, do remember it’s a whole cortex and not one of the assorted important-but-small brain bits we mentioned above.
How? She has developed training programs for this, based on what she calls Strategic Memory Advanced Reasoning Tactics (SMART), to support support attention, planning, judgment and emotional management.
You can read more about those programs here:
Center For Brain Health | Our Programs
Participation in those is mostly not free, however, if you join their…
Center For Brain Health | BrainHealth Project
…then they will periodically invite you to join pilot programs, research programs, and the like, which will either be free or they-pay-you affairs—because this is how science is done, and you can read about yourself (anonymized, of course) later in peer-reviewed papers of the kind we often cite here.
If you’re not interested in any of that though, we will say that according to Dr. Chapman, the keys are:
Inhibition: be conscious of this function of your brain, and develop it. This is the function of your brain that stops you from making mistakes—or put differently: stops you from saying/doing something stupid.
Switching: do this consciously; per “I am now doing this task, now I am switching to this other task”, rather than doing the gear-grinding thing we discussed earlier
Working memory: this is effectively your brain’s RAM. Unlike the RAM of a computer (can be enhanced by adding another chip or replacing with a bigger chip), our brain’s RAM can be increased by frequent use, and especially by judicious use of progressive overloading (with rests between!) which we’ll discuss in the high-strain, high-yield section.
Flexibility: this is about creative problem-solving, openness to new ideas, and curiosity
See also: Curiosity Kills The Neurodegeneration
How to do the “high-strain, high-yield” part
Delighting this chess-playing writer, Dr. Chapman recommends chess. Although, similar games such as go (a Chinese game that looks simpler than chess but actually requires more calculation) work equally well too.
Why?
Games like chess and go cause structural changes that are particularly helpful, in terms of engaging in such foundational tasks as learning, abstract reasoning, problem-solving and self-control:
Chess Practice as a Protective Factor in Dementia
Basically, it checks (so to speak) a lot of boxes, especially for the pre-frontal cortex. Some notes:
- Focusing on the game is required for brain improvement; simply pushing wood casually will not do it. Ideally, calculating several moves ahead will allow for strong working memory use (because to calculate several moves ahead, one will have to hold increasingly many possible positions in the mind while doing so).
- The speed of play must be sufficiently slow as to allow not only for thinking, but also for what in chess is called “blunder-checking”, in other words, having decided on one’s move, pausing to consider whether it is a mistake, and actively trying to find evidence that it is. This is the crucial “inhibition habit”, and when one does it reflexively, one will make fewer mistakes. Tying this to dementia, see for example how one of the common symptoms of dementia is falling for scams that one wouldn’t have previously. How did cognitive decline make someone naïve? It didn’t, per se; it just took away their ability to, having decided what to do, pause to consider whether it was a mistake, and actively trying to find evidence that it is.
- That “conscious switching” that we talked about, rather than multitasking? In chess, there is a difference between strategy and tactics. Don’t worry about what that difference is for now (learn it if you want to take up chess), but know that strong players will only strategize while it is their opponent’s turn, and only calculate (tactics) while it is their own turn. It’s very tempting to flit constantly between one and the other, but chess requires players to have the mental discipline be able to focus on one task or the other and stick with that task until it’s the appointed time to switch.
If you feel like taking up chess, this site (and related app, if you want it) is free (it’s been funded by voluntary donations for a long time now) and good and even comes with free tuition and training tools: LiChess.org
Here’s another site that this writer (hi, it’s me) personally uses—it has great features too, but many are paywalled (I’m mostly there just because I’ve been there nearly since its inception, so I’m baked into the community now): Chess.com
Want to know more?
You might like this book by Dr. Chapman, which we haven’t reviewed yet but it did inform large parts of today’s article:
Make Your Brain Smarter: Increase Your Brain’s Creativity, Energy, and Focus – by Dr. Sandra Chapman
Enjoy!
Share This Post
-
Beetroot vs Pumpkin – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to pumpkin, we picked the beetroot.
Why?
It was close! And an argument could be made for either.
In terms of macros, beetroot has about 3x more protein and about 3x more fiber, as well as about 2x more carbs, making it the “more food per food” option. While both have a low glycemic index, we picked the beetroot here for its better numbers overall.
In the category of vitamins, beetroot has more of vitamins B6 and B9, while pumpkin has more of vitamins A, B2, B3, B5, E, and K. So, a fair win for pumpkin this time.
When it comes to minerals, though, beetroot has more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pumpkin has a tiny bit more copper. An easy win for beetroot here.
In short, both are great, and although pumpkin shines in the vitamin category, beetroot wins on overall nutritional density.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what it can do
Take care!
Share This Post
-
From eye exams to blood tests and surgery: how doctors use light to diagnose disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is the next article in our ‘Light and health’ series, where we look at how light affects our physical and mental health in sometimes surprising ways. Read other articles in the series.
You’re not feeling well. You’ve had a pounding headache all week, dizzy spells and have vomited up your past few meals.
You visit your GP to get some answers and sit while they shine a light in your eyes, order a blood test and request some medical imaging.
Everything your GP just did relies on light. These are just some of the optical technologies that have had an enormous impact in how we diagnose disease.
megaflopp/Shutterstock 1. On-the-spot tests
Point-of-care diagnostics allow doctors to test patients on the spot and get answers in minutes, rather than sending samples to a lab for analysis.
The “flashlight” your GP uses to view the inside of your eye (known as an ophthalmoscope) is a great example. This allows doctors to detect abnormal blood flow in the eye, deformations of the cornea (the outermost clear layer of the eye), or swollen optical discs (a round section at the back of the eye where the nerve link to the brain begins). Swollen discs are a sign of elevated pressure inside your head (or in the worst case, a brain tumour) that could be causing your headaches.
The invention of lasers and LEDs has enabled many other miniaturised technologies to be provided at the bedside or clinic rather than in the lab.
Pulse oximetry is a famous example, where a clip attached to your finger reports how well your blood is oxygenated. It does this by measuring the different responses of oxygenated and de-oxygenated blood to different colours of light.
Pulse oximetry is used at hospitals (and sometimes at home) to monitor your respiratory and heart health. In hospitals, it is also a valuable tool for detecting heart defects in babies.
See that clip on the patient’s finger? That’s a pulse oximeter, which relies on light to monitor respiratory and heart health. CGN089/Shutterstock 2. Looking at molecules
Now, back to that blood test. Analysing a small amount of your blood can diagnose many different diseases.
A machine called an automated “full blood count analyser” tests for general markers of your health. This machine directs focused beams of light through blood samples held in small glass tubes. It counts the number of blood cells, determines their specific type, and reports the level of haemoglobin (the protein in red blood cells that distributes oxygen around your body). In minutes, this machine can provide a snapshot of your overall health.
For more specific disease markers, blood serum is separated from the heavier cells by spinning in a rotating instrument called a centrifuge. The serum is then exposed to special chemical stains and enzyme assays that change colour depending on whether specific molecules, which may be the sign of a disease, are present.
These colour changes can’t be detected with the naked eye. However, a light beam from an instrument called a spectrometer can detect tiny amounts of these substances in the blood and determine if the biomarkers for diseases are present, and at what levels.
Light shines through the blood sample and tells us whether biomarkers for disease are present. angellodeco/Shutterstock 3. Medical imaging
Let’s re-visit those medical images your GP ordered. The development of fibre-optic technology, made famous for transforming high-speed digital communications (such as the NBN), allows light to get inside the body. The result? High-resolution optical imaging.
A common example is an endoscope, where fibres with a tiny camera on the end are inserted into the body’s natural openings (such as your mouth or anus) to examine your gut or respiratory tracts.
Surgeons can insert the same technology through tiny cuts to view the inside of the body on a video screen during laparoscopic surgery (also known as keyhole surgery) to diagnose and treat disease.
Doctors can insert this flexible fibre-optic tube with a camera on the end into your body. Eduard Valentinov/Shutterstock How about the future?
Progress in nanotechnology and a better understanding of the interactions of light with our tissues are leading to new light-based tools to help diagnose disease. These include:
- nanomaterials (materials on an extremely small scale, many thousands of times smaller than the width of a human hair). These are being used in next-generation sensors and new diagnostic tests
- wearable optical biosensors the size of your fingernail can be included in devices such as watches, contact lenses or finger wraps. These devices allow non-invasive measurements of sweat, tears and saliva, in real time
- AI tools to analyse how blood serum scatters infrared light. This has allowed researchers to build a comprehensive database of scatter patterns to detect any cancer
- a type of non-invasive imaging called optical coherence tomography for more detailed imaging of the eye, heart and skin
- fibre optic technology to deliver a tiny microscope into the body on the tip of a needle.
So the next time you’re at the GP and they perform (or order) some tests, chances are that at least one of those tests depend on light to help diagnose disease.
Matthew Griffith, Associate Professor and ARC Future Fellow and Director, UniSA Microscopy and Microanalysis Facilities, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Strong Bones Forever − by Dr. Raymond Hinish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This doctor of pharmacy would like for fewer people to take (or need to take) osteoporosis medications. Indeed, as the subtitle suggests, the focus here is on drug-free solutions.
And not just because “natural is better” as an argument without evidence, rather, he talks about the limitations and drawbacks of osteoporosis medications (which we wrote about previously, but he has more room to go into more detail), whereupon some osteoporosis meds may do more harm than good.
His method boasts improvements in bone density by 11% or more in two years, and covers such topics as:
- which calcium (and why no, dairy is not what you want; it contains things that inhibit calcium absorption, so the calcium will be stuck in your arteries instead of your bones)
- which minerals are more important than calcium, and why
- common mistakes that many people make that sabotage their bone density
It’s about more than just diet though; he does also talk about hormones, and not just other lifestyle factors, but also many “industry secrets” that aren’t really secrets per se, it’s just, people outside of the industry don’t usually know them—pertaining to things like how to get the most out of bone density tests (i.e. how to get better accuracy), how to meaningfully assess fracture risk, and, if choosing to take osteoporosis meds, how to minimize the risks and maximize the benefits.
The style is very direct and informational, very easy to read, remarkably jargon-free, and our only criticism is that there is no bibliography.
Bottom line: if you’d like to improve your bone density, this book can certainly help with that.
Click here to check out Strong Bones Forever, and have strong bones forever!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Five Supplements That Actually Work Vs Arthritis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Diana Girnita, a double board-certified physician (internal medicine & rheumatology) who, in addition to her MD, also has a PhD in immunology—bearing in mind that rheumatoid arthritis is an autoimmune condition.
Her mission is to help people with any form of arthritis (rheumatoid or otherwise) and those with many non-arthritic autoimmune conditions (ranging from tendonitis to lupus) to live better.
Today, we’ll be looking at her recommendations of 5 supplements that actually help alleviate arthritis:
Collagen
Collagen famously supports skin, nails, bones, and joint cartilage; Dr. Girnita advises that it’s particularly beneficial for osteoarthritis.
Specifically, she recommends either collagen peptides or hydrolyzed collagen, as they are most absorbable. However, collagen can also be sourced from foods like bone broth, fish with skin and bones, and gelatin-based foods.
If you’re vegetarian/vegan, then it becomes important to simply consume the ingredients for collagen, because like most animals, we can synthesize it ourselves provided we get the necessary nutrients. For more on that, see:
We Are Such Stuff As Fish Are Made Of
Glucosamine & chondroitin
Technically two things, but almost always sold/taken together. Naturally found in joint cartilage, it can slow cartilage breakdown and reduce pain in osteoarthritis.
Studies show pain relief, especially in moderate-to-severe cases; best taken long-term. Additionally, it’s a better option than NSAIDs for patients with heart or gastrointestinal issues.
10almonds tip: something that’s tricker to find as a supplement than glucosamine and chondroitin, but you might want to check it out:
Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
Omega-3 fatty acids
Dr. Girnita recommends this one because unlike the above recommendations that mainly help reduce/reverse the joint damage itself, omega-3 reduces inflammation, pain, and stiffness, and can decrease or eliminate the need for NSAIDs in rheumatoid arthritis and psoriatic arthritis.
She recommends 2-4g EPA/DHA daily; ideally taken with a meal for better absorption.
She also recommends to look for mercury-free options—algae-derived are usually better than fish-derived, but check for certification either way! See also:
What Omega-3 Fatty Acids Really Do For Us
Boswellia serrata (frankincense)
Popularly enjoyed as an incense but also available in supplement form, it contains boswellic acid, which reduces inflammation and cartilage damage.
Dr. Girnita recommends 100 mg daily, but advises that it may interact with some antidepressants, anti-anxiety medications, and NSAIDs—so speak with your pharmacist/doctor if unsure.
We also wrote about this one here:
Science-Based Alternative Pain Relief
Curcumin (turmeric)
Well-known for its potent anti-inflammatory properties, it’s comparable to NSAIDs in pain relief for most common forms of arthritis.
Dr. Girnita recommends 1–1.5g of curcumin daily, ideally combined with black pepper for better absorption:
Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Lastly…
Dr. Girnita advises to not blindly trust supplements, but rather, to test them for 2–3 months while keeping a journal of your symptoms. If it improves things for you, keep it up, if not, discontinue. Humans can be complicated and not everything will work exactly the same way for everyone!
For more on dealing with chronic pain specifically, by the way, check out:
Managing Chronic Pain (Realistically!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
‘I keep away from people’ – combined vision and hearing loss is isolating more and more older Australians
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our ageing population brings a growing crisis: people over 65 are at greater risk of dual sensory impairment (also known as “deafblindness” or combined vision and hearing loss).
Some 66% of people over 60 have hearing loss and 33% of older Australians have low vision. Estimates suggest more than a quarter of Australians over 80 are living with dual sensory impairment.
Combined vision and hearing loss describes any degree of sight and hearing loss, so neither sense can compensate for the other. Dual sensory impairment can occur at any point in life but is increasingly common as people get older.
The experience can make older people feel isolated and unable to participate in important conversations, including about their health.
bricolage/Shutterstock Causes and conditions
Conditions related to hearing and vision impairment often increase as we age – but many of these changes are subtle.
Hearing loss can start as early as our 50s and often accompany other age-related visual changes, such as age-related macular degeneration.
Other age-related conditions are frequently prioritised by patients, doctors or carers, such as diabetes or heart disease. Vision and hearing changes can be easy to overlook or accept as a normal aspect of ageing. As an older person we interviewed for our research told us
I don’t see too good or hear too well. It’s just part of old age.
An invisible disability
Dual sensory impairment has a significant and negative impact in all aspects of a person’s life. It reduces access to information, mobility and orientation, impacts social activities and communication, making it difficult for older adults to manage.
It is underdiagnosed, underrecognised and sometimes misattributed (for example, to cognitive impairment or decline). However, there is also growing evidence of links between dementia and dual sensory loss. If left untreated or without appropriate support, dual sensory impairment diminishes the capacity of older people to live independently, feel happy and be safe.
A dearth of specific resources to educate and support older Australians with their dual sensory impairment means when older people do raise the issue, their GP or health professional may not understand its significance or where to refer them. One older person told us:
There’s another thing too about the GP, the sort of mentality ‘well what do you expect? You’re 95.’ Hearing and vision loss in old age is not seen as a disability, it’s seen as something else.
Isolated yet more dependent on others
Global trends show a worrying conundrum. Older people with dual sensory impairment become more socially isolated, which impacts their mental health and wellbeing. At the same time they can become increasingly dependent on other people to help them navigate and manage day-to-day activities with limited sight and hearing.
One aspect of this is how effectively they can comprehend and communicate in a health-care setting. Recent research shows doctors and nurses in hospitals aren’t making themselves understood to most of their patients with dual sensory impairment. Good communication in the health context is about more than just “knowing what is going on”, researchers note. It facilitates:
- shorter hospital stays
- fewer re-admissions
- reduced emergency room visits
- better treatment adherence and medical follow up
- less unnecessary diagnostic testing
- improved health-care outcomes.
‘Too hard’
Globally, there is a better understanding of how important it is to maintain active social lives as people age. But this is difficult for older adults with dual sensory loss. One person told us
I don’t particularly want to mix with people. Too hard, because they can’t understand. I can no longer now walk into that room, see nothing, find my seat and not recognise [or hear] people.
Again, these experiences increase reliance on family. But caring in this context is tough and largely hidden. Family members describe being the “eyes and ears” for their loved one. It’s a 24/7 role which can bring frustration, social isolation and depression for carers too. One spouse told us:
He doesn’t talk anymore much, because he doesn’t know whether [people are] talking to him, unless they use his name, he’s unaware they’re speaking to him, so he might ignore people and so on. And in the end, I noticed people weren’t even bothering him to talk, so now I refuse to go. Because I don’t think it’s fair.
Dual sensory loss can be isolating for older people and carers. Synthex/Shutterstock So, what can we do?
Dual sensory impairment is a growing problem with potentially devastating impacts.
It should be considered a unique and distinct disability in all relevant protections and policies. This includes the right to dedicated diagnosis and support, accessibility provisions and specialised skill development for health and social professionals and carers.
We need to develop resources to help people with dual sensory impairment and their families and carers understand the condition, what it means and how everyone can be supported. This could include communication adaptation, such as social haptics (communicating using touch) and specialised support for older adults to navigate health care.
Increasing awareness and understanding of dual sensory impairment will also help those impacted with everyday engagement with the world around them – rather than the isolation many feel now.
Moira Dunsmore, Senior Lecturer, Sydney Nursing School, Faculty of Medicine and Health, University of Sydney, University of Sydney; Annmaree Watharow, Lived Experience Research Fellow, Centre for Disability Research and Policy, University of Sydney, and Emily Kecman, Postdoctoral research fellow, Department of Linguistics, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: