How much time should you spend sitting versus standing? New research reveals the perfect mix for optimal health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People have a pretty intuitive sense of what is healthy – standing is better than sitting, exercise is great for overall health and getting good sleep is imperative.
However, if exercise in the evening may disrupt our sleep, or make us feel the need to be more sedentary to recover, a key question emerges – what is the best way to balance our 24 hours to optimise our health?
Our research attempted to answer this for risk factors for heart disease, stroke and diabetes. We found the optimal amount of sleep was 8.3 hours, while for light activity and moderate to vigorous activity, it was best to get 2.2 hours each.
Finding the right balance
Current health guidelines recommend you stick to a sensible regime of moderate-to vigorous-intensity physical activity 2.5–5 hours per week.
However mounting evidence now suggests how you spend your day can have meaningful ramifications for your health. In addition to moderate-to vigorous-intensity physical activity, this means the time you spend sitting, standing, doing light physical activity (such as walking around your house or office) and sleeping.
Our research looked at more than 2,000 adults who wore body sensors that could interpret their physical behaviours, for seven days. This gave us a sense of how they spent their average 24 hours.
At the start of the study participants had their waist circumference, blood sugar and insulin sensitivity measured. The body sensor and assessment data was matched and analysed then tested against health risk markers — such as a heart disease and stroke risk score — to create a model.
Using this model, we fed through thousands of permutations of 24 hours and found the ones with the estimated lowest associations with heart disease risk and blood-glucose levels. This created many optimal mixes of sitting, standing, light and moderate intensity activity.
When we looked at waist circumference, blood sugar, insulin sensitivity and a heart disease and stroke risk score, we noted differing optimal time zones. Where those zones mutually overlapped was ascribed the optimal zone for heart disease and diabetes risk.
You’re doing more physical activity than you think
We found light-intensity physical activity (defined as walking less than 100 steps per minute) – such as walking to the water cooler, the bathroom, or strolling casually with friends – had strong associations with glucose control, and especially in people with type 2 diabetes. This light-intensity physical activity is likely accumulated intermittently throughout the day rather than being a purposeful bout of light exercise.
Our experimental evidence shows that interrupting our sitting regularly with light-physical activity (such as taking a 3–5 minute walk every hour) can improve our metabolism, especially so after lunch.
While the moderate-to-vigorous physical activity time might seem a quite high, at more than 2 hours a day, we defined it as more than 100 steps per minute. This equates to a brisk walk.
It should be noted that these findings are preliminary. This is the first study of heart disease and diabetes risk and the “optimal” 24 hours, and the results will need further confirmation with longer prospective studies.
The data is also cross-sectional. This means that the estimates of time use are correlated with the disease risk factors, meaning it’s unclear whether how participants spent their time influences their risk factors or whether those risk factors influence how someone spends their time.
Australia’s adult physical activity guidelines need updating
Australia’s physical activity guidelines currently only recommend exercise intensity and time. A new set of guidelines are being developed to incorporate 24-hour movement. Soon Australians will be able to use these guidelines to examine their 24 hours and understand where they can make improvements.
While our new research can inform the upcoming guidelines, we should keep in mind that the recommendations are like a north star: something to head towards to improve your health. In principle this means reducing sitting time where possible, increasing standing and light-intensity physical activity, increasing more vigorous intensity physical activity, and aiming for a healthy sleep of 7.5–9 hours per night.
Beneficial changes could come in the form of reducing screen time in the evening or opting for an active commute over driving commute, or prioritising an earlier bed time over watching television in the evening.
It’s also important to acknowledge these are recommendations for an able adult. We all have different considerations, and above all, movement should be fun.
Christian Brakenridge, Postdoctoral research fellow at Swinburne University Centre for Urban Transitions, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fitness Walking and Bodyweight Exercises – by Frank S. Ring
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of exercise manuals assume that the reader has a “basic” body (nothing Olympian, but nothing damaged either). As we get older, increasingly few of us fall into the “but nothing damaged either” category!
Here’s where Ring brings to bear his decades of experience as a coach and educator, and also his personal recovery from a serious back injury.
The book covers direct, actionable exercise advice (with all manner of detail), and also offers mental health tips he’s learned along the way.
Ring, like us, is a big fan of keeping things simple, so he focusses on “the core four” of bodyweight exercises:
- Pushups
- Squats
- Lunges
- Planks
These four exercises get a whole chapter devoted to them, though! Because there are ways to make each exercise easier or harder, or have different benefits. For example, adjustments include:
- Body angle
- Points of contact
- Speed
- Pausing
- Range of motion
This, in effect, makes a few square meters of floor (and perhaps a chair or bench) your fully-equipped gym.
As for walking? Ring enjoys and extols the health benefits, and/but also uses his walks a lot for assorted mental exercises, and recommends we try them too.
A fine book for anyone who wants to gain and/or maintain good health, but doesn’t pressingly want to join a gym or start pumping iron!
Share This Post
-
Healthy Cook’s Anti-Inflammatory Diet & Cookbook – by Dr. Albert Orbinati
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is a root cause of very many illnesses, and exacerbates almost all the ones it doesn’t cause. So, reducing inflammation is a very good way to stay well in general, reducing one’s risk factors for very many other diseases.
Dr. Orbinati starts by giving advice for adjusting to an anti-inflammatory diet, including advice on trying an elimination diet, if you suspect an undiagnosed allergy/intolerance.
Thereafter, he gives guidance on pantry-stocking—not just what anti-inflammatory foods to include and what inflammatory foods to skip, but also, what food and nutrient pairings are particularly beneficial, like how black pepper and turmeric are both anti-inflammatory by themselves, but the former greatly increases the bioavailability of the latter if consumed together.
The rest of the book—aside from assorted appendices, such as 8 pages of scientific references—is given over to the recipes.
The recipes themselves are, obviously, anti-inflammatory in focus. As one might expect, therefore, most are vegetarian and many are vegan, but we do find many recipes with chicken and fish as well; there’s also some use of eggs and fermented dairy in some of the recipes too.
The book certainly does deliver on its promise of flavorful healthy food; that’s what happens when one includes a lot of herbs and spices in one’s cooking, as well as the fact that many other polyphenol-rich foods are, by nature, tasty in and of themselves.
Bottom line: if you’d like to expand your anti-inflammatory culinary repertoire, this book is a top-tier choice for that.
Click here to check out Healthy Cook’s Anti-Inflammatory Diet & Cookbook, and spice up your kitchen!
Share This Post
-
The Science of Self-Learning – by Peter Hollins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Teaching oneself new things is often the most difficult kind of bootstrapping, especially when one is unsure of such critical things as:
- Where to begin? How, for that matter, do we find where to begin?
- What can/should a learning journey look like?
- What challenges should we expect, and how will we overcome them?
Hollins answers all of these questions and more. The greatest value of this book is perhaps in its clear presentation of concrete step-by-step instructions. Hollins gives illustrated examples too, but most importantly, he gives models that can be applied to any given type of learning.
The book also covers the most difficult problems most people face when trying to learn something by themselves, including:
- Keeping oneself on-task (maintaining discipline)
- Measuring progress (self-testing beyond memorization)
- Keeping a fair pace of progress (avoiding plateaus)
- How to know when one’s knowledge is sufficient or not (avoiding Dunning-Kruger Club)
All in all, if you’re looking to learn a new subject or skill, this could be a first step that saves you a lot of time later!
Get your copy of the Science of Self-Learning on Amazon today!
Share This Post
Related Posts
-
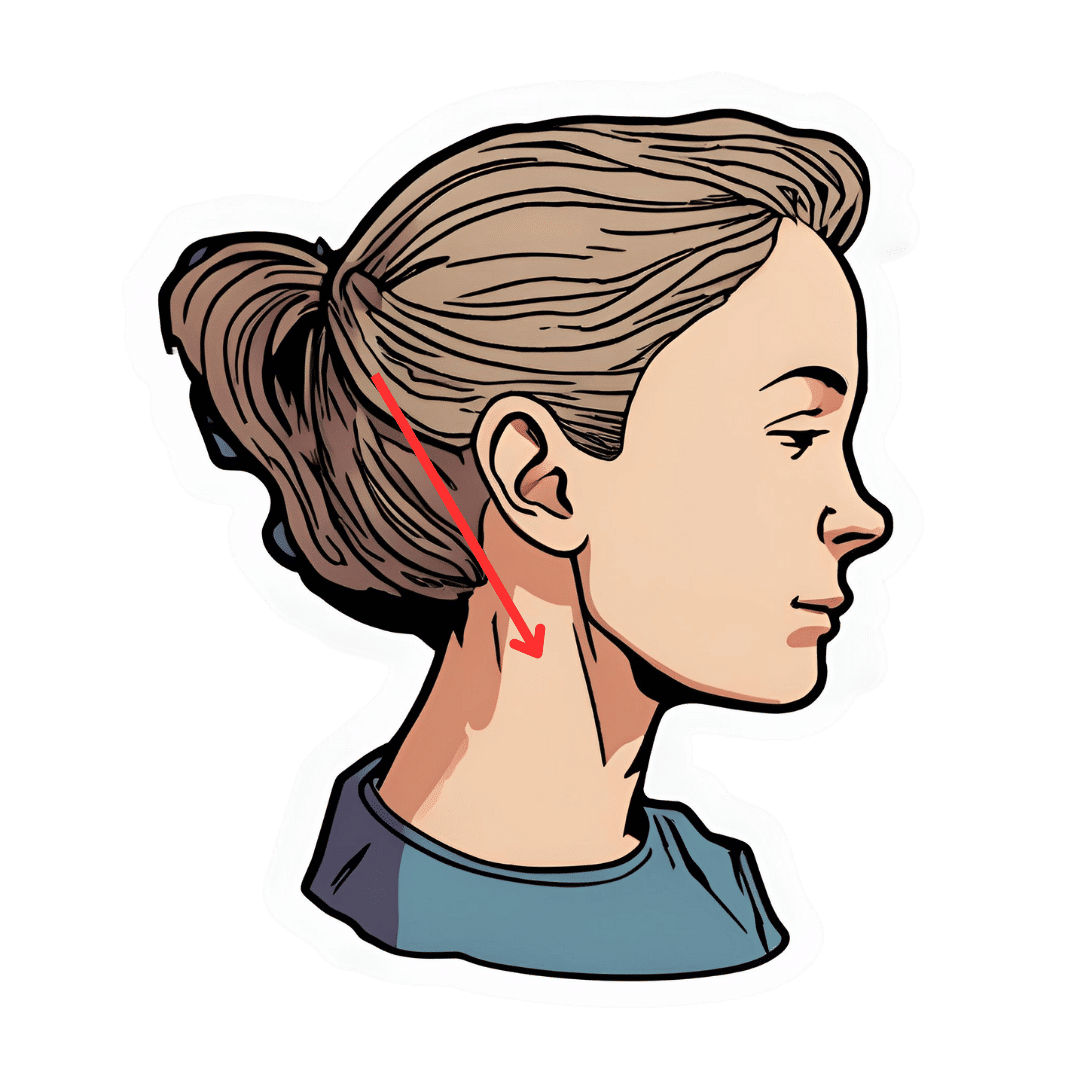
The Vagus Nerve’s Power for Weight Loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Arun Dhir is a university lecturer, a gastrointestinal surgeon, an author, and a yoga and meditation instructor, and he has this to say:
Gut feelings
The vagus nerve is the 10th cranial nerve, also known as “vagus” (“the wanderer”), because it travels from the brain to many other body parts, including the ears, throat, heart, respiratory system, gut, pancreas, liver, and reproductive system. It’s no surprise then, that it plays a key role in brain-gut communication and metabolism regulation.
The vagus nerve is part of the parasympathetic nervous system, responsible for rest, digestion, and counteracting the stress response. Most signals through the vagus nerve travel from the gut to the brain, though there is communication in both directions.
You may be beginning to see how this works and its implications for weight management: the vagus nerve senses metabolites from the liver, pancreas, and small intestine, and regulates insulin production by stimulating beta cells in the pancreas, which is important for avoiding/managing insulin resistance and metabolic syndrome in general.
Dr. Dhir cites a study in which vagus nerve stimulation (originally used for treating epilepsy and depression) was shown to cause unintentional weight loss (6-11%) in patients, revealing a link to weight management. Of course, that is quite a specific sample, so more research is needed to say for sure, but because the principle is very sound and the mechanism of action is clear, it’s not being viewed as a controversial conclusion.
As for how get these benefits, here are seven ways:
- Cold water on the face: submerge your face in cold water in the morning while holding water in your mouth, or cover your face with a cold wet washcloth (while holding your breath please; no need to waterboard yourself!), which activates the “mammalian dive response” in which your body activates the parasympathetic nervous system in order to remain calm and thus survive for longer underwater
- Alternate hot and cold showers: switch between hot and cold water during showers for 10-second intervals; this creates eustress and activates the process of hormesis, improving your overall stress management and reducing any chronic stress response you may otherwise have going on
- Humming and gargling: the vibrations in the throat stimulate the nearby vagus nerve
- Deep breathing (pranayama): yoga breathing exercises, especially combined with somatic exercises such as the sun salutation, can stimulate the vagus nerve
- Intermittent fasting: helps recalibrate the metabolism and indirectly improves vagus nerve function
- Massage and acupressure: stimulates lymphatic channels and the vagus nerve
- Long walks in nature (“forest bathing”): helps trigger relaxation in general
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Vagus Nerve (And How You Can Make Use Of It)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 4 Best Stretches To Do Before Bed (And Even: To Do In Bed!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Contrary to the stereotype of early morning yoga sessions, the evening is actually the best time to improve flexibility.
Not only that, but there are benefits to stretching on a soft surface, such as your bed, rather than the floor—in few words, it reduces the nervous feedback that limits your flexibility.
The most comfortable yoga session
Here are three great stretches to do of an evening:
Frog pose:
- Spread your knees wide, forming 90° angles at your ankles, knees, and hips.
- Press your hips downward and experiment with tilting your tailbone upwards.
- Hold for 1–3 minutes, breathing calmly.
Half straddle stretch:
- This stretch is done with one leg extended, and your other leg bent with foot against your inner thigh.
- Keep your lower back elongated while folding forward.
- Adjust the stretch’s focus by moving towards the middle or towards the extended leg, to stretch your inner thighs more or your hamstrings more, respectively.
- Hold for 1–2 minutes per leg.
Tabletop chest stretch:
- From a tabletop position, walk/slide your hands forward and drop your chest down.
- Hold for at least 1 minute, breathing deeply.
- Variations:
- Turn thumbs upward to engage side muscles.
- Cross arms to stretch the ribs.
Cross-legged forward fold:
- Start in a cross-legged seated position and slightly shift your hips backwards.
- Fold forward, allowing the spine to round.
- Hold for 1–3 minutes, breathing calmly.
This latter is especially good despite its simplicity, as it provides a deep stretch in the outer hips and lower back.
For more on all of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Over 50? Do These 3 Stretches Every Morning To Avoid Pain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pasteurization: What It Does And Doesn’t Do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pasteurization’s Effect On Risks & Nutrients
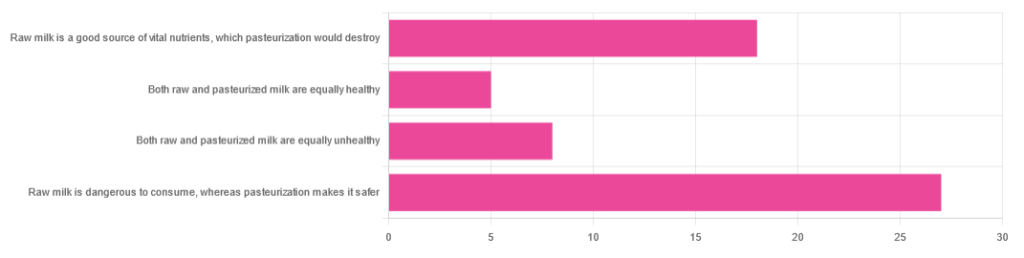
In Wednesday’s newsletter, we asked you for your health-related opinions of raw (cow’s) milk, and got the above-depicted, below-described, set of responses:
- About 47% said “raw milk is dangerous to consume, whereas pasteurization makes it safer”
- About 31% said “raw milk is a good source of vital nutrients which pasteurization would destroy”
- About 14% said “both raw milk and pasteurized milk are equally unhealthy”
- About 9% said “both raw milk and pasteurized milk are equally healthy”
Quite polarizing! So, what does the science say?
“Raw milk is dangerous to consume, whereas pasteurization makes it safer: True or False?”
True! Coincidentally, the 47% who voted for this are mirrored by the 47% of the general US population in a similar poll, deciding between the options of whether raw milk is less safe to drink (47%), just as safe to drink (15%), safer to drink (9%), or not sure (30%):
Public Fails to Appreciate Risk of Consuming Raw Milk, Survey Finds
As for what those risks are, by the way, unpasteurized dairy products are estimated to cause 840x more illness and 45x more hospitalizations than pasteurized products.
This is because unpasteurized milk can (and often does) contain E. coli, Listeria, Salmonella, Cryptosporidium, and other such unpleasantries, which pasteurization kills.
Source for both of the above claims:
(we know the title sounds vague, but all this information is easily visible in the abstract, specifically, the first two paragraphs)
Raw milk is a good source of vital nutrients which pasteurization would destroy: True or False?
False! Whether it’s a “good” source can be debated depending on other factors (e.g., if we considered milk’s inflammatory qualities against its positive nutritional content), but it’s undeniably a rich source. However, pasteurization doesn’t destroy or damage those nutrients.
Incidentally, in the same survey we linked up top, 16% of the general US public believed that pasteurization destroys nutrients, while 41% were not sure (and 43% knew that it doesn’t).
Note: for our confidence here, we are skipping over studies published by, for example, dairy farming lobbies and so forth. Those do agree, by the way, but nevertheless we like sources to be as unbiased as possible. The FDA, which is not completely unbiased, has produced a good list of references for this, about half of which we would consider biased, and half unbiased; the clue is generally in the journal names. For example, Food Chemistry and the Journal of Food Science and Journal of Nutrition are probably less biased than the International Dairy Association and the Journal of Dairy Science:
FDA | Raw Milk Misconceptions and the Danger of Raw Milk Consumption
this page covers a lot of other myths too, more than we have room to “bust” here, but it’s very interesting reading and we recommend to check it out!
Notably, we also weren’t able to find any refutation by counterexample on PubMed, with the very slight exception that some studies sometimes found that in the case of milks that were of low quality, pasteurization can reduce the vitamin E content while increasing the vitamin A content. For most milks however, no significant change was found, and in all cases we looked at, B-vitamins were comparable and vitamin D, popularly touted as a benefit of cow’s milk, is actually added later in any case. And, importantly, because this is a common argument, no change in lipid profiles appears to be findable either.
In science, when something has been well-studied and there aren’t clear refutations by counterexample, and the weight of evidence is clearly very much tipped into one camp, that usually means that camp has it right.
Milk generally is good/bad for the health: True or False?
True or False, depending on what we want to look at. It’s definitely not good for inflammation, but the whole it seems to be cancer-neutral and only increases heart disease risk very slightly:
- Keep Inflammation At Bay ← short version is milk is bad, fermented milk products are fine in moderation
- Is Dairy Scary? ← short version is that milk is neither good nor terrible; fermented dairy products however are health-positive in numerous ways when consumed in moderation
You may be wondering…
…how this goes for the safety of dairy products when it comes to the bird flu currently affecting dairy cows, so:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: