Native Americans Have Shorter Life Spans. Better Health Care Isn’t the Only Answer.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
HISLE, S.D. — Katherine Goodlow is only 20, but she has experienced enough to know that people around her are dying too young.
Goodlow, a member of the Lower Brule Sioux Tribe, said she’s lost six friends and acquaintances to suicide, two to car crashes, and one to appendicitis. Four of her relatives died in their 30s or 40s, from causes such as liver failure and covid-19, she said. And she recently lost a 1-year-old nephew.
“Most Native American kids and young people lose their friends at a young age,” said Goodlow, who is considering becoming a mental health therapist to help her community. “So, I’d say we’re basically used to it, but it hurts worse every time we lose someone.”
Native Americans tend to die much earlier than white Americans. Their median age at death was 14 years younger, according to an analysis of 2018-21 data from the Centers for Disease Control and Prevention
The disparity is even greater in Goodlow’s home state. Indigenous South Dakotans who died between 2017 and 2021 had a median age of 58 — 22 years younger than white South Dakotans, according to state data.
Donald Warne, a physician who is co-director of the Johns Hopkins Center for Indigenous Health and a member of the Oglala Sioux Tribe, can rattle off the most common medical conditions and accidents killing Native Americans.
But what’s ultimately behind this low life expectancy, agree Warne and many other experts on Indigenous health, are social and economic forces. They argue that in addition to bolstering medical care and fully funding the Indian Health Service — which provides health care to Native Americans — there needs to be a greater investment in case management, parenting classes, and home visits.
“It’s almost blasphemy for a physician to say,” but “the answer to addressing these things is not hiring more doctors and nurses,” Warne said. “The answer is having more community-based preventions.”
The Indian Health Service funds several kinds of these programs, including community health worker initiatives, and efforts to increase access to fresh produce and traditional foods.
Private insurers and state Medicaid programs, including South Dakota’s, are increasingly covering such services. But insurers don’t pay for all the services and aren’t reaching everyone who qualifies, according to Warne and the National Academy for State Health Policy.
Warne pointed to Family Spirit, a program developed by the Johns Hopkins center to improve health outcomes for Indigenous mothers and children.
Chelsea Randall, the director of maternal and child health at the Great Plains Tribal Leaders’ Health Board, said community health workers educate Native pregnant women and connect them with resources during home visits.
“We can be with them throughout their pregnancy and be supportive and be the advocate for them,” said Randall, whose organization runs Family Spirit programs across seven reservations in the Dakotas, and in Rapid City, South Dakota.
The community health workers help families until children turn 3, teaching parenting skills, family planning, drug abuse prevention, and stress management. They can also integrate the tribe’s culture by, for example, using their language or birthing traditions.
The health board funds Family Spirit through a grant from the federal Health Resources and Services Administration, Randall said. Community health workers, she said, use some of that money to provide child car seats and to teach parents how to properly install them to counter high rates of fatal crashes.
Other causes of early Native American deaths include homicide, drug overdoses, and chronic diseases, such as diabetes, Warne said. Native Americans also suffer a disproportionate number of infant and maternal deaths.
The crisis is evident in the obituaries from the Sioux Funeral Home, which mostly serves Lakota people from the Pine Ridge Reservation and surrounding area. The funeral home’s Facebook page posts obituaries for older adults, but also for many infants, toddlers, teenagers, young adults, and middle-aged residents.
Misty Merrival, who works at the funeral home, blames poor living conditions. Some community members struggle to find healthy food or afford heat in the winter, she said. They may live in homes with broken windows or that are crowded with extended family members. Some neighborhoods are strewn with trash, including intravenous needles and broken bottles.
Seeing all these premature deaths has inspired Merrival to keep herself and her teenage daughter healthy by abstaining from drugs and driving safely. They also talk every day about how they’re feeling, as a suicide-prevention strategy.
“We’ve made a promise to each other that we wouldn’t leave each other like that,” Merrival said.
Many Native Americans live in small towns or on poor, rural reservations. But rurality alone doesn’t explain the gap in life expectancy. For example, white people in rural Montana live 17 years longer, on average, than Native Americans in the state, according to state data reported by Lee Enterprises newspapers.
Many Indigenous people also face racism or personal trauma from child or sexual abuse and exposure to drugs or violence, Warne said. Some also deal with generational trauma from government programs and policies that broke up families and tried to suppress Native American culture.
Even when programs are available, they’re not always accessible.
Families without strong internet connections can’t easily make video appointments. Some lack cars or gas money to travel to clinics, and public transportation options are limited.
Randall, the health board official, is pregnant and facing her own transportation struggles.
It’s a three-hour round trip between her home in the town of Pine Ridge and her prenatal appointments in Rapid City. Randall has had to cancel several appointments when family members couldn’t lend their cars.
Goodlow, the 20-year-old who has lost several loved ones, lives with seven other people in her mother’s two-bedroom house along a gravel road. Their tiny community on the Pine Ridge Reservation has homes and ranches but no stores.
Goodlow attended several suicide-prevention presentations in high school. But the programs haven’t stopped the deaths. One friend recently killed herself after enduring the losses of her son, mother, best friend, and a niece and nephew.
A month later, another friend died from a burst appendix at age 17, Goodlow said. The next day, Goodlow woke up to find one of her grandmother’s parakeets had died. That afternoon, she watched one of her dogs die after having seizures.
“I thought it was like some sign,” Goodlow said. “I started crying and then I started thinking, ‘Why is this happening to me?’”
Warne said the overall conditions on some reservations can create despair. But those same reservations, including Pine Ridge, also contain flourishing art scenes and language and cultural revitalization programs. And not all Native American communities are poor.
Warne said federal, state, and tribal governments need to work together to improve life expectancy. He encourages tribes to negotiate contracts allowing them to manage their own health care facilities with federal dollars because that can open funding streams not available to the Indian Health Service.
Katrina Fuller is the health director at Siċaŋġu Co, a nonprofit group on the Rosebud Reservation in South Dakota. Fuller, a member of the Rosebud Sioux Tribe, said the organization works toward “wicozani,” or the good way of life, which encompasses the physical, emotional, cultural, and financial health of the community.
Siċaŋġu Co programs include bison restoration, youth development, a Lakota language immersion school, financial education, and food sovereignty initiatives.
“Some people out here that are struggling, they have dreams, too. They just need the resources, the training, even the moral support,” Fuller said. “I had one person in our health coaching class tell me they just really needed someone to believe in them, that they could do it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Managing Chronic Pain (Realistically!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Realistic chronic pain management
We’ve had a number of requests to do a main feature on managing chronic pain, so here it is!
A quick (but important) note before we begin:
Obviously, not all chronic pain is created equal. Furthermore, we know that you, dear reader with chronic pain, have been managing yours for however long you have, learning as you go. You also doubtlessly know your individual condition inside out.
We also know that people with chronic health conditions in general are constantly beset by well-meaning unsolicited advice from friends and family, asking if you’ve heard about [thing you heard about 20 years ago] that will surely change your life and cure you overnight.
It’s frustrating, and we’re going to try to avoid doing that here, while still offering the advice that was asked for. We ask you, therefore, to kindly overlook whatever you already knew, and if you already knew it all, well, we salute you and will not be surprised if that’s the case for at least some readers. Chronic pain’s a… Well, it’s a chronic pain.
All that said, let’s dive in…
How are you treating your body right now?
Are you hydrated; have you eaten; are you standing/sitting/lying in a position that at least should be comfortable for you in principle?
The first two things affect pain perception; the latter can throw a spanner in the works if something’s not quite right.
Move your body (gently!)
You know your abilities, so think about the range of motion that you have, especially in the parts of your body that hurt (if that’s “everywhere”, then, our sympathies, and we hope you find the same advice applies). Think about your specific muscles and joints as applicable, and what the range of motion is “supposed” to be for each. Exercise your range of motion as best you can (gently!) to the point of its limit(s) and/or pain.
- If you take it past that limit, there is a good chance you will make it worse. You don’t want that.
- If you don’t take it to the limit, there is a good chance your range of movement will deteriorate, and your “safe zone” (i.e., body positions that are relatively free from pain) will diminish. You definitely don’t want that, either.
Again, moderation is key. Yes, annoying as the suggestion may be, such things as yoga etc can help, if done carefully and gently. You know your limits; work with those, get rest between, and do what you can.
For most people this will at least help keep the pain from getting worse.
Hot & Cold
Both of these things could ease your pain… Or make it worse. There is an element of “try it and see”, but here’s a good general guide:
Here’s How to Choose Between Using Ice or Heat for Pain
Meditation… Or Distraction
Meditating really does help a lot of people. In the case of pain, it can be counterintuitively helpful to focus for a while on the sensation of the pain… But in a calm, detached fashion. Without judgement.
“Yes, I am experiencing pain. Yes, it feels like I’m being stabbed with hot knives. Yes, this is tortuous; wow, I feel miserable. This truly sucks.”
…it doesn’t sound like a good experience, does it? And it’s not, but paying it attention this way can paradoxically help ease things. Pain is, after all, a messenger. And in the case of chronic pain, it’s in some ways a broken messenger, but what a messenger most needs is to be heard.
The above approach a) is good b) may have a limit in how long you can sustain it at a time, though. So…
The opposite is a can be a good (again, short-term) approach too. Call a friend, watch your favorite movie, play a video game if that’s your thing. It won’t cure anything, but it can give you a little respite.
Massage
Unless you already know this makes your pain worse, this is a good thing to try. It doesn’t have to be a fancy spa; if the nature of your pain and condition permits, you can do self-massage. If you have a partner or close friend who can commit to helping, it can be very worth them learning to give a good massage. There are often local courses available, and failing that, there is also YouTube.
Here’s an example of a good video for myofascial release massage, which can ease a lot of common kinds of chronic pain:
Some quick final things to remember:
- If you find something helps, then it helps, do that.
- That goes for mobility aids and other disability aids too, even if it was designed for a different disability. If it helps, it helps. You’re not stealing anyone’s thunder (or resources) by using something that makes your life easier. We’re not in this life to suffer!
- There is no such thing as “this pain is not too much”. The correct amount of pain is zero. Maybe your body won’t let you reach zero, but more than that is “too much” already.
- You don’t have to be suffering off the scale to deserve relief from pain
Share This Post
-
Total Recovery – by Dr. Gary Kaplan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, know: Dr. Kaplan is an osteopath, and as such, will be mostly approaching things from that angle. That said, he is also board certified in other things too, including family medicine, so he’s by no means a “one-trick pony”, nor are there “when your only tool is a hammer, everything starts to look like a nail” problems to be found here. Instead, the scope of the book is quite broad.
Dr. Kaplan talks us through the diagnostic process that a doctor goes through when presented with a patient, what questions need to be asked and answered—and by this we mean the deeper technical questions, e.g. “what do these symptoms have in common”, and “what mechanism was at work when the pain become chronic”, not the very basic questions asked in the initial debriefing with the patient.
He also asks such questions (and questions like these get chapters devoted to them) as “what if physical traumas build up”, and “what if physical and emotional pain influence each other”, and then examines how to interrupt the vicious cycles that lead to deterioration of one’s condition.
The style of the book is very pop-science and often narrative in its presentation, giving lots of anecdotes to illustrate the principles. It’s a “sit down and read it cover-to-cover” book—or a chapter a day, whatever your preferred pace; the point is, it’s not a “dip directly to the part that answers your immediate question” book; it’s not a textbook or manual.
Bottom line: a lot of this work is about prompting the reader to ask the right questions to get to where we need to be, but there are many illustrative possible conclusions and practical advices to be found and given too, making this a useful read if you and/or a loved one suffers from chronic pain.
Click here to check out Total Recovery, and solve your own mysteries!
Share This Post
-
Exercise and Fat Loss (5 Things You Need To Know)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to think “I’ll eat whatever; I can always burn it off later”, and if it’s an odd occasion, then that’s fine; indeed, a fit and healthy body can usually weather small infrequent dietary indiscretions easily. But…
You can’t outrun a bad diet
Exercise can create a calorie deficit, but over time, the body balances this out by adjusting one’s metabolism, leading to a plateau in fat loss—and as you might know, you can’t out-exercise a bad diet. On the contrary, dietary adjustments are crucial for fat loss and body recomposition.
About that calorie deficit in the first place, by the way: extreme calorie deficits through exercise alone can lead to muscle loss, reduced energy, and thus sabotage long-term fat loss because having muscle mass increases one’s base metabolic rate (while having fat does not).
Another thing to bear in mind about exercise is that longer workouts without adequate rests in between can cause burnout, injury, or weight gain due to the body doing its best to conserve energy.
So, a good diet is a necessary condition for both muscle maintenance and fat loss.
Five Key Diet Tips:
- Include foods you love: don’t feel obliged cut out favorite foods that are a little unhealthy; incorporate them in moderation for sustainability.
- Keep adjustments small: avoid making drastic dietary changes all at once; make gradual tweaks to prevent feeling deprived.
- Prioritize protein: focus on including a protein source in every meal to increase satiety and aid in muscle building.
- Avoid low-calorie diets: drastically cutting calories can lead to muscle loss, metabolic adaptation, and overeating.
- Embrace diet evolution: changes may not feel sustainable at first, but adjustments over time help achieve long-term balance. You can always “adjust course” as you go.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Are You A Calorie-Burning Machine?
Take care!
Share This Post
Related Posts
-
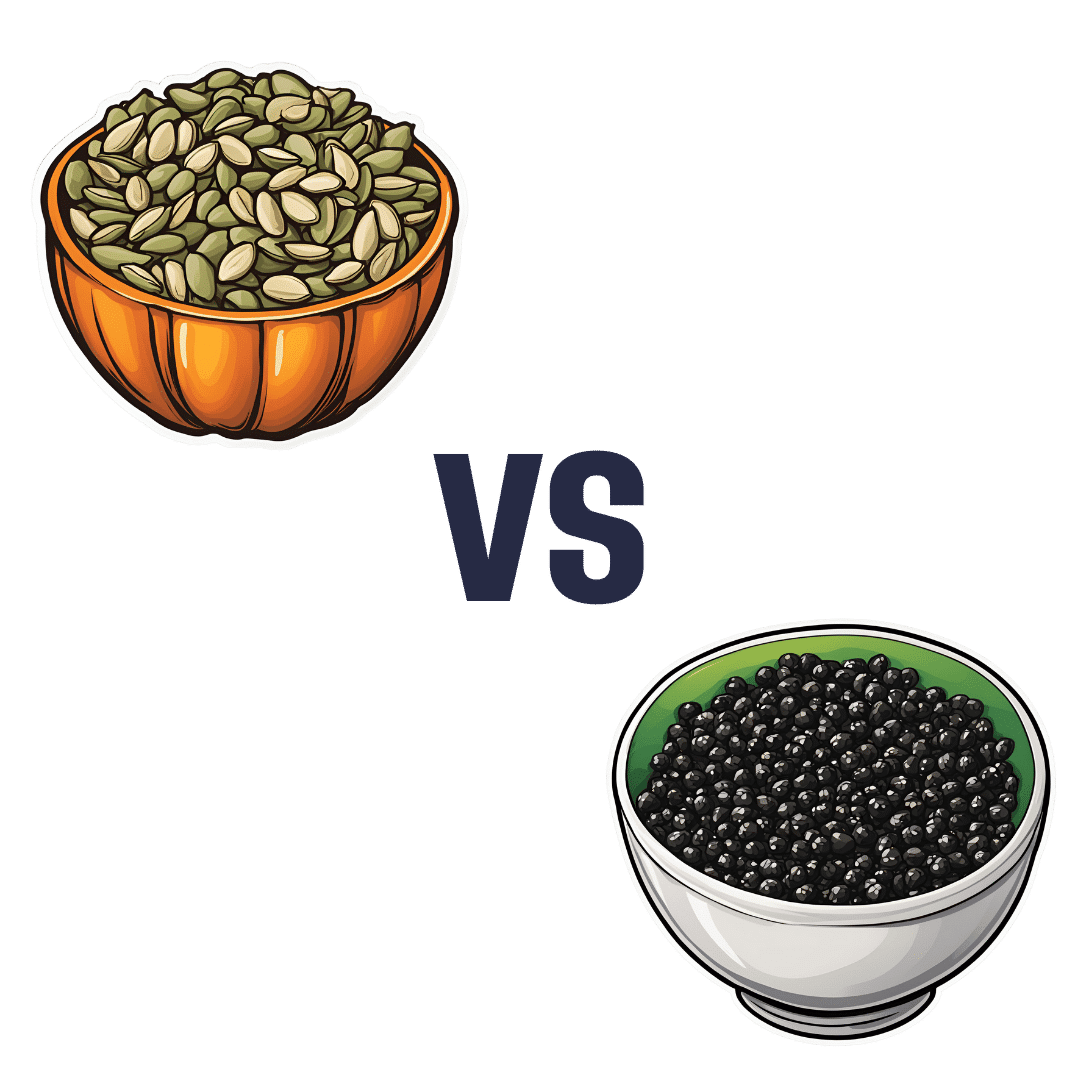
Pumpkin Seeds vs Watermelon Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pumpkin seeds to watermelon seeds, we picked the watermelon.
Why?
Starting with the macros: pumpkin seeds have a lot more carbs, while watermelon seeds have a lot more protein, despite pumpkin seeds being famous for such. They’re about equal on fiber. In terms of fats, watermelon seeds are higher in fats, and yes, these are healthy fats, mostly polyunsaturated.
When it comes to vitamins, pumpkin seeds are marginally higher in vitamins A and C, while watermelon seeds are a lot higher in vitamins B1, B2, B3, B5, B6, and B9. An easy win for watermelon seeds here.
In the category of minerals, despite being famous for zinc, pumpkin seeds are higher only in potassium, while watermelon seeds are higher in iron, magnesium, manganese, and phosphorus; the two seeds are equal on calcium, copper, and zinc. Another win for watermelon seeds.
In short, enjoy both, but watermelon has more to offer. Of course, if buying just the seeds and not the whole fruit, it’s generally easier to find pumpkin seeds than watermelon seeds, so do bear in mind that pumpkin seeds’ second place isn’t that bad here—it’s just a case of a very nutritious food looking bad by standing next to an even better one.
Want to learn more?
You might like to read:
Seed Saving Secrets – by Alice Mirren
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Plums vs Strawberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing plums to strawberries, we picked the strawberries.
Why?
Both are great! Absolutely top-tier fruits. However, even within the top tier, there are distinctions:
In terms of of macros, plums have more carbs while strawberries have more fiber; we’ll take the extra fiber for the win here.
In the category of vitamins, plums have more of vitamins A, B1, B2, and K, while strawberries have more of vitamins B6, B9, C, E, and choline, thus scoring a marginal win for strawberries in this round.
When it comes to minerals, plums have (slightly) more copper, while strawberries have more calcium, iron, magnesium, manganese, phosphorus, selenium, and zinc. One more win for strawberries.
In terms of phytochemicals, plums have a higher total mass of polyphenols, and so win this round, although strawberries scored well too.
Adding up the sections makes for an overall win for strawberries, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is thunderstorm asthma becoming more common?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When spring arrives, so do warnings about thunderstorm asthma. But a decade ago, most of us hadn’t heard of it.
So where did thunderstorm asthma come from? Is it a new phenomenon?
In 2016, the world’s most catastrophic thunderstorm asthma event took Melbourne by surprise. An increase in warnings and monitoring is partly a response to this.
But there are also signs climate change may be exacerbating the likelihood of thunderstorm asthma, with more extreme weather, extended pollen seasons and a rise in Australians reporting hay fever.
A landmark catastrophe
The first time many Australians heard of thunderstorm asthma was in November 2016, when a major event rocked Melbourne.
During a late night storm, an estimated 10,000 people were rushed to hospitals with severe asthma attacks. With thousands of calls on emergency lines, ambulances and emergency departments were unprepared to handle the rapid increase in people needing urgent medical care. Tragically, ten of those people died.
This was the most catastrophic thunderstorm asthma event in recorded history and the first time deaths have ever occurred anywhere in the world.
In response, the Victorian Department of Health implemented initiatives, including public awareness campaigns and improvements to health and emergency services, to be ready for future thunderstorm asthma events.
A network of pollen monitoring stations was also set up across the state to gather data that helps to predict future events.
A problem for decades
While this event was unexpected, it wasn’t the first time we’d had thunderstorm asthma in Australia – we’ve actually known about it for decades.
Melbourne reported its first instance of thunderstorm asthma back in 1984, only a year after this phenomenon was first discovered in Birmingham in the United Kingdom.
Thunderstorm asthma has since been reported in other parts of Australia, including Canberra and New South Wales. But it is still most common in Melbourne. Compared to any other city (or country) the gap is significant: over a quarter of all known events worldwide have occurred in Melbourne.
Why Melbourne?
Melbourne’s location makes it a hotspot for these kinds of events. Winds coming from the north of Melbourne tend to be dry and hot as they come from deserts in the centre of Australia, while winds from the south are cooler as they come from the ocean.
When hot and cool air mix above Melbourne, it creates the perfect conditions for thunderstorms to form.
Northern winds also blow a lot of pollen from farmlands into the city, in particular grass pollen. This is not only the most common cause of seasonal hay fever in Melbourne but also a major trigger of thunderstorm asthma.
Why grass pollen?
There’s a particular reason grass pollen is the main culprit behind thunderstorm asthma in Australia. During storms there is a lot of moisture in the air. Grass pollen will absorb this moisture, making it swell up like a water balloon.
If pollen absorbs too much water whilst airborne, it can burst or “rupture,” releasing hundreds of microscopic particles into the air that can be swept by powerful winds.
Normally, when you breathe in pollen it gets stuck in your upper airway – for example, your nose and throat. This is what causes typical hay fever symptoms such as sneezing or runny nose.
But the microscopic particles released from ruptured grass pollen are much smaller and don’t get stuck as easily in the upper airway. Instead, they can travel deep into your airways until they reach your lungs. This may trigger more severe symptoms, such as wheezing or difficulty breathing, even in people with no prior history of asthma.
So who is at risk?
You might think asthma is the biggest risk factor for thunderstorm asthma. In fact, the biggest risk factor is hay fever.
Up to 99% of patients who went to the emergency department during the Melbourne 2016 event had hay fever, while a majority (60%) had no prior diagnosis of asthma.
Every single person hospitalised was allergic to at least one type of grass pollen. All had a sensitivity to ryegrass.
Is thunderstorm asthma becoming more common?
Thunderstorm asthma events are rare, with just 26 events officially recorded worldwide.
However there is evidence these events could become more frequent and severe in coming years, due to climate change. Higher temperatures and pollution could be making plants produce more pollen and pollen seasons last much longer.
Extreme weather events, including thunderstorms, are also expected to become more common and severe.
In addition, there are signs rates that hay fever may be increasing. The number of Australians reporting allergy symptoms have risen from 15% in 2008 to 24% in 2022. Similar trends in other countries has been linked to climate change.
How can I prepare?
Here are three ways you can reduce your risk of thunderstorm asthma:
- stock up on allergy medication and set up an asthma action plan with your GP
- check daily pollen forecasts for the estimated pollen level and risk of a thunderstorm asthma event in your local area
- on days with high pollen or a high risk of thunderstorm asthma, spend less time outside or wear a surgical face mask to reduce your symptoms.
Kira Morgan Hughes, PhD Candidate in Allergy and Asthma, School of Life and Environmental Sciences, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: