How to Stay Sane – by Philippa Perry
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is not: a guide of “how to stay sane” in the popular use of the word “sane”, meaning free from serious mental illness of all and any kinds in general, and especially free from psychotic delusions. Alas, this book will not help with those.
What, then, is it? A guide of “how to stay sane” in the more casual sense of resiliently and adaptively managing stress, anxiety, and suchlike. The “light end” of mental health struggles, that nonetheless may not always feel light when dealing with them.
The author, a psychotherapist, draws from her professional experience and training to lay out psychological tools for our use, as well as giving the reader a broader understanding of the most common ills that may ail us.
The writing style is relaxed and personable; it’s not at all like reading a textbook.
The psychotherapeutic style is not tied to one model, and rather hops from one to another, per what is most likely to help for a given thing. This is, in this reviewer’s opinion at least, far better than the (all-too common) attempt made by a lot of writers to try to present their personal favorite model as the cure for all ills, instead of embracing the whole toolbox as this one does.
Bottom line: if your mental health is anywhere between “mostly good” and “a little frayed around the edges but hanging on by at least a few threads”, then this book likely can help you gain/maintain the surer foundation you’re surely seeking.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Who Initiates Sex & Why It Matters
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In an ideal world, it wouldn’t matter any more than who first says “let’s get something to eat” when hungry. But in reality, it can cause serious problems on both sides:
Fear and loathing?
The person who initiates gets the special prize of an n% chance of experiencing rejection, and then what? Try again, and again, and risk seeming pushy? Or leave the ball in the other person’s court, where it may then go untouched for the next few months, because (in the most positive scenario) they were waiting for you to initiate at a better time for them?
The person who does not initiate, and/but does not want sex at that time, gets the special prize of either making their partner feel unwanted, insecure, and perhaps unloved, or else grudgingly consenting to sex that’s going to be no fun while your heart’s not in it, and thus create the same end result plus you had an extra bad experience?
So, that sucks all around:
- Initiating touch (sex or cuddling) can feel like a test of being wanted, whereupon a lack of initiation or response may be misinterpreted as a lack of love or appreciation.
- Meanwhile, non-reciprocation might stem from exhaustion or unrelated issues. For many, it’s a physiological lottery.
10almonds note: not discussed in this video, but for many couples, problems can also arise because one partner or another just isn’t showing up with the expected physical signs of physiological arousal, so even if they say (and mean!) an enthusiastic “yes”, their body’s signs get misread as a “not really, though”, resulting in one partner feeling rejected, and both feeling inadequate—on account of something that was completely unrelated to how the person actually felt about the prospect of sex*.
*Sometimes, physiological arousal will simply not accompany psychological arousal, no matter how sincere the latter. And on the flipside, sometimes the signs of physiological arousal will just show up without psychological arousal. The human body is just like that sometimes. We all must listen to our partners’ words, not their genitals!
The solution to this problem is thus the same as the solution to the rest of the problem that is discussed in the video, and it’s: good communication.
That can be easier said than done, of course—not everyone is at their most eloquent in such situations! Which is why it can be important to have those conversations first outside of the bedroom when the stakes are low/non-existent.
Even with the best communication, a more general, overarching non-reciprocity (real or perceived) of sexual desire can cause bitterness, resentment, and can ultimately be relationship-ending if a resolution that’s acceptable to everyone involved is not found.
Ultimately, the work as a couple must begin from within as individuals—addressing self-worth issues to better navigate love and intimacy.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Relationships: When To Stick It Out & When To Call It Quits
Take care!
Share This Post
-
Evidence doesn’t support spinal cord stimulators for chronic back pain – and they could cause harm
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In an episode of ABC’s Four Corners this week, the use of spinal cord stimulators for chronic back pain was brought into question.
Spinal cord stimulators are devices implanted surgically which deliver electric impulses directly to the spinal cord. They’ve been used to treat people with chronic pain since the 1960s.
Their design has changed significantly over time. Early models required an external generator and invasive surgery to implant them. Current devices are fully implantable, rechargeable and can deliver a variety of electrical signals.
However, despite their long history, rigorous experimental research to test the effectiveness of spinal cord stimulators has only been conducted this century. The findings don’t support their use for treating chronic pain. In fact, data points to a significant risk of harm.
What does the evidence say?
One of the first studies used to support the effectiveness of spinal cord stimulators was published in 2005. This study looked at patients who didn’t get relief from initial spinal surgery and compared implantation of a spinal cord stimulator to a repeat of the spinal surgery.
Although it found spinal cord stimulation was the more effective intervention for chronic back pain, the fact this study compared the device to something that had already failed once is an obvious limitation.
Later studies provided more useful evidence. They compared spinal cord stimulation to non-surgical treatments or placebo devices (for example, deactivated spinal cord stimulators).
A 2023 Cochrane review of the published comparative studies found nearly all studies were restricted to short-term outcomes (weeks). And while some studies appeared to show better pain relief with active spinal cord stimulation, the benefits were small, and the evidence was uncertain.
Only one high-quality study compared spinal cord stimulation to placebo up to six months, and it showed no benefit. The review concluded the data doesn’t support the use of spinal cord stimulation for people with back pain.
What about the harms?
The experimental studies often had small numbers of participants, making any estimate of the harms of spinal cord stimulation difficult. So we need to look to other sources.
A review of adverse events reported to Australia’s Therapeutic Goods Administration found the harms can be serious. Of the 520 events reported between 2012 and 2019, 79% were considered “severe” and 13% were “life threatening”.
We don’t know exactly how many spinal cord stimulators were implanted during this period, however this surgery is done reasonably widely in Australia, particularly in the private and workers compensation sectors. In 2023, health insurance data showed more than 1,300 spinal cord stimulator procedures were carried out around the country.
In the review, around half the reported harms were due to a malfunction of the device itself (for example, fracture of the electrical lead, or the lead moved to the wrong spot in the body). The other half involved declines in people’s health such as unexplained increased pain, infection, and tears in the lining around the spinal cord.
More than 80% of the harms required at least one surgery to correct the problem. The same study reported four out of every ten spinal cord stimulators implanted were being removed.
Chronic back pain can be debilitating. CGN089/Shutterstock High costs
The cost here is considerable, with the devices alone costing tens of thousands of dollars. Adding associated hospital and medical costs, the total cost for a single procedure averages more than $A50,000. With many patients undergoing multiple repeat procedures, it’s not unusual for costs to be measured in hundreds of thousands of dollars.
Rebates from Medicare, private health funds and other insurance schemes may go towards this total, along with out-of-pocket contributions.
Insurers are uncertain of the effectiveness of spinal cord stimulators, but because their implantation is listed on the Medicare Benefits Schedule and the devices are approved for reimbursement by the government, insurers are forced to fund their use.
Industry influence
If the evidence suggests no sustained benefit over placebo, the harms are significant and the cost is high, why are spinal cord stimulators being used so commonly in Australia? In New Zealand, for example, the devices are rarely used.
Doctors who implant spinal cord stimulators in Australia are well remunerated and funding arrangements are different in New Zealand. But the main reason behind the lack of use in New Zealand is because pain specialists there are not convinced of their effectiveness.
In Australia and elsewhere, the use of spinal cord stimulators is heavily promoted by the pain specialists who implant them, and the device manufacturers, often in unison. The tactics used by the spinal cord stimulator device industry to protect profits have been compared to tactics used by the tobacco industry.
A 2023 paper describes these tactics which include flooding the scientific literature with industry-funded research, undermining unfavourable independent research, and attacking the credibility of those who raise concerns about the devices.
It’s not all bad news
Many who suffer from chronic pain may feel disillusioned after watching the Four Corners report. But it’s not all bad news. Australia happens to be home to some of the world’s top back pain researchers who are working on safe, effective therapies.
New approaches such as sensorimotor retraining, which includes reassurance and encouragement to increase patients’ activity levels, cognitive functional therapy, which targets unhelpful pain-related thinking and behaviour, and old approaches such as exercise, have recently shown benefits in robust clinical research.
If we were to remove funding for expensive, harmful and ineffective treatments, more funding could be directed towards effective ones.
Ian Harris, Professor of Orthopaedic Surgery, UNSW Sydney; Adrian C Traeger, Research Fellow, Institute for Musculoskeletal Health, University of Sydney, and Caitlin Jones, Postdoctoral Research Associate in Musculoskeletal Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Aging For Beginners – by Ezra Bayda & Elizabeth Hamilton
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one’s not about how to avoid aging, but rather, how to be at peace with whatever aging may be happening, perhaps despite our best efforts.
The book is dedicated:
❝To all the starving and suffering children throughout the world, with the wish that they may someday have the opportunity to experience the life of a contented geriatric❞
It’s a stark reminder that old age is a privilege that many do not get to enjoy, thanks to poverty, disease, wars, and accidents and incidents along the way.
So, how to go about making the very most of what we have, for those of us who are perhaps going gray in a comfortable, safe environment?
The answer may surprise you: the authors tackle things head-on without dressing old age up in euphemisms or platitudes—they cover not just the physical decline that typically occurs eventually, but also the impact of the physical pain that this may bring, the way this may play into loneliness and helplessness, and perhaps anxiety and/or depression. And, of course, the topic of grief and loss, that for most of us becomes all the more part of our lives as we get older. For that matter, our own mortality is also something the authors come back to from start to finish.
Thus, this is not necessarily a cheerful book—but it gives the tools such that we can be cheerful about life in general, in the face of all the aforementioned things, without pretending that things that are not good are good, just, making our peace with what is, and making the most out of what we have.
The authors are Zen teachers with decades of experience, and this book is heavily influenced by Zen principles. And yes, it does teach meditation too, but that’s just one tool in the toolbox.
The style is deep and yet very readable, heavy of tone and at the same time inspiring of lightness of heart.
Bottom line: if you’d like to worry less about aging (while still doing all you want to stay young), this book can certainly help with that.
Click here to check out Aging For Beginners, and be at peace with yourself.
Share This Post
Related Posts
-
You’re Not Forgetful: How To Remember Everything
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Elizabeth Filips, medical student busy learning a lot of information, explains how in today’s video:
Active processing
An important thing to keep in mind is that forgetting is an active process, not passive as once believed. It has its own neurotransmitters and pathways, and as such, to improve memory, it’s essential to understand and manage forgetting.
So, how does forgetting occur? Memories are stored with cues or tags, which help retrieve information. However, overloading cues with too much information can cause “transient forgetting”—that is to say, the information is still in there somewhere; you just don’t have the filing system required to retrieve the data. This is the kind of thing that you will try hard to remember at some point in the day when you need it, fail, and then wake up at 3am with an “Aha!” because your brain finally found what you were looking for. So, to avoid that, use unique and strong cues to help improve recall (mnemonics are good for this, as are conceptual anchors).
While memory does not appear to actually be finite, there is some practical truth in the “finite storage” model insofar as learning new information can overwrite previous knowledge, iff your brain mistakes it for an update rather than addition. So for that reason, it’s good to periodically go over old information—in psychology this is called rehearsal, which may conjure theatrical images, but it can be as simple as mentally repeating a phone number, a mnemonic, or visually remembering a route one used to take to go somewhere.
Self-perception affects memory performance. Negative beliefs about one’s memory can worsen performance (so don’t say “I have a bad memory”, even to yourself, and in contrast, find more positive affirmations to make about your memory), and mental health in general plays a significant role in memory. For example, if you have ever had an extended period of depression, then chances are good you have some huge gaps in your memory for that time in your life.
A lot of what we learned in school was wrong—especially what we learned about learning. Traditional (vertical) learning is harder to retain, whereas horizontal learning (connecting topics through shared characteristics) creates stronger, interconnected memories. In short, your memories should tell contextual stories, not be isolated points of data.
Embarking on a new course of study? Yes? (If not, then why not? Pick something!)
It may be difficult at first, but experts memorize things more quickly due to built-up intuition in their field. For example a chess master can glance at a chess board for about 5 seconds and memorize the position—but only if the position is one that could reasonably arise in a game; if the pieces are just placed at random, then their memorization ability plummets to that of the average person, because their expertise has been nullified.
What this means in practical terms: building a “skeleton” framework before learning can enhance memorization through logical connections. For this reason, if embarking on a serious course of study, getting a good initial overview when you start is critical, so that you have a context for the rest of what you learn to go into. For example, let’s say you want to learn a language; if you first quickly do a very basic bare-bones course, such as from Duolingo or similar, then even though you’ll have a very small vocabulary and a modest grasp of grammar and make many mistakes and have a lot of holes in your knowledge, you now have somewhere to “fit” every new word or idea you learn. Same goes for other fields of study; for example, a doctor can be told about a new drug and remember everything about it immediately, because they understand the systems it interacts with, understand how it does what it does, and can compare it mentally to similar drugs, and they thus have a “place” in that overall system for the drug information to reside. But for someone who knows nothing about medicine, it’s just a lot of big words with no meaning. So: framework first, details later.
For more on all this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Boost Your Memory Immediately (Without Supplements)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Read a Book – by Mortimer J. Adler and Charles Van Doren
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are you a cover-to-cover person, or a dip-in-and-out person?
Mortimer Adler and Charles van Doren have made a science out of getting the most from reading books.
They help you find what you’re looking for (Maybe you want to find a better understanding of PCOS… maybe you want to find the definition of “heuristics”… maybe you want to find a new business strategy… maybe you want to find a romantic escape… maybe you want to find a deeper appreciation of 19th century poetry, maybe you want to find… etc).
They then help you retain what you read, and make sure that you don’t miss a trick.
Whether you read books so often that optimizing this is of huge value for you, or so rarely that when you do, you want to make it count, this book could make a real difference to your reading experience forever after.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is Cutting Calories The Key To Healthy Long Life?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Caloric Restriction with Optimal Nutrition
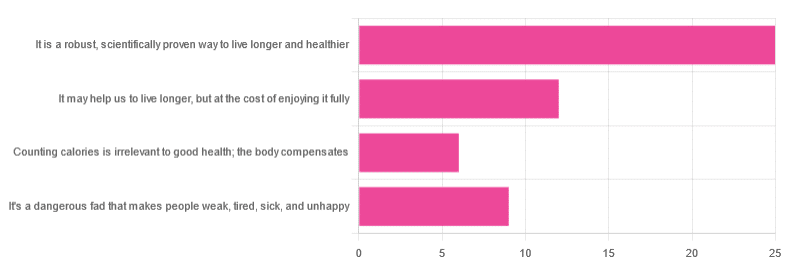
Yesterday, we asked you “What is your opinion of caloric restriction as a health practice?” and got the above-depicted, below-described spread of responses:
- 48% said “It is a robust, scientifically proven way to live longer and healthier”
- 23% said “It may help us to live longer, but at the cost of enjoying it fully”
- 17% said “It’s a dangerous fad that makes people weak, tired, sick, and unhealthy”
- 12% said “Counting calories is irrelevant to good health; the body compensates”
So… What does the science say?
A note on terms, first
“Caloric restriction” (henceforth: CR), as a term, sees scientific use to mean anything from a 25% reduction to a 50% reduction, compared to metabolic base rate.
This can also be expressed the other way around, “dropping to 60% of the metabolic base rate” (i.e., a 40% reduction).
Here we don’t have the space to go into much depth, so our policy will be: if research papers consider it CR, then so will we.
A quick spoiler, first
The above statements about CR are all to at least some degree True in one way or another.
However, there are very important distinctions, so let’s press on…
CR is a robust, scientifically proven way to live longer and healthier: True or False?
True! This has been well-studied and well-documented. There’s more science for this than we could possibly list here, but here’s a good starting point:
❝Calorie restriction (CR), a nutritional intervention of reduced energy intake but with adequate nutrition, has been shown to extend healthspan and lifespan in rodent and primate models.
Accumulating data from observational and randomized clinical trials indicate that CR in humans results in some of the same metabolic and molecular adaptations that have been shown to improve health and retard the accumulation of molecular damage in animal models of longevity.
In particular, moderate CR in humans ameliorates multiple metabolic and hormonal factors that are implicated in the pathogenesis of type 2 diabetes, cardiovascular diseases, and cancer, the leading causes of morbidity, disability and mortality❞
Source: Ageing Research Reviews | Calorie restriction in humans: an update
See also: Caloric restriction in humans reveals immunometabolic regulators of health span
We could devote a whole article (or a whole book, really) to this, but the super-short version is that it lowers the metabolic “tax” on the body and allows the body to function better for longer.
CR may help us to live longer, but at the cost of enjoying it fully: True or False?
True or False, contingently, depending on what’s important to you. And that depends on psychology as much as physiology, but it’s worth noting that there is often a selection bias in the research papers; people ill-suited to CR drop out of the studies and are not counted in the final data.
Also, relevant for a lot of our readers, most (human-based) studies recruit people over 18 and under 60. So while it is reasonable to assume the same benefits will be carried over that age, there is not nearly as much data for it.
Studies into CR and Health-Related Quality of Life (HRQoL) have been promising, and/but have caveats:
❝In non-obese adults, CR had some positive effects and no negative effects on HRQoL.❞
❝We do not know what degree of CR is needed to achieve improvements in HRQoL, but we do know it requires an extraordinary amount of support.
Therefore, the incentive to offer this intervention to a low-risk, normal or overweight individual is lacking and likely not sustainable in practice.❞
CR a dangerous fad that makes people weak, tired, sick, and unhealthy: True or False?
True if it is undertaken improperly, and/or without sufficient support. Many people will try CR and forget that the idea is to reduce metabolic load while still getting good nutrition, and focus solely on the calorie-counting.
So for example, if a person “saves” their calories for the day to have a night out in a bar where they drink their calories as alcohol, then this is going to be abysmal for their health.
That’s an extreme example, but lesser versions are seen a lot. If you save your calories for a pizza instead of a night of alcoholic drinks, then it’s not quite so woeful, but for example the nutrition-to-calorie ratio of pizza is typically not great. Multiply that by doing it as often as not, and yes, someone’s health is going to be in ruins quite soon.
Counting calories is irrelevant to good health; the body compensates: True or False?
True if by “good health” you mean weight loss—which is rarely, if ever, what we mean by “good health” here at 10almonds (unless we clarify such), but it’s a very common association and indeed, for some people it’s a health goal. You cannot sustainably and healthily lose weight by CR alone, especially if you’re not getting optimal nutrition.
Your body will notice that you are starving, and try to save you by storing as much fat as it can, amongst other measures that will similarly backfire (cortisol running high, energy running low, etc).
For short term weight loss though, yes, it’ll work. At a cost. That we don’t recommend.
❝By itself, decreasing calorie intake will have a limited short-term influence.❞
Source: Reducing Calorie Intake May Not Help You Lose Body Weight
See also…
❝Caloric restriction is a commonly recommended weight-loss method, yet it may result in short-term weight loss and subsequent weight regain, known as “weight cycling”, which has recently been shown to be associated with both poor sleep and worse cardiovascular health❞
Source: Dieting Behavior Characterized by Caloric Restriction
In summary…
Caloric restriction is a well-studied area of health science. We know:
- Practised well, it can extend not only lifespan, but also healthspan
- Practised well, it can improve mood, energy, sexual function, and the other things people fear losing
- Practised badly, it can be ruinous to the health—it is critical to practise caloric restriction with optimal nutrition.
- Practised badly, it can lead to unhealthy weight loss and weight regain
One final note…
If you’ve tried CR and hated it, and you practised it well (e.g., with optimal nutrition), then we recommend just not doing it.
You could also try intermittent fasting instead, for similar potential benefits. If that doesn’t work out either, then don’t do that either!
Sometimes, we’re just weird. It can often be because of a genetic or epigenetic quirk. There are usually workarounds, and/but not everything that’s right for most people will be right for all of us.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: