Fruit & Veg In The Fridge: Pros & Cons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝What effect does refrigeration have on the nutritional value of fruit and vegetables??❞
It’s difficult to give a single definitive answer, because naturally there are a lot of different fruits and vegetables, and a lot of different climates. The answer may be different for tomatoes in Alaska vs bananas in Arizona!
However, we can still generalize at least somewhat
Refrigeration will generally slow down any degradation process, and in the case of fruit and vegetables, that can mean slowing down their “ripening” too, as applicable.
However…
Refrigeration will also impede helpful bioactivity too, and that includes quite a list of things.
Here’s a good study that’s quite illustrative; we’d summarize the conclusions but the rather long title already does that nicely:
So, this really is a case of “there are pros and cons, but probably more cons on balance”.
In practical terms, a good take-away from this can be twofold:
- don’t keep fruit and veg in the fridge unless the ambient temperature really requires it
- if the ambient temperature does require it, it’s best to get the produce in fresh each day if that’s feasible, to minimize time spent in the fridge
An extra thing not included there: often when it comes to the spoilage of fruit and veg, the problem is that it respires and oxidizes; reducing the temperature does lower the rate of those, but often a far better way is to remove the oxygen. So for example, if you get carried away and chop too many carrot batons for your hummus night, then putting them in a sealed container can go a long way to keeping them fresh.
See also: How Does the Nutritional Value of Fruits and Vegetables Change Over Time?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Teen Daily Delivery Requested
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I thoroughly enjoy your daily delivery. I’d love to see one for teens too!
That’s great to hear! The average age of our subscribers is generally rather older, but it’s good to know there’s an interest in topics for younger people. We’ll bear that in mind, and see what we can do to cater to that without alienating our older readers!
That said: it’s never too soon to be learning about stuff that affects us when we’re older—there are lifestyle factors at 20 that affect Alzheimer’s risk at 60, for example (e.g. drinking—excessive drinking at 20* is correlated to higher Alzheimer’s risk at 60).
*This one may be less of an issue for our US readers, since the US doesn’t have nearly as much of a culture of drinking under 21 as some places. Compare for example with general European practices of drinking moderately from the mid-teens, or the (happily, diminishing—but historically notable) British practice of drinking heavily from the mid-teens.
Share This Post
-
Caffeine: Cognitive Enhancer Or Brain-Wrecker?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Two Sides Of Caffeine
We asked you for your health-related opinions on caffeine itself, not necessarily the coffee, tea, energy drinks, etc that might contain it.
We have, by the way previously written about the health effects of coffee and tea specifically:
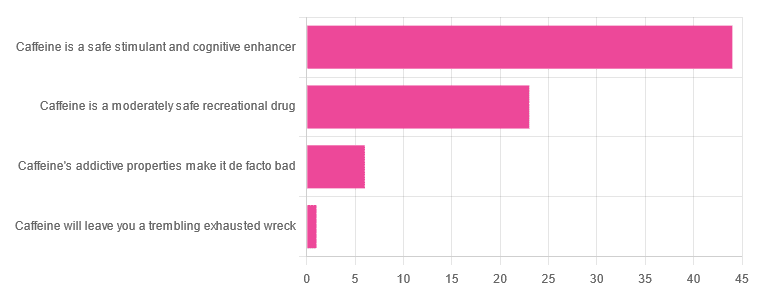
As for our question about caffeine itself, though, we got the above-depicted, below-described, set of results:
- About 59% said “caffeine is a safe stimulant and cognitive enhancer”
- About 31% said “caffeine is a moderately safe recreational drug”
- About 8% said “caffeine’s addictive properties make it de facto bad”
- One (1) person said “caffeine will leave you a trembling exhausted wreck”
But what does the science say?
Caffeine is addictive: True or False?
True, though one will find occasional academics quibbling the definition. Most of the studies into the mechanisms of caffeine addiction have been conducted on rats, but human studies exist too and caffeine is generally considered addictive for humans, for example:
See also:
Notwithstanding its addictive status, caffeine is otherwise safe: True or False?
True-ish, for most people. Some people with heart conditions or a hypersensitivity to caffeine may find it is not safe for them at all, and for the rest of us, the dose makes the poison. For example:
❝Can too much caffeine kill you? Although quite rare, caffeine can be fatal in cases of overdose; such circumstances are generally not applicable to healthy individuals who typically consume caffeine via beverages such as tea or coffee.❞
this paper, by the way, also includes a good example of academics quibbling the definition of addiction!
Caffeine is a cognitive enhancer: True or False?
True, but only in the case of occasional use. If you are using it all the time, your physiology will normalize it and you will require caffeine in order to function at your normal level. To attain higher than that, once addicted to caffeine, would now require something else.
Read more: Caffeine: benefits and drawbacks for technical performance
Caffeine will leave you a trembling exhausted wreck: True or False?
True or False depending on usage:
- The famously moderate 3–5 cups per day will not, for most people, cause any such problems.
- Using/abusing it to make up for lost sleep (or some other source of fatigue, such as physical exhaustion from exertion), however, is much more likely to run into problems.
In the latter case, caffeine really is the “payday loan” of energy! It’ll give you an adrenal boost now (in return, you must suffer the adrenal dumping later, along with lost energy expended in the adrenaline surge), and also, the tiredness that you thought was gone, was just caffeine’s adenosine-blocking activities temporarily preventing you from being able to perceive the tiredness. So you’ll have to pay that back later, with interest, because of the extra time/exertion too.
Want to make caffeine a little more gentle on your system?
Taking l-theanine alongside caffeine can ameliorate some of caffeine’s less wonderful effects—and as a bonus, l-theanine has some nifty benefits of its own, too:
Enjoy!
Share This Post
-
Why do some people’s hair and nails grow quicker than mine?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout recorded history, our hair and nails played an important role in signifying who we are and our social status. You could say, they separate the caveman from businessman.
It was no surprise then that many of us found a new level of appreciation for our hairdressers and nail artists during the COVID lockdowns. Even Taylor Swift reported she cut her own hair during lockdown.
So, what would happen if all this hair and nail grooming got too much for us and we decided to give it all up. Would our hair and nails just keep on growing?
The answer is yes. The hair on our head grows, on average, 1 centimeter per month, while our fingernails grow an average of just over 3 millimetres.
When left unchecked, our hair and nails can grow to impressive lengths. Aliia Nasyrova, known as the Ukrainian Rapunzel, holds the world record for the longest locks on a living woman, which measure an impressive 257.33 cm.
When it comes to record-breaking fingernails, Diana Armstrong from the United States holds that record at 1,306.58 cm.
Most of us, however, get regular haircuts and trim our nails – some with greater frequency than others. So why do some people’s hair and nails grow more quickly?
Jari Lobo/Pexels Remind me, what are they made out of?
Hair and nails are made mostly from keratin. Both grow from matrix cells below the skin and grow through different patterns of cell division.
Nails grow steadily from the matrix cells, which sit under the skin at the base of the nail. These cells divide, pushing the older cells forward. As they grow, the new cells slide along the nail bed – the flat area under the fingernail which looks pink because of its rich blood supply.
Nails, like hair, are made mostly of keratin. Scott Gruber/Unsplash A hair also starts growing from the matrix cells, eventually forming the visible part of the hair – the shaft. The hair shaft grows from a root that sits under the skin and is wrapped in a sac known as the hair follicle.
This sac has a nerve supply (which is why it hurts to pull out a hair), oil-producing glands that lubricate the hair and a tiny muscle that makes your hair stand up when it’s cold.
At the follicle’s base is the hair bulb, which contains the all-important hair papilla that supplies blood to the follicle.
Matrix cells near the papilla divide to produce new hair cells, which then harden and form the hair shaft. As the new hair cells are made, the hair is pushed up above the skin and the hair grows.
But the papilla also plays an integral part in regulating hair growth cycles, as it sends signals to the stem cells to move to the base of the follicle and form a hair matrix. Matrix cells then get signals to divide and start a new growth phase.
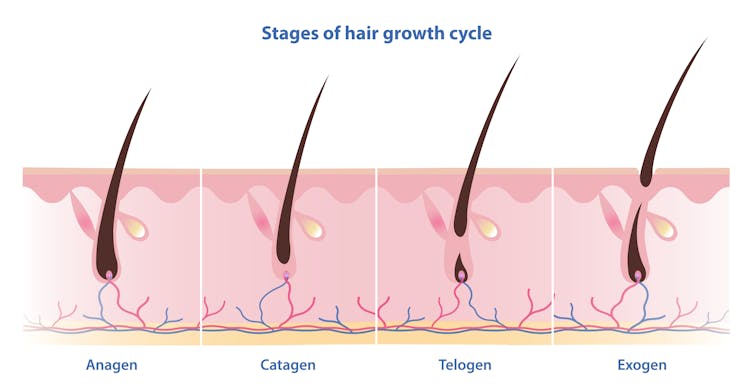
Unlike nails, our hair grows in cycles
Scientists have identified four phases of hair growth, the:
- anagen or growth phase, which lasts between two and eight years
- catagen or transition phase, when growth slows down, lasting around two weeks
- telogen or resting phase, when there is no growth at all. This usually lasts two to three months
- exogen or shedding phase, when the hair falls out and is replaced by the new hair growing from the same follicle. This starts the process all over again.
Hair follicles enter these phases at different times so we’re not left bald. Mosterpiece/Shutterstock Each follicle goes through this cycle 10–30 times in its lifespan.
If all of our hair follicles grew at the same rate and entered the same phases simultaneously, there would be times when we would all be bald. That doesn’t usually happen: at any given time, only one in ten hairs is in the resting phase.
While we lose about 100–150 hairs daily, the average person has 100,000 hairs on their head, so we barely notice this natural shedding.
So what affects the speed of growth?
Genetics is the most significant factor. While hair growth rates vary between individuals, they tend to be consistent among family members.
Nails are also influenced by genetics, as siblings, especially identical twins, tend to have similar nail growth rates.
Genetics have the biggest impact on growth speed. Cottonbro Studio/Pexels But there are also other influences.
Age makes a difference to hair and nail growth, even in healthy people. Younger people generally have faster growth rates because of the slowing metabolism and cell division that comes with ageing.
Hormonal changes can have an impact. Pregnancy often accelerates hair and nail growth rates, while menopause and high levels of the stress hormone cortisol can slow growth rates.
Nutrition also changes hair and nail strength and growth rate. While hair and nails are made mostly of keratin, they also contain water, fats and various minerals. As hair and nails keep growing, these minerals need to be replaced.
That’s why a balanced diet that includes sufficient nutrients to support your hair and nails is essential for maintaining their health.
Nutrition can impact hair and nail growth. Cottonbro Studio/Pexels Nutrient deficiencies may contribute to hair loss and nail breakage by disrupting their growth cycle or weakening their structure. Iron and zinc deficiencies, for example, have both been linked to hair loss and brittle nails.
This may explain why thick hair and strong, well-groomed nails have long been associated with perception of good health and high status.
However, not all perceptions are true.
No, hair and nails don’t grow after death
A persistent myth that may relate to the legends of vampires is that hair and nails continue to grow after we die.
In reality, they only appear to do so. As the body dehydrates after death, the skin shrinks, making hair and nails seem longer.
Morticians are well aware of this phenomenon and some inject tissue filler into the deceased’s fingertips to minimise this effect.
So, it seems that living or dead, there is no escape from the never-ending task of caring for our hair and nails.
Michelle Moscova, Adjunct Associate Professor, Anatomy, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Exercises for Aging-Ankles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can Ankles Deterioration be Stopped?
As we all know (or have experienced!), Ankle mobility deteriorates with age.
We’re here to argue that it’s not all doom and gloom!
(In fact, we’ve written about keeping our feet, and associated body parts, healthy here).
This video by “Livinleggings” (below) provides a great argument that yes, ankle deterioration can be stopped, or even reversed. It’s a must-watch for anyone from yoga enthusiasts to gym warriors who might be unknowingly crippling their ankle-health.
How We Can Prioritise Our Ankles
Poor ankle flexibility isn’t just an inconvenience – it’s a direct route to knee issues, hip hiccups, and back pain. More importantly, ankle strength is a core component of building overall mobility.
With 12 muscles in the ankle, it can be overwhelming to work out which to strengthen – and how. But fear not, we can prioritise three of the twelve: the calf duo (gastrocnemius and soleus) and the shin’s main muscle, the tibialis anterior.
The first step is to test yourself! A simple wall test reveals any hidden truths about your ankle flexibility. Go to the 1:55 point in the video to see how it’s done.
If you can’t do it, you’ve got work to be done.
If you read the book we recommended on great functional exercises for seniors, then you may already be familiar with some super ankle exercises.
Otherwise, these four ankle exercises are a great starting point:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tahini vs Hummus – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tahini to hummus, we picked the tahini.
Why?
Both are great! But tahini is so nutritionally dense, that it makes even the wonder food that is hummus look bad next to it.
In terms of macros, tahini is higher in everything except water. So, higher in protein, carbs, fats, and fiber. In terms of those fats, the fat breakdown is similar for both, being mostly polyunsaturated and monounsaturated, with a small percentage of saturated. Tahini has the lower glycemic index, but both are so low that it makes no practical difference.
In terms of vitamins, tahini has more of vitamins A, B1, B2, B3, B5, B9, E, and choline, while hummus is higher in vitamin B6.
This is a good reason to embellish hummus with some red pepper (vitamin A), a dash of lemon (vitamin C), etc, but we’re judging these foods in their most simple states, for fairness.
When it comes to minerals, tahini has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Meanwhile, hummus is higher in sodium.
Note: hummus is a good source of all those minerals too! Tahini just has more.
In short… Enjoy both, but tahini is the more nutritionally dense by far. On the other hand, if for whatever reason you’re looking for something lower in carbs, fats, and calories, then hummus is where it’s at.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Treat Your Own Back – by Robin McKenzie
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note about the author first: he’s a physiotherapist and not a doctor, but with over 40 years of practice to his name and 33 letters after his name (CNZM OBE FCSP (Hon) FNZSP (Hon) Dip MDT Dip MT), he seems to know his stuff. And certainly, if you visit any physiotherapist, they will probably have some of his books on their own shelves.
This book is intended for the layperson, and as such, explains everything that you need to know, in order to diagnose and treat your back. To this end, he includes assorted tests to perform, a lot of details about various possible back conditions, and then exercises to fix it, i.e. fix whatever you have now learned that the problem is, in your case (if indeed you didn’t know for sure already).
Of course, not everything can be treated by exercises, and he does point to what other things may be necessary in those cases, but for the majority, a significant improvement (if not outright symptom-free status) can be enjoyed by applying the techniques described in this book.
Bottom line: for most people, this book gives you the tools required to do exactly what the title says.
Click here to check out Treat Your Own Back, and treat your own back!
PS: if your issue is not with your back, we recommend you check out his other books in the series (neck, shoulder, hip, knee, ankle) 😎
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: