Can I Eat That? – by Jenefer Roberts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The answer to the question in the title is: you can eat pretty much anything, if you’re prepared for the consequences!
This book looks to give you the information to make your own decisions in that regard. There’s a large section on the science of glucose metabolism in the context of food (other aspects of glucose metabolism aren’t covered), so you will not simply be told “raw carrots are good; mashed potatoes are bad”, you’ll understand many factors that affect it, e.g:
- Macronutrient profiles of food and resultant base glycemic indices
- How the glycemic index changes if you cut something, crush it, mash it, juice it, etc
- How the glycemic index changes if you chill something, heat it, fry it, boil it, etc
- The many “this food works differently in the presence of this other food” factors
- How your relative level of insulin resistance affects things itself
…and much more.
The style is simple and explanatory, without deep science, but with good science and comprehensive advice.
There are also the promised recipes; they’re in an appendix at the back and aren’t the main meat of the book, though.
Bottom line: if you’ve ever found it confusing working out what works how in the mysterious world of diabetes nutrition, this book is a top tier demystifier.
Click here to check out Can I Eat That?, and gain confidence in your food choices!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Boost Your Metabolism When Over 50
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Dawn Andalon, a physiotherapist, explains the role of certain kinds of exercise in metabolism; here’s what to keep in mind:
Work with your body
Many people make the mistake of thinking that it is a somehow a battle of wills, and they must simply will their body to pick up the pace. That’s not how it works though, and while that can occasionally get short-term results, at best it’ll quickly result in exhaustion. So, instead:
- Strength training: engage in weight training 2–3 times per week; build muscle and combat bone loss too. Proper guidance from trainers familiar with older adults is recommended. Pilates (Dr. Andalon is a Pilates instructor) can also complement strength training by enhancing core stability and preventing injuries. The “building muscle” thing is important for metabolism, because muscle increases the body’s metabolic base rate.
- Protein intake: Dr. Andalon advises to consume 25–30 grams of lean protein per meal to support muscle growth and repair (again, important for the same reason as mentioned above re exercise). Dr. Andalon’s recommendation is more protein per meal than is usually advised, as it is generally held that the body cannot use more than about 20g at once.
- Sleep quality: prioritize good quality sleep, by practising good sleep hygiene, and also addressing any potential hormonal imbalances affecting sleep. If you do not get good quality sleep, your metabolism will get sluggish in an effort to encourage you to sleep more.
- Exercise to manage stress: regular walking (such as the popular 10,000 steps daily) helps manage stress and improve metabolism. Zone two cardio (low-intensity movement) also supports joint health, blood flow, and recovery—but the main issue about stress here is that if your body experiences unmanaged stress, it will try to save you from whatever is stressing you by reducing your metabolic base rate so that you can out-survive the bad thing. Which is helpful if the stressful thing is that the fruit trees got stripped by giraffes and hunting did not yield a kill, but not so helpful if the stressful thing is the holiday season.
- Hydration: your body cannot function properly without adequate hydration; water is needed (directly or indirectly) for all bodily processes, and your metabolism will also “dry up” without it.
- Antidiabetic & anti-inflammatory diet: minimize sugar intake and reduce processed foods, especially those with inflammatory refined oils (esp. canola & sunflower) and the like. This has very directly to do with your body’s energy metabolism, and as they say in computing, “garbage in; garbage out”.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Burn! How To Boost Your Metabolism
Take care!
Share This Post
-
How To Gain Weight (Healthily!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Do You Have To Gain?
We have previously promised a three-part series about changing one’s weight:
- Losing weight (specifically, losing fat)
- Gaining weight (specifically, gaining muscle)
- Gaining weight (specifically, gaining fat)
There will be, however, no need for a “losing muscle” article, because (even though sometimes a person might have some reason to want to do this), it’s really just a case of “those things we said for gaining muscle? Don’t do those and the muscle will atrophy naturally”.
Here’s our first article: How To Lose Weight (Healthily!)
While some people will want to lose fat, please do be aware that the association between weight loss and good health is not nearly so strong as the weight loss industry would have you believe:
And, while BMI is not a useful measure of health in general, it’s worth noting that over the age of 65, a BMI of 27 (which is in the high end of “overweight”, without being obese) is associated with the lowest all-cause mortality:
BMI and all-cause mortality in older adults: a meta-analysis
Here was our second article: How To Build Muscle (Healthily!)
And now, it’s time for the last part, which yes, is also something that some people want/need to do (healthily!), and want/need help with that.
How to gain fat, healthily
Fat gets a bad press, but when it comes to health, we would die without it.
Even in the case of having excess fat, the fat itself is not generally the problem, so much as comorbid metabolic issues that are often caused by the same things as the excess fat.
So, how to gain fat healthily?
- Obvious but potentially dangerously misleading answer: “in moderation”
- More useful answer: “carefully”
Because, you can “in moderation” put on less than one pound per week for a few years and be in very bad health by the end of it. So how does this “carefully” work any differently to “in moderation”?
The key is in how we store the fat
Not merely where we store it (though that’ll follow from the “how”), but specifically: how we store it.
- When we consume energy from food in excess of our immediate survival needs, our body stores what it can. This is good!
- When our body is receiving energy from food faster than it can physically process it to store it healthily, it will start shoving it wherever it can instead. This is bad!
This is the physiological equivalent of the difference between tidying a room carefully, and cramming everything into one cupboard in 30 seconds just to get it out of sight.
So, you do need to consume calories yes, but you need to consume them in a way your body can take its time about storing them.
We’ve written before about the science of this, so we’ll share some links, but first, here are the practical tips:
- Do not drink your calories. Drinking calories tends to be the equivalent of injecting sugars directly into your veins, in terms of how quickly it gets received.
- See also: How To Unfatty A Fatty Liver ← this is highly relevant, because the same process that results in unhealthy weight gain, results in liver disease, by the same mechanism (the liver gets overwhelmed).
- Eat your greens. No, they won’t provide many calories, but they are critical to your body not being overwhelmed by the arrival of sugars.
- See also: 10 Ways To Balance Blood Sugars ← the other 9 things are also helpful for not putting on fat unhealthily, so using these alongside a calorie-dense diet can result in healthy fat gain as needed
- Get more of your calories from fats than carbs. Fats will not overwhelm your body’s glycemic response in the same way that carbs will.
- Again this is about getting calories while not getting metabolic disease. See also: How To Prevent And Reverse Type Two Diabetes as the advice is the same for that, for the same reason!
- Consider going low-carb, but even if you choose not to, go for carbs with a low glycemic index instead of a high glycemic index.
- For reference, see: Glycemic Index Chart: Glycemic index and glycemic load ratings for 500+ foods
- Need healthy fats in a snack? Enjoy nuts (unless you have an allergy); they will be your best friend in this regard. As an example, a mere 1oz portion of cashew nuts has 157 calories.
- See also: Why You Should Diversify Your Nuts
- Need healthy fats for cooking? Enjoy olive oil, as it has one of the healthiest lipids profiles available, and is a great way to increase the calorific content of many meals.
Lastly…
Be patient, enjoy your food, and stick as best you can to the above considerations. All strength to you.
Take care!
Share This Post
-
The Knowledge That Harvard Medical School’s Clinical Instructor Dr. Monique Tello Thinks Everyone SHOULD Have About Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anyone (who has not had a double mastectomy, anyway) can get breast cancer.
Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
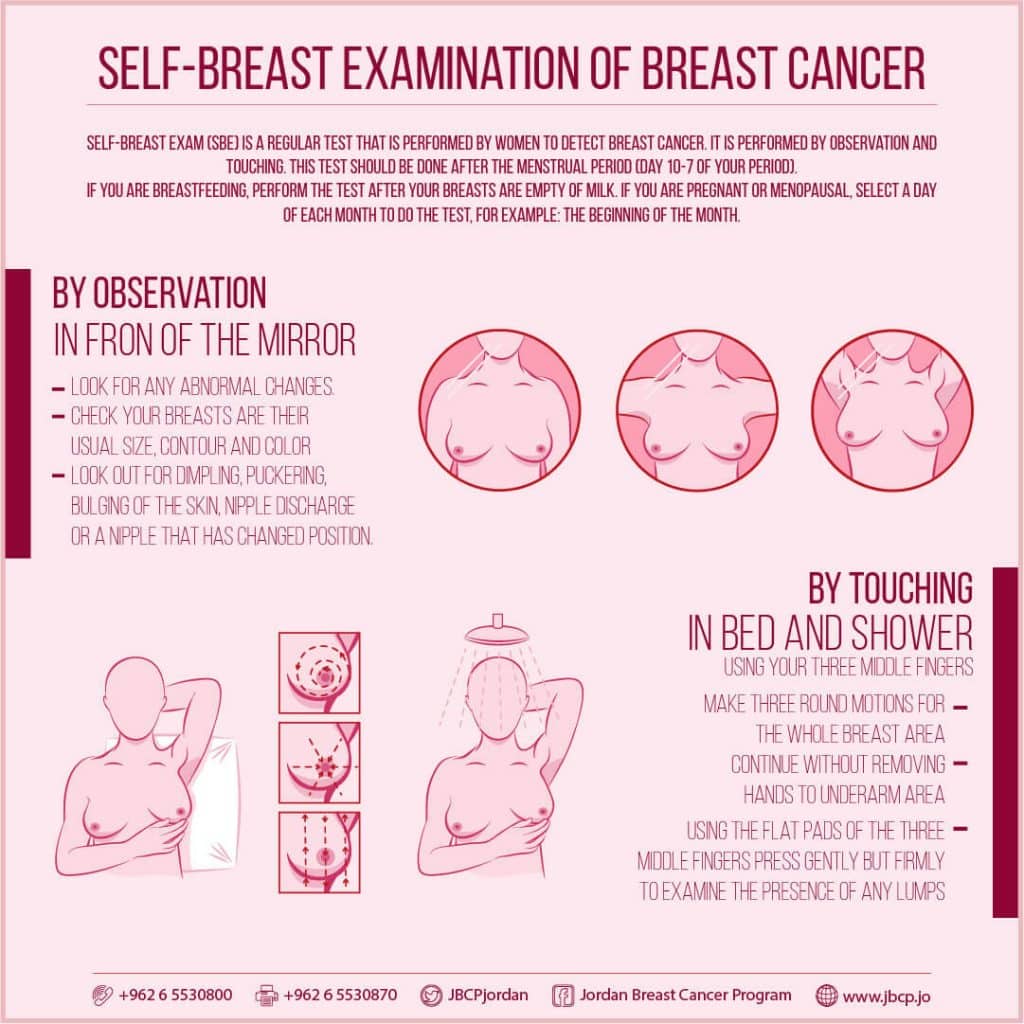
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:
This graphic created by the Jordan Breast Cancer Program (check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it.
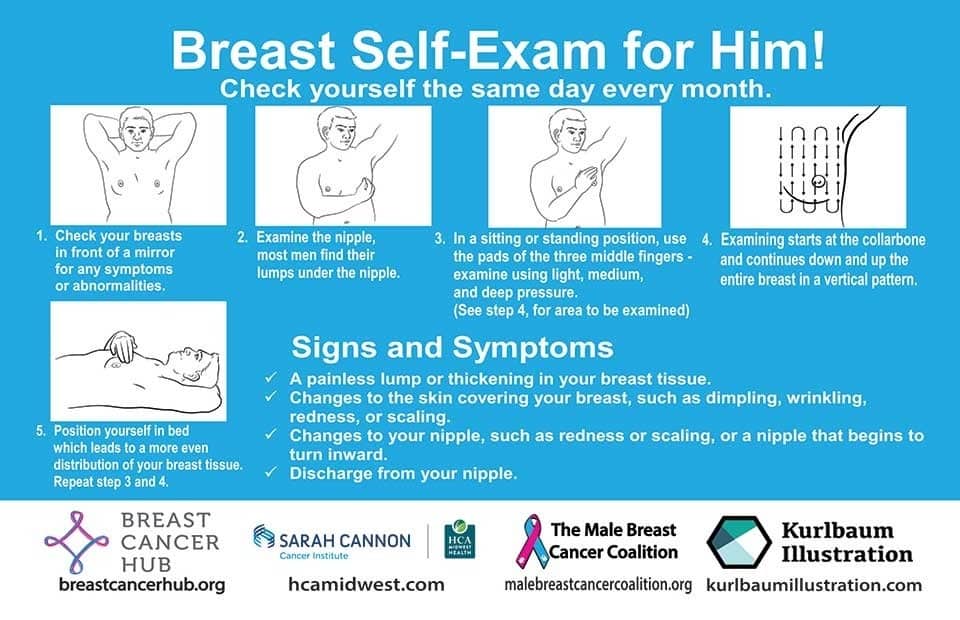
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?
So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to! Take care of yourself; you’re important.
Pssst! Did you scroll past the diagrams, looking for the online 4-minute test promised by the subtitle? If so, scroll back up; the link is in the middle!
Harvard Medical School’s Clinical Instructor’s Five-Point Plan for Heart Health
Dr. Monique Tello, M.D., M.P.H., is a practicing physician at Massachusetts General Hospital, director of research and academic affairs for the MGH DGM Healthy Lifestyle Program, clinical instructor at Harvard Medical School, and author of the evidence-based lifestyle change guide Healthy Habits for Your Heart.
Here are what she says are the five most important factors to help keep your ticker ticking:
5. Have (at most) a moderate alcohol intake! While there are polyphenols such as resveratrol in red wine that could boost heart health, there’s so little per glass that you may need 100–1000 glasses to get the dosage that provides benefits in mouse studies. If you’re not a mouse, it may not be as beneficial, and Dr. Tello recommends drinking no more than one glass per day of any alcohol. What constitutes a glass? It varies from one kind of drink to another, so here’s a handy guide.
4. Don’t smoke. Best of all to never start. But if you did, quit. Simple as that. There is no healthy amount of smoking. While paradoxically, quitting smoking may of course be stressful to you, the long term gains are considered more than worth it. As with all advice, do consult your own physician for guidance, as individual circumstances may vary, and that may change the best approach for you.
3. Maintain a healthy body weight. While BMI (Body Mass Index) is not a perfect system, it’s a system in popular use, and Dr. Tello recommends keeping a BMI between 18.5 and 24.9.
What’s your BMI? It takes into account your height and weight; here’s a Quick BMI Calculator for your convenience.
2. Keep a healthy level of physical activity—which ideally means at least 30 minutes per day vigorous activity, but obviously if you’re not used to this, take it slowly and build up over time. Even just small lifestyle changes (walking where possible, taking the stairs instead of the elevator where possible, etc) can add up to a big difference.
1. Enjoy a healthy diet. This is the single most important thing, and the best modern scientific consensus holds that the best diet contains plenty of vegetables, fruits and nuts, whole grains, and omega-3 fatty acids, while it avoids processed meats, sugar-sweetened beverages, trans fats (what are trans fats?), and too much sodium.
Share This Post
Related Posts
-
3 Appetite Suppressants Better Than Ozempic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Annette Bosworth gives her recommendations, and explains why:
What and how
We’ll get straight to it; the recommendations are:
- Coffee, black, unsweetened: not only suppresses the appetite but also boosts the metabolism, increasing fat burn.
- Salt: especially for when fasting (as under such circumstances we may lose salts without replenishing them), a small taste of this can help satisfy taste buds while replenishing sodium and—depending on the salt—other minerals. For example, if you buy “low-sodium salt” in the supermarket, this is generally sodium chloride cut with potassium chloride and/or occasionally magnesium sulfate.
- Ketones (MCT oil): ketones can suppress hunger, particularly when fasting causes blood sugar levels to drop. Supplementing with MCT oil promotes ketone production in the liver, training the body to produce more ketones naturally, thus curbing appetite.
For more on these including the science of them, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Ozempic vs Five Natural Supplements
- Some Surprising Truths About Hunger And Satiety
- The Fruit That Can Specifically Reduce Belly Fat
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
SuperLife – by Darin Olien
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We mostly know more or less what we’re supposed to be doing, at least to a basic level, when it comes to diet and exercise. So why don’t we do it?
Where Darin Olien excels in this one is making healthy living—mostly the dietary aspects thereof—not just simple, but also easy.
He gives principles we can apply rather than having to memorize lots of information… And his “this will generally be better than that” format also means that the feeling is one of reducing harm, increasing benefits, without needing to get absolutist about anything. And that, too, makes healthy living easier.
The book also covers some areas that a lot of books of this genre don’t—such as blood oxygenation, and maintenance of healthy pH levels—and aspects such as those are elements that help this book to stand out too.
Don’t be put off and think this is a dry science textbook, though—it’s not. In fact, the tone is light and the style is easy-reading throughout.
Bottom line: if you want to take an easy, casual, but scientifically robust approach to tweaking your health for the better, this book will enable you to do that.
Click here to check out SuperLife and start upgrading your health!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An Apple (Cider Vinegar) A Day…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
An Apple (Cider Vinegar) A Day…
You’ve probably heard of people drinking apple cider vinegar for its health benefits. It’s not very intuitive, so today we’re going to see what the science has to say…
Apple cider vinegar for managing blood sugars
Whether diabetic, prediabetic, or not at all, blood sugar spikes aren’t good for us, so anything that evens that out is worth checking out. As for apple cider vinegar…
Diabetes Control: Is Vinegar a Promising Candidate to Help Achieve Targets?
…the answer found by this study was “yes”, but their study was small, and they concluded that more research would be worthwhile. So…
…was also a small study, with the same (positive) results.
But! We then found a much larger systematic review was conducted, examining 744 previously-published papers, adding in another 14 they found via those. After removing 47 duplicates, and removing another 15 for not having a clinical trial or not having an adequate control, they concluded:
❝In this systematic review and meta-analyses, the effect of vinegar consumption on postprandial glucose and insulin responses were evaluated through pooled analysis of glucose and insulin AUC in clinical trials. Vinegar consumption was associated with a statistically significant reduction in postprandial glucose and insulin responses in both healthy participants and participants with glucose disorder.❞
~ Sishehbor, Mansoori, & Shirani
Check it out:
Apple cider vinegar for weight loss?
Yep! It appears to be an appetite suppressant, probably moderating ghrelin and leptin levels.
But…
As a bonus, it also lowers triglycerides and total cholesterol, while raising HDL (good cholesterol), and that’s in addition to doubling the weight loss compared to control:
How much to take?
Most of these studies were done with 1–2 tbsp of apple cider vinegar in a glass of water, at mealtime.
Obviously, if you want to enjoy the appetite-suppressant effects, take it before the meal! If you forget and/or choose to take it after though, it’ll still help keep your blood sugars even and still give you the cholesterol-moderating benefits.
Where to get it?
Your local supermarket will surely have it. Or if you buy it online, you can even get it in capsule form!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: