How worried should I be about cryptosporidiosis? Am I safe at the pool?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You might have heard of something called “cryptosporidiosis” recently, closely followed by warnings to stay away from your local swimming pool if you’ve had diarrhoea.
More than 700 cases of this gastrointestinal disease were reported in Queensland in January, which is 13 times more than in January last year. Just under 500 cases have been recorded in New South Wales this year to-date, while other states have similarly reported an increase in the number of cryptosporidiosis infections in recent months.
Cryptosporidiosis has been listed as a national notifiable disease in Australia since 2001.
But what exactly is it, and should we be worried?
What causes cryptosporidiosis, and who is affected?
Cryptosporidiosis is the disease caused by the parasite Cryptosporidium, of which there are two types that can make us sick. Cryptosporidum hominis only affects humans and is the major cause of recent outbreaks in Australia, while Cryptosporidium parvum can also affect animals.
The infection is spread by spores called oocysts in the stools of humans and animals. When ingested, these oocysts migrate and mature in the small bowel. They damage the small bowel lining and can lead to diarrhoea, nausea, vomiting, fever and abdominal discomfort.
Most people develop symptoms anywhere from one to 12 days after becoming infected. Usually these symptoms resolve within two weeks, but the illness may last longer and can be severe in those with a weakened immune system.
Children and the elderly tend to be the most commonly affected. Cryptosporidiosis is more prevalent in young children, particularly those under five, but the disease can affect people of any age.

LBeddoe/Shutterstock
So how do we catch it?
Most major outbreaks of cryptosporidiosis have been due to people drinking contaminated water. The largest recorded outbreak occurred in Milwaukee in 1993 where 403,000 people were believed to have been infected.
Cryptosporidium oocysts are very small in size and in Milwaukee they passed through the filtration system of one of the water treatment plants undetected, infecting the city’s water supply. As few as ten oocysts can cause infection, making it possible for contaminated drinking water to affect a very large number of people.
Four days after infection a person with cryptosporidiosis can shed up to ten billion oocysts into their stool a day, with the shedding persisting for about two weeks. This is why one infected person in a swimming pool can infect the entire pool in a single visit.
Cryptosporidium oocysts excreted in the faeces of infected humans and animals can also reach natural bodies of water such as beaches, rivers and lakes directly through sewer pipes or indirectly such as in manure transported with surface runoff after heavy rain.
One study which modelled Cryptosporidium concentrations in rivers around the world estimated there are anywhere from 100 to one million oocysts in a litre of river water.
In Australia, cryptosporidiosis outbreaks tend to occur during the late spring and early summer periods when there’s an increase in recreational water activities such as swimming in natural water holes, water catchments and public pools. We don’t know exactly why cases have seen such a surge this summer compared to other years, but we know Cryptosporidium is very infectious.
Oocysts have been found in foods such as fresh vegetables and seafood but these are not common sources of infection in Australia.
What about chlorine?
Contrary to popular belief, chlorine doesn’t kill off all infectious microbes in a swimming pool. Cryptosporidium oocysts are hardy, thick-walled and resistant to chlorine and acid. They are not destroyed by chlorine at the normal concentrations found in swimming pools.
We also know oocysts can be significantly protected from the effects of chlorine in swimming pools by faecal material, so the presence of even small amounts of faecal matter contaminated with Cryptosporidium in a swimming pool would necessitate closure and a thorough decontamination.
Young children and in particular children in nappies are known to increase the potential for disease transmission in recreational water. Proper nappy changing, frequent bathroom breaks and showering before swimming to remove faecal residue are helpful ways to reduce the risk.

Yulia Simonova/Shutterstock
Some sensible precautions
Other measures you can take to reduce yours and others’ risk of cryptosporidiosis include:
- avoid swimming in natural waters such as rivers and creeks during and for at least three days after heavy rain
- avoid swimming in beaches for at least one day after heavy rain
- avoid drinking untreated water such as water from rivers or springs. If you need to drink untreated water, boiling it first will kill the Cryptosporidium
- avoid swallowing water when swimming if you can
- if you’ve had diarrhoea, avoid swimming for at least two weeks after it has resolved
- avoid sharing towels or linen for at least two weeks after diarrhoea has resolved
- avoid sharing, touching or preparing food that other people may eat for at least 48 hours after diarrhoea has resolved
- wash your hands with soap and water after going to the bathroom or before preparing food (Cryptosporidium is not killed by alcohol gels and sanitisers).
Not all cases of diarrhoea are due to cryptosporidiosis. There are many other causes of infectious gastroenteritis and because the vast majority of the time recovery is uneventful you don’t need to see a doctor unless very unwell. If you do suspect you may have cryptosporidiosis you can ask your doctor to refer you for a stool test.
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
True Age – by Dr. Morgan Levine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Yesterday’s book review (Counterclockwise) was about psychological factors affecting physical aging (progression or reversal thereof); today we have a book about the physiological factors affecting physical aging (progression or reversal thereof).
Dr. Levine is first and foremost a gerontological epigeneticist, and a lot of this book touches on her research in that field and that of her colleagues.
She does also discuss direct environmental factors also though, and—as you might well expect—lifestyle factors.
Regular readers of 10almonds are unlikely to gain anything new in the category of lifestyle matters, but a lot of the other material will be enlightening, especially with regard to the things that might at first glance seem set in stone, but we can in fact modify, and thus “choose our own adventure” when it comes to how the rest of our life plays out, healthwise (so: choose wisely!).
The book is mostly an overview on the (at time of writing: 2022) current state of affairs in the world of longevity research, and although it’s not a “how to” manual, there is plenty in the category of practical takeaways to be gleaned too.
The style is is mostly light pop science, but with a lot of hard science woven in—she is a good explainer, and has clearly made a notable effort to explain complex concepts in simple ways, while still delivering the complex concepts too (i.e. not overly “dumbing down”).
Bottom line: if you’d like to know about what can be done to increase your healthspan and general longevity, this book has a lot of answers!
Click here to check out True Age, and shift yours in the direction you prefer!
Share This Post
-
Hitting the beach? Here are some dangers to watch out for – plus 10 essentials for your first aid kit
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Summer is here and for many that means going to the beach. You grab your swimmers, beach towel and sunscreen then maybe check the weather forecast. Did you think to grab a first aid kit?
The vast majority of trips to the beach will be uneventful. However, if trouble strikes, being prepared can make a huge difference to you, a loved one or a stranger.
So, what exactly should you be prepared for?
FTiare/Shutterstock Knowing the dangers
The first step in being prepared for the beach is to learn about where you are going and associated levels of risk.
In Broome, you are more likely to be bitten by a dog at the beach than stung by an Irukandji jellyfish.
In Byron Bay, you are more likely to come across a brown snake than a shark.
In the summer of 2023–24, Surf Life Saving Australia reported more than 14 million Australian adults visited beaches. Surf lifesavers, lifeguards and lifesaving services performed 49,331 first aid treatments across 117 local government areas around Australia. Surveys of beach goers found perceptions of common beach hazards include rips, tropical stingers, sun exposure, crocodiles, sharks, rocky platforms and waves.
Sun and heat exposure are likely the most common beach hazard. The Cancer Council has reported that almost 1.5 million Australians surveyed during summer had experienced sunburn during the previous week. Without adequate fluid intake, heat stroke can also occur.
Lacerations and abrasions are a further common hazard. While surfboards, rocks, shells and litter might seem more dangerous, the humble beach umbrella has been implicated in thousands of injuries.
Sprains and fractures are also associated with beach activities. A 2022 study linked data from hospital, ambulance and Surf Life Saving cases on the Sunshine Coast over six years and found 79 of 574 (13.8%) cervical spine injuries occurred at the beach. Surfing, smaller wave heights and shallow water diving were the main risks.
Rips and rough waves present a higher risk at areas of unpatrolled beach, including away from surf lifesaving flags. Out of 150 coastal drowning deaths around Australia in 2023–24, nearly half were during summer. Of those deaths:
- 56% occurred at the beach
- 31% were rip-related
- 86% were male, and
- 100% occurred away from patrolled areas.
People who had lived in Australia for less than two years were more worried about the dangers, but also more likely to be caught in a rip.
Safety Beach on Victoria’s Mornington Peninsula. Still bring your first aid essentials though. Julia Kuleshova/Shutterstock Knowing your DR ABCs
So, beach accidents can vary by type, severity and impact. How you respond will depend on your level of first aid knowledge, ability and what’s in your first aid kit.
A first aid training company survey of just over 1,000 Australians indicated 80% of people agree cardiopulmonary resuscitation (CPR) is the most important skill to learn, but nearly half reported feeling intimidated by the prospect.
CPR training covers an established checklist for emergency situations. Using the acronym “DR ABC” means checking for:
- Danger
- Response
- Airway
- Breathing
- Circulation
A complete first aid course will provide a range of skills to build confidence and be accredited by the national regulator, the Australian Skills Quality Authority.
What to bring – 10 first aid essentials
Whether you buy a first aid kit or put together you own, it should include ten essential items in a watertight, sealable container:
- Band-Aids for small cuts and abrasions
- sterile gauze pads
- bandages (one small one for children, one medium crepe to hold on a dressing or support strains or sprains, and one large compression bandage for a limb)
- large fabric for sling
- a tourniquet bandage or belt to restrict blood flow
- non-latex disposable gloves
- scissors and tweezers
- medical tape
- thermal or foil blanket
- CPR shield or breathing mask.
Before you leave for the beach, check the expiry dates of any sunscreen, solutions or potions you choose to add.
If you’re further from help
If you are travelling to a remote or unpatrolled beach, your kit should also contain:
- sterile saline solution to flush wounds or rinse eyes
- hydrogel or sunburn gel
- an instant cool pack
- paracetamol and antihistamine medication
- insect repellent.
Make sure you carry any “as-required” medications, such as a Ventolin puffer for asthma or an EpiPen for severe allergy.
Vinegar is no longer recommended for most jellyfish stings, including Blue Bottles. Hot water is advised instead.
In remote areas, also look out for Emergency Response Beacons. Located in high-risk spots, these allow bystanders to instantly activate the surf emergency response system.
If you have your mobile phone or a smart watch with GPS function, make sure it is charged and switched on and that you know how to use it to make emergency calls.
First aid kits suitable for the beach range in price from $35 to over $120. Buy these from certified first aid organisations such as Surf Lifesaving Australia, Australian Red Cross, St John Ambulance or Royal Life Saving. Kits that come with a waterproof sealable bag are recommended.
Be prepared this summer for your trip to the beach and pack your first aid kit. Take care and have fun in the sun.
Andrew Woods, Lecturer, Nursing, Faculty of Health, Southern Cross University and Willa Maguire, Associate Lecturer in Nursing, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
A Cold Shower A Day Keeps The Doctor Away?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Cold Shower A Day Keeps The Doctor Away?
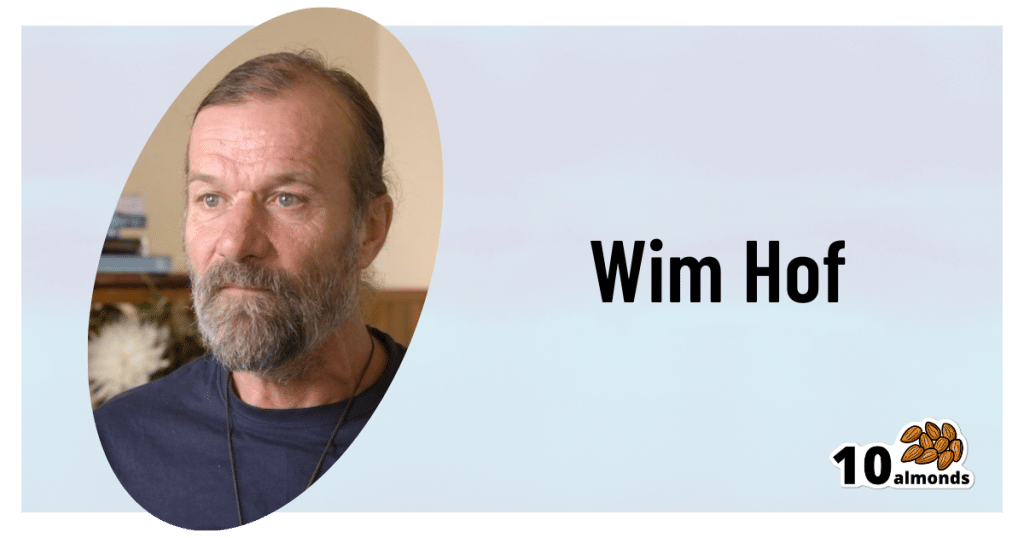
This is Dutch extreme athlete Wim Hof, also known as “The Iceman”! He’s broken many world records mostly relating to the enduring the cold, for example:
- climbing Mount Kilimanjaro in shorts
- running a half-marathon above the Arctic Circle barefoot
- standing in a container completely covered with ice cubes for more than 112 minutes
You might not want to do yoga in your pyjamas on an iceberg, but you might like…
- better circulatory health
- reduced risk of stroke
- a boosted immune system
- healthier skin
- more energy and alertness
…and things like that. Wim Hof’s method is not just about extreme athletic achievements; most of what he does, the stuff that can benefit the rest of us, is much more prosaic.
The Wim Hof Method
For Wim Hof, three things are key:
- Breathing (See: Wim Hof Method Breathing Exercises)
- Commitment (See: How to Increase Willpower)
- Cold therapy (See: Benefits of Cold Therapy)
Today, we’re going to be focusing on the last one there.
What are the benefits of Cold Therapy?
Once upon a time, we didn’t have central heating, electric blankets, thermal underwear, and hot showers. In fact, once upon a time, we didn’t have houses or clothes. We used to be a lot more used to the elements! And while it’s all well and good to enjoy modern comforts, it has left our bodies lacking practice.
Practice at what? Most notably: vasodilation and vasoconstriction, in response to temperature changes. Either:
- vasodilation, because part of our body needs more blood to keep it warm and nourished, or
- vasoconstriction, because part of our body needs less blood running through it to get cooled down.
Switching between the two gives the blood vessels practice at doing it, and improves vascular muscle tone. If your body doesn’t get that practice, your blood vessels will be sluggish at making the change. This can cause circulation problems, which in turn have a big impact in many other areas of health, including:
- cardiovascular disease
- stroke risk
- mood instability
- nerve damage in extremities
On the flipside, if the blood vessels do get regular practice at dilating and constricting, you might enjoy lower risk of those things, and instead:
- improved immune response
- healthier skin
- better quality sleep
- more energy and alertness
- improved sexual performance/responsiveness
So, how to get that, without getting extreme?
As today’s title suggests, “a cold shower a day” is a great practice.
You don’t have to jump straight in, especially if you think your circulation and vascular responses might be a bit sluggish in the first instance. In fact, Wim Hof recommends:
- Week 1: Thirty seconds of cold water at the end of a warm shower each morning
- Week 2: One minute of cold water at the end of a warm shower each morning
- Week 3: A minute and a half of cold water at the end of a warm shower each morning
- Week 4: Two minutes of cold water at the end of a warm shower each morning
How cold is cold?
The benefits of cold exposure begin at around 16ºC / 60ºF, so in most places, water from the cold water mains is sufficiently cold.
As your body becomes more used to making the quick-change on a vascular level, the cold water will seem less shocking to your system. In other words, on day 30 it won’t hit you like it did on day one.
At that point, you can either continue with your two-minutes daily cold shower, and reap the benefits, or if you’re curious to push it further, that’s where ice baths come in!
Can anyone do it, or are any conditions contraindicated?
As ever, we’re a health and productivity newsletter, not doctors, let alone your doctors. Nothing here is medical advice. However, Wim Hof himself says:
❝Listen to your body, and never force the practices. We advise against doing Wim Hof Method if you are dealing with any of the following:
- Epilepsy
- High blood pressure
- Coronary heart disease
- A history of serious healthy issues like heart failure or stroke
- Pregnancy*
- Childhood*❞
*There is simply not enough science regarding the effects of cold exposure on people who are pregnant, or children. Obviously, we don’t expect this to be remedied anytime soon, because the study insitutions’ ethics boards would (rightly!) hold up the study.
As for the other conditions, and just generally if unsure, consult a doctor.
As you can see, this does mean that a limitation of Cold Therapy is that it appears to be far better as a preventative, since it helps guard against the very conditions that could otherwise become contraindications.
We haven’t peppered today’s main feature with study papers, partly because Wim Hof’s own website has kindly collated a collection of them (with links and summaries!) onto one page:
Further reading: The Science Behind The Wim Hof Method
Share This Post
Related Posts
-
Lifestyle vs Multiple Sclerosis & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
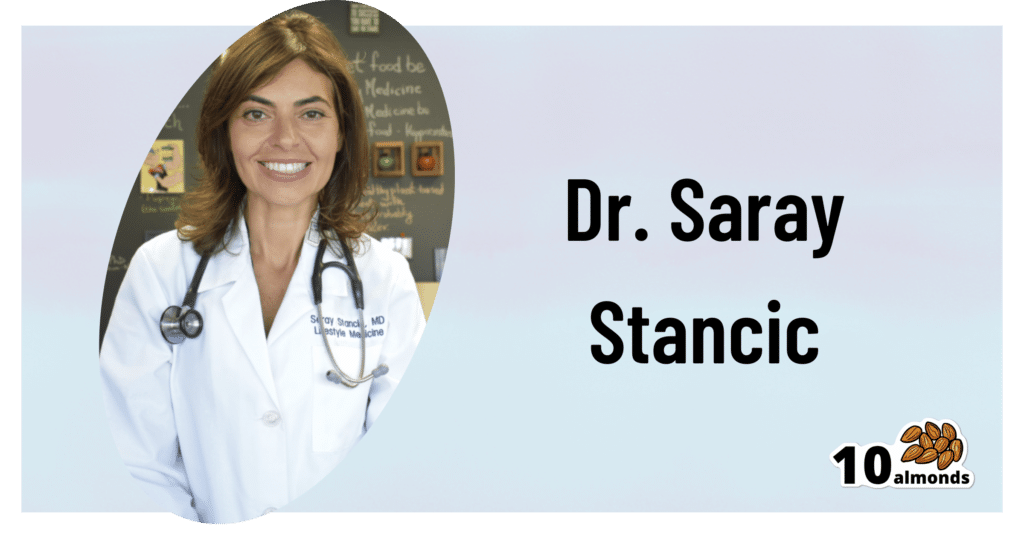
This is Dr. Saray Stancic. She’s another from the ranks of “doctors who got a serious illness and it completely changed how they view the treatment of serious illness”.
In her case, Stancic was diagnosed with multiple sclerosis, and wasn’t impressed with the results from the treatments offered, so (after 8 years of pain, suffering, and many medications, only for her condition to worsen) she set about doing better with an evidence-based lifestyle medicine approach.
After 7 years of her new approach, she would go on to successfully run a marathon and live symptom-free.
All this to say: her approach isn’t a magic quick fix, but it is a serious method for serious results, and after all, while it’d be nice to be magically in perfect health tomorrow, what’s important is being in good health for life, right?
If you’re interested in her impressive story, check out:
Doctor With Multiple Sclerosis On The Collapse Of US Healthcare
If you want to know what she did, then read on…
Six key lifestyle changes
Dr. Stancic credits her recovery to focus on the following evidence-based approaches:
The plant-centered plate
This is critical, and is the one she places most emphasis on. Most chronic diseases are exacerbated, if not outright caused, by chronic inflammation, and one cannot fix that without an anti-inflammatory diet.
An anti-inflammatory diet doesn’t have to be 100% plant-based, but broadly speaking, plants are almost always anti-inflammatory to a greater or lesser degree, while animal products are often pro-inflammatory—especially red meat and unfermented dairy.
For more details, see:
Anti-Inflammatory Diet 101 (What to Eat to Fight Inflammation)
Movement every day
While “exercise is good for you” is in principle not a shocker, remember that her starting point was being in terrible condition with badly flared-up MS.
Important to understand here is that excessive exercise can weaken the immune system and sometimes cause flare-ups of various chronic diseases.
Moving thoroughly and moving often, however, is best. So walking yes, absolutely, but also don’t neglect the rest of your body, do some gentle bodyweight squats (if you can; if you can’t, work up to them), stretch your arms as well as your legs, take all your joints through a full range of motion.
See also:
The Doctor Who Wants Us To Exercise Less, & Move More
Mindful stress management
Stress in life is unavoidable, but how we manage it is up to us. Bad things will continue to happen, great and small, but we can take a deep breath, remember that those things aren’t the boss of us, and deal with it calmly and conscientiously.
Mindfulness-Based Stress Reduction is of course the evidence-based “gold standard” for this, but whatever (not substance-based) method works for you, works for you!
About MBSR:
No-Frills, Evidence-Based Mindfulness
Good sleeping habits
Getting good sleep can be hard for anyone, let alone if you have chronic pain. However, Dr. Stancic advocates for doing whatever we can to get good sleep—which means not just duration (the famous “7–9 hours”), but also quality.
Learn more:
The 6 Dimensions Of Sleep (And Why They Matter)
Substance intake awareness
This one’s not so much of a “don’t do drugs, kids” as the heading makes it look. Dr. Stancic assumes we already know, for example, that smoking is bad for us in a long list of ways, and alcohol isn’t much better.
However, she also advises us that in our eagerness to do that plant-based diet, we would do better to go for whole foods plant-based, rather than the latest processed meat substitutes, for example.
And supplements? She bids us exercise caution, and to make sure to get good quality, as poor quality supplements can be worse than taking nothing (looking at you, cheap turmeric supplements that contain heavy metals).
And of course, that nutrients gained from diet will almost always be better than nutrients gained from supplements, as our body can usually use them better.
And see also, some commonly-made supplements mistakes:
Do You Know Which Supplements You Shouldn’t Take Together? (10 Pairs!)
Human connection
Lastly, we humans are a social species by evolution; as individuals, we may enjoy relatively more or less social contact, but having access to such is important not just for our mental health, but our physical health too—we will tend to deteriorate much more quickly when we have to deal with everything alone, all other things being equal.
It doesn’t mean you need a busy social life if that’s not in your nature, but it does mean it’s incredibly beneficial to have at least a small number of people that you trust and whose company you enjoy, at least relatively accessible to you (i.e., their life need not revolve around you, but they are the kind of people who will generally happily spend time with you and provide support when needed if they can).
As for how:
How To Beat Loneliness & Isolation
Want to know more from Dr. Stancic?
We recently reviewed this very good book of hers, which goes over each of these six things in much more detail than we have room for here:
What’s Missing from Medicine – by Dr. Saray Stancic
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Clean Needles Save Lives. In Some States, They Might Not Be Legal.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Kim Botteicher hardly thinks of herself as a criminal.
On the main floor of a former Catholic church in Bolivar, Pennsylvania, Botteicher runs a flower shop and cafe.
In the former church’s basement, she also operates a nonprofit organization focused on helping people caught up in the drug epidemic get back on their feet.
The nonprofit, FAVOR ~ Western PA, sits in a rural pocket of the Allegheny Mountains east of Pittsburgh. Her organization’s home county of Westmoreland has seen roughly 100 or more drug overdose deaths each year for the past several years, the majority involving fentanyl.
Thousands more residents in the region have been touched by the scourge of addiction, which is where Botteicher comes in.
She helps people find housing, jobs, and health care, and works with families by running support groups and explaining that substance use disorder is a disease, not a moral failing.
But she has also talked publicly about how she has made sterile syringes available to people who use drugs.
“When that person comes in the door,” she said, “if they are covered with abscesses because they have been using needles that are dirty, or they’ve been sharing needles — maybe they’ve got hep C — we see that as, ‘OK, this is our first step.’”
Studies have identified public health benefits associated with syringe exchange services. The Centers for Disease Control and Prevention says these programs reduce HIV and hepatitis C infections, and that new users of the programs are more likely to enter drug treatment and more likely to stop using drugs than nonparticipants.
This harm-reduction strategy is supported by leading health groups, such as the American Medical Association, the World Health Organization, and the International AIDS Society.
But providing clean syringes could put Botteicher in legal danger. Under Pennsylvania law, it’s a misdemeanor to distribute drug paraphernalia. The state’s definition includes hypodermic syringes, needles, and other objects used for injecting banned drugs. Pennsylvania is one of 12 states that do not implicitly or explicitly authorize syringe services programs through statute or regulation, according to a 2023 analysis. A few of those states, but not Pennsylvania, either don’t have a state drug paraphernalia law or don’t include syringes in it.
Those working on the front lines of the opioid epidemic, like Botteicher, say a reexamination of Pennsylvania’s law is long overdue.
There’s an urgency to the issue as well: Billions of dollars have begun flowing into Pennsylvania and other states from legal settlements with companies over their role in the opioid epidemic, and syringe services are among the eligible interventions that could be supported by that money.
The opioid settlements reached between drug companies and distributors and a coalition of state attorneys general included a list of recommendations for spending the money. Expanding syringe services is listed as one of the core strategies.
But in Pennsylvania, where 5,158 people died from a drug overdose in 2022, the state’s drug paraphernalia law stands in the way.
Concerns over Botteicher’s work with syringe services recently led Westmoreland County officials to cancel an allocation of $150,000 in opioid settlement funds they had previously approved for her organization. County Commissioner Douglas Chew defended the decision by saying the county “is very risk averse.”
Botteicher said her organization had planned to use the money to hire additional recovery specialists, not on syringes. Supporters of syringe services point to the cancellation of funding as evidence of the need to change state law, especially given the recommendations of settlement documents.
“It’s just a huge inconsistency,” said Zoe Soslow, who leads overdose prevention work in Pennsylvania for the public health organization Vital Strategies. “It’s causing a lot of confusion.”
Though sterile syringes can be purchased from pharmacies without a prescription, handing out free ones to make drug use safer is generally considered illegal — or at least in a legal gray area — in most of the state. In Pennsylvania’s two largest cities, Philadelphia and Pittsburgh, officials have used local health powers to provide legal protection to people who operate syringe services programs.
Even so, in Philadelphia, Mayor Cherelle Parker, who took office in January, has made it clear she opposes using opioid settlement money, or any city funds, to pay for the distribution of clean needles, The Philadelphia Inquirer has reported. Parker’s position signals a major shift in that city’s approach to the opioid epidemic.
On the other side of the state, opioid settlement funds have had a big effect for Prevention Point Pittsburgh, a harm reduction organization. Allegheny County reported spending or committing $325,000 in settlement money as of the end of last year to support the organization’s work with sterile syringes and other supplies for safer drug use.
“It was absolutely incredible to not have to fundraise every single dollar for the supplies that go out,” said Prevention Point’s executive director, Aaron Arnold. “It takes a lot of energy. It pulls away from actual delivery of services when you’re constantly having to find out, ‘Do we have enough money to even purchase the supplies that we want to distribute?’”
In parts of Pennsylvania that lack these legal protections, people sometimes operate underground syringe programs.
The Pennsylvania law banning drug paraphernalia was never intended to apply to syringe services, according to Scott Burris, director of the Center for Public Health Law Research at Temple University. But there have not been court cases in Pennsylvania to clarify the issue, and the failure of the legislature to act creates a chilling effect, he said.
Carla Sofronski, executive director of the Pennsylvania Harm Reduction Network, said she was not aware of anyone having faced criminal charges for operating syringe services in the state, but she noted the threat hangs over people who do and that they are taking a “great risk.”
In 2016, the CDC flagged three Pennsylvania counties — Cambria, Crawford, and Luzerne — among 220 counties nationwide in an assessment of communities potentially vulnerable to the rapid spread of HIV and to new or continuing high rates of hepatitis C infections among people who inject drugs.
Kate Favata, a resident of Luzerne County, said she started using heroin in her late teens and wouldn’t be alive today if it weren’t for the support and community she found at a syringe services program in Philadelphia.
“It kind of just made me feel like I was in a safe space. And I don’t really know if there was like a come-to-God moment or come-to-Jesus moment,” she said. “I just wanted better.”
Favata is now in long-term recovery and works for a medication-assisted treatment program.
At clinics in Cambria and Somerset Counties, Highlands Health provides free or low-cost medical care. Despite the legal risk, the organization has operated a syringe program for several years, while also testing patients for infectious diseases, distributing overdose reversal medication, and offering recovery options.
Rosalie Danchanko, Highlands Health’s executive director, said she hopes opioid settlement money can eventually support her organization.
“Why shouldn’t that wealth be spread around for all organizations that are working with people affected by the opioid problem?” she asked.
In February, legislation to legalize syringe services in Pennsylvania was approved by a committee and has moved forward. The administration of Gov. Josh Shapiro, a Democrat, supports the legislation. But it faces an uncertain future in the full legislature, in which Democrats have a narrow majority in the House and Republicans control the Senate.
One of the bill’s lead sponsors, state Rep. Jim Struzzi, hasn’t always supported syringe services. But the Republican from western Pennsylvania said that since his brother died from a drug overdose in 2014, he has come to better understand the nature of addiction.
In the committee vote, nearly all of Struzzi’s Republican colleagues opposed the bill. State Rep. Paul Schemel said authorizing the “very instrumentality of abuse” crossed a line for him and “would be enabling an evil.”
After the vote, Struzzi said he wanted to build more bipartisan support. He noted that some of his own skepticism about the programs eased only after he visited Prevention Point Pittsburgh and saw how workers do more than just hand out syringes. These types of programs connect people to resources — overdose reversal medication, wound care, substance use treatment — that can save lives and lead to recovery.
“A lot of these people are … desperate. They’re alone. They’re afraid. And these programs bring them into someone who cares,” Struzzi said. “And that, to me, is a step in the right direction.”
At her nonprofit in western Pennsylvania, Botteicher is hoping lawmakers take action.
“If it’s something that’s going to help someone, then why is it illegal?” she said. “It just doesn’t make any sense to me.”
This story was co-reported by WESA Public Radio and Spotlight PA, an independent, nonpartisan, and nonprofit newsroom producing investigative and public-service journalism that holds power to account and drives positive change in Pennsylvania.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Revive and Maintain Metabolism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝How to jump start a inactive metabolism and keep it going? THANKYOU❞
The good news is, if you’re alive, your metabolism is active (it never stops!). So, it may just need perking up a little.
As for keeping it going, well, that’s what we’re here for! We’re all in favor of healthy longevity.
We’ll do a main feature soon on what we can do to influence our metabolism in either direction, but to give some quick notes here:
- A lot of our metabolism is influenced by genes and is unalterable (without modifying our genes, anyway)
- Metabolism isn’t just one thing—it’s many. And sometimes, parts of our metabolism can be much quicker or slower than others.
- When people talk about wanting a “faster metabolism”, they’re usually referring to fat-burning, and that’s just a small part of the picture, but we understand that it’s a focal point for many.
There really is enough material for a whole main feature on metabolic tweaks, though, so watch this space!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: