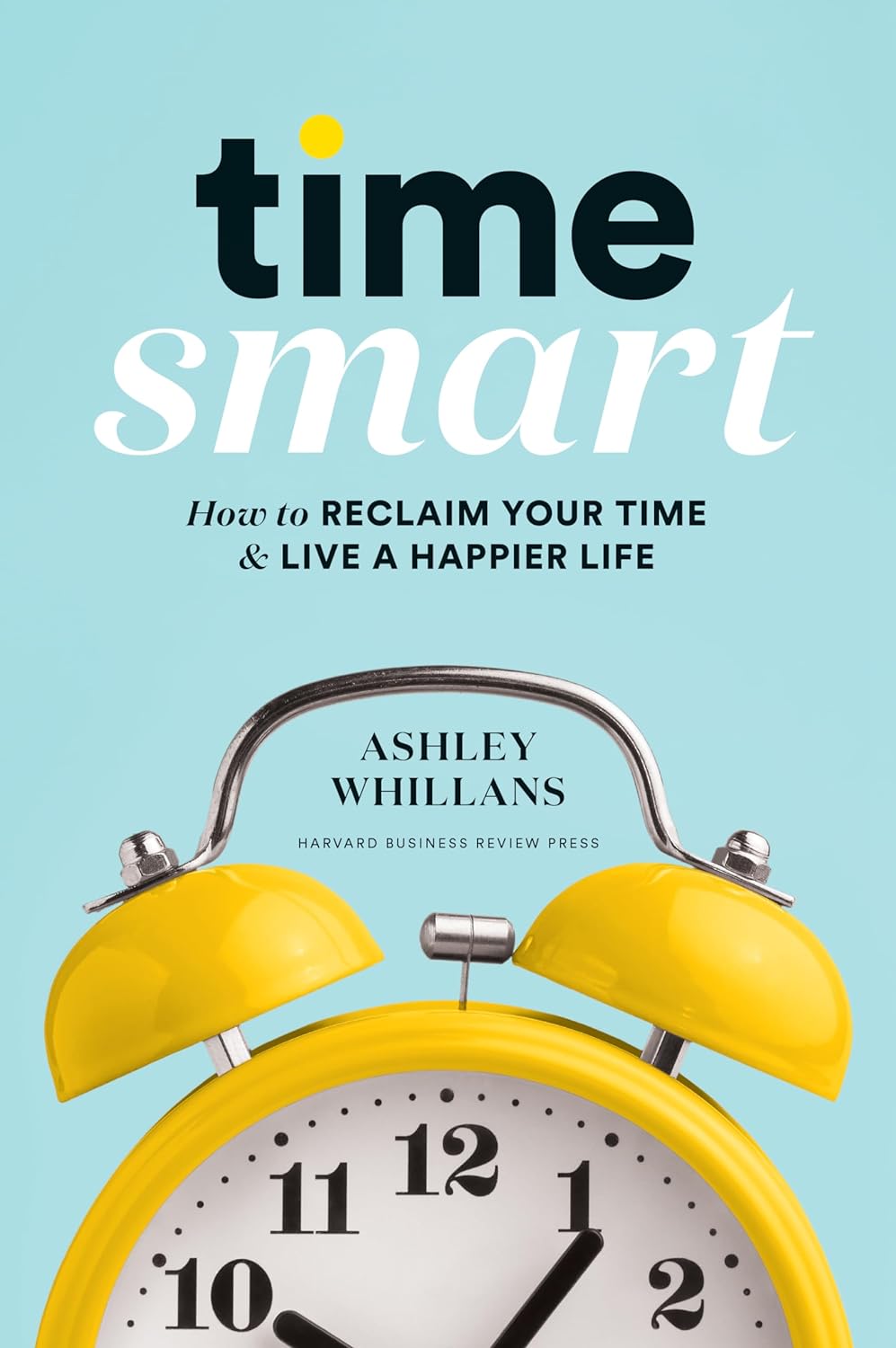
Time Smart – by Dr. Ashley Whillans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: it’s not a productivity book.
What is rather: a book of better wellbeing.
There is a little overlap, insofar as getting “time smart” in the ways that Dr. Whillans recommends will give you more ability to also be more productive—if that’s what you want.
She talks us through time traps and the “time poverty epidemic”, as well as steps to finding time and funding time. Perhaps most critical idea-wise is the chapter on building a “time-affluence habit”, making decisions that prioritize your time-freedom where you can—which in turn will allow you to build yet more. Kind of like compound interest really, but for time.
The writing style is a conversational tone, but peppered with bullet-point lists and charts and the like from time to time, and often with citations to back up claims. It makes for a very readable book, and yet one that’s also inspiring of the confidence that it’s more than just one person’s opinion.
Bottom line: if you sometimes feel like you could do everything you want to if you could just find the time, this book can help you get there.
Click here to check out Time Smart, and live your most satisfying life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
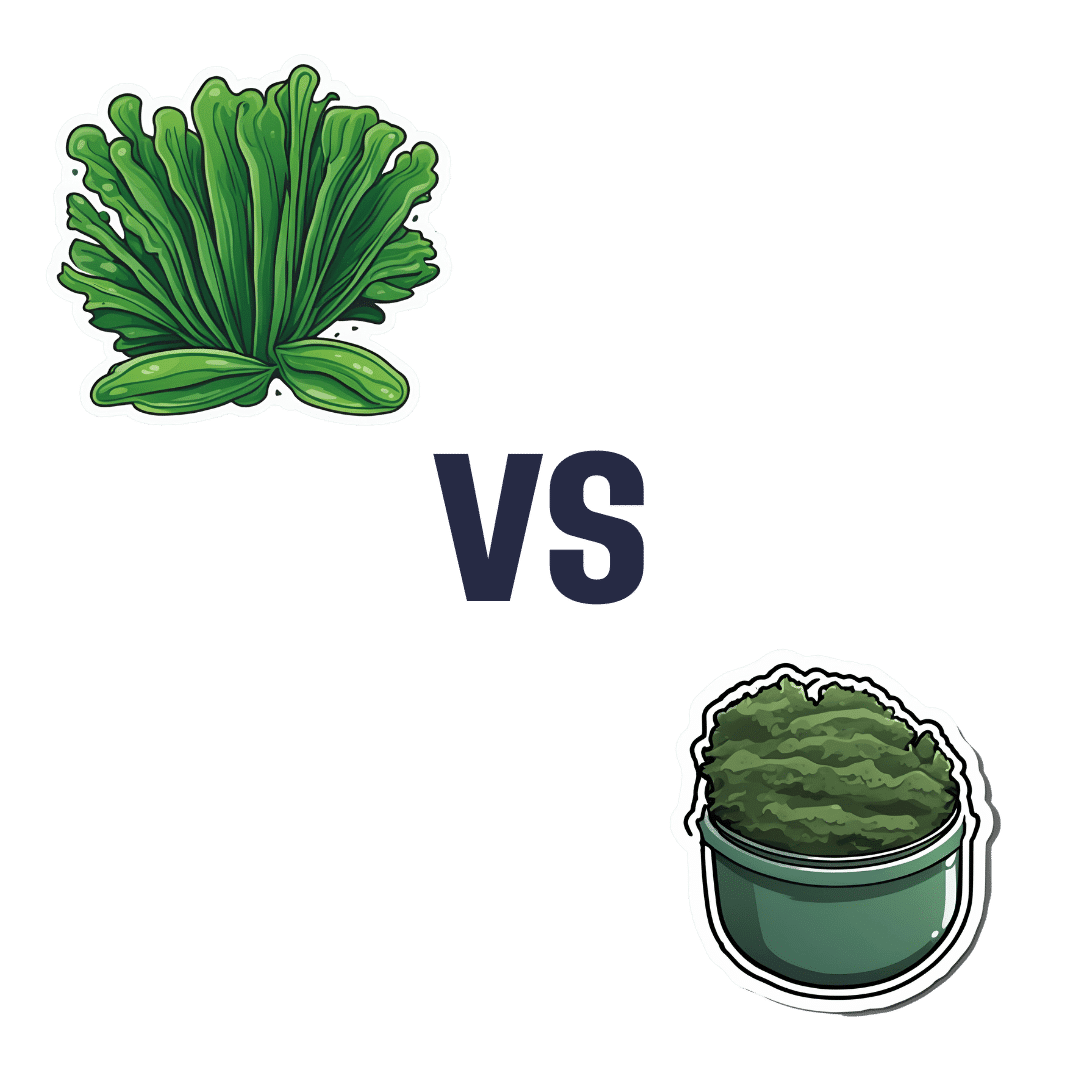
Spirulina vs Nori – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing spirulina to nori, we picked the nori.
Why?
In the battle of the seaweeds, if spirulina is a superfood (and it is), then nori is a super-dooperfood. So today is one of those “a very nutritious food making another very nutritious food look bad by standing next to it” days. With that in mind…
In terms of macros, they’re close to identical. They’re both mostly water with protein, carbs, and fiber. Technically nori is higher in carbs, but we’re talking about 2.5g/100g difference.
In the category of vitamins, spirulina has more vitamin B1, while nori has a lot more of vitamins A, B2, B3, B5, B6, B9, C, E, K, and choline.
When it comes to minerals, it’s a little closer but still a clear win for nori; spirulina has more copper, iron, and magnesium, while nori has more calcium, manganese, phosphorus, potassium, and zinc.
Want to try some nori? Here’s an example product on Amazon 😎
Want to learn more?
You might like to read:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nori was an important part of the diet enjoyed here
Take care!
Share This Post
-
3 Things Everyone Over 50 Must Do Daily for Healthy Feet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Will Harlow, the over-50s specialist physio, wants you to be on a good footing:
Daily steps in the right direction
The three daily exercises recommended in the video are:
Exercise 1: Towel Scrunch
The towel scrunch exercise strengthens the flexor muscles in the feet, improving balance and improving contact with the ground. To do this exercise, sit on a chair with a towel placed on the floor beneath your toes while keeping your heels on the ground. Use only your toes to pull the towel toward your heel, scrunching it up as much as possible. This movement strengthens the arch of the foot and can help alleviate symptoms of flat feet. For best results, practice this exercise for 2–3 minutes once or twice daily. Once you’ve got the hand of doing it sitting, do it while standing.
Exercise 2: Big Toe Extension
Big toe extension is an essential exercise for maintaining foot mobility and improving walking kinesthetics by preventing stiffness in the big toe. To do this exercise, keep your foot flat on the floor and try to lift only your big toe while keeping the four other toes firmly pressed down. To be clear, we mean under its own power; not using your hands to help. Many people find this difficult initially, but it’s due to a loss of neural connection rather than muscle strength, so with practice, the ability to isolate the movement improves quite quickly. Perform 10 repetitions in a row, three times per day, for optimal benefits. Once you’ve got the hand of doing it sitting, do it while standing.
Exercise 3: Calf Stretch
The calf stretch is an important exercise for maintaining foot health by preventing tight calves, which can contribute to issues like plantar fasciitis and Morton’s neuroma. To do this stretch, place your hands against a wall for support and extend one leg straight behind you while keeping your other heel firmly on the floor. The front knee should be bent while the back leg remains straight, creating a stretch in the calf. Hold this position for 30 seconds (building up to that, if necessary). Since the effectiveness of stretching comes from frequency rather than duration, this stretch should be performed three to four times per day for the best results.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation ← this one’s about general habits, not exercises
Take care!
Share This Post
-
The Mediterranean Diet Cookbook for Beginners – by Jessica Aledo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of Mediterranean Diet books on the market, and not all of them actually stick to the Mediterranean Diet. There’s a common mistake of thinking “Well, this dish is from the Mediterranean region, so…”, but that doesn’t make, for example, bacon-laden carbonara part of the Mediterranean Diet!
Jessica Aledo does better, and sticks unwaveringly to the Mediterranean Diet principles.
First, she gives a broad introduction, covering:
- The Mediterranean Diet pyramid
- Foods to eat on the Mediterranean Diet
- Foods to avoid on the Mediterranean Diet
- Benefits of the Mediterranean Diet
Then, it’s straight into the recipes, of which there are 201 (as with many recipe books, the title is a little misleading about this).
They’re divided into sections, thus:
- Breakfasts
- Lunches
- Snacks
- Dinners
- Desserts
The recipes are clear and simple, one per double-page, with high quality color illustrations. They give ingredients/directions/nutrients. There’s no padding!
Helpfully, she does include a shopping list as an appendix, which is really useful!
Bottom line: if you’re looking to build your Mediterranean Diet repertoire, this book is an excellent choice.
Get your copy of The Mediterranean Diet Cookbook for Beginners from Amazon today!
Share This Post
Related Posts
-
Lobster vs Crab – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing lobster to crab, we picked the crab.
Why?
Generally speaking, most seafood is healthy in moderation (assuming it’s well-prepared, not poisonous, and you don’t have an allergy), and for most people, these two sea creatures are indeed considered a reasonable part of a healthy balanced diet.
In terms of macros, they’re comparable in protein, and technically crab has about 2x the fat, but in both cases it’s next to nothing, so 2x almost nothing is still almost nothing. And, if we break down the lipids profiles, crab has a sufficiently smaller percentage of saturated fat (compared to monounsaturated and polyunsaturated), that crab actually has less saturated fat than lobster. In balance, the category of macros is either a tie or a slight win for crab, depending on your personal priorities.
When it comes to vitamins, crab wins easily with more of vitamins A, B1, B2, B6, B9, B12, and C, in most cases by considerable margins (we’re talking multiples of what lobster has). Lobster, meanwhile, has more of vitamin B3 (tiny margin) and vitamin B5 (pantothenic acid, as in, the vitamin that’s in basically everything edible, and thus almost impossible to be deficient in unless literally starving).
The minerals scene is more balanced; lobster has more calcium, copper, manganese, and selenium, while crab has more iron, magnesium, phosphorus, potassium, and zinc. The margins are comparable from one creature to another, so all in all the 4:5 score means a modest win for crab.
Both of these creatures are good sources of omega-3 fatty acids, but crab is better.
Lobster and crab are both somewhat high in cholesterol, but crab is the relatively lower of the two.
In short: for most people most of the time, both are fine to enjoy in moderation, but if picking one, crab is the healthier by most metrics.
Want to learn more?
You might like to read:
Shrimp vs Caviar – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why a common asthma drug will now carry extra safety warnings about depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australia’s Therapeutic Goods Administration (TGA) recently issued a safety alert requiring extra warnings to be included with the asthma and hay fever drug montelukast.
The warnings are for users and their families to look for signs of serious behaviour and mood-related changes, such as suicidal thoughts and depression. The new warnings need to be printed at the start of information leaflets given to both patients and health-care providers (sometimes called a “boxed” warning).
So why did the TGA issue this warning? And is there cause for concern if you or a family member uses montelukast? Here’s what you need to know.
First, what is montelukast?
Montelukast is a prescription drug also known by its brand names which include Asthakast, Lukafast, Montelair and Singulair. It’s used to manage the symptoms of mild-to-moderate asthma and seasonal hay fever in children and adults.
Asthma occurs when the airways tighten and produce extra mucus, which makes it difficult to get air into the lungs. Likewise, the runny nose characteristic of hay fever occurs due to the overproduction of mucus.
Leukotrienes are an important family of chemicals found throughout the airways and involved in both mucus production and airway constriction. Montelukast is a cysteinyl leukotriene receptor antagonist, meaning it blocks the site in the airways where the leukotrienes work.
Montelukast can’t be used to treat acute asthma (an asthma attack), as it takes time for the tablet to be broken down in the stomach and for it to be absorbed into the body. Rather, it’s taken daily to help prevent asthma symptoms or seasonal hay fever.
It can be used alongside asthma puffers that contain corticosteriods and drugs like salbutamol (Ventolin) in the event of acute attacks.
What is the link to depression and suicide?
The possibility that this drug may cause behavioural changes is not new information. Manufacturers knew this as early as 2007 and issued warnings for possible side-effects including depression, suicidality and anxiousness.
The United Kingdom’s Medicines and Healthcare products Regulatory Agency has required a warning since 2008 but mandated a more detailed warning in 2019. The United States’ Food and Drug Administration has required boxed warnings for the drug since 2020.
Montelukast can help children and adults with asthma. adriaticfoto/Shutterstock Montelukast is known to potentially induce a number of behaviour and mood changes, including agitation, anxiety, depression, irritability, obsessive-compulsive symptoms, and suicidal thoughts and actions.
Initially a 2009 study that analysed data from 157 clinical trials involving more than 20,000 patients concluded there were no completed suicides due to taking the drug, and only a rare risk of suicide thoughts or attempts.
The most recent study, published in November 2024, examined data from more than 100,000 children aged 3–17 with asthma or hay fever who either took montelukast or used only inhaled corticosteroids.
It found montelukast use was associated with a 32% higher incidence of behavioural changes. The behaviour change with the strongest association was sleep disturbance, but montelukast use was also linked to increases in anxiety and mood disorders.
In the past ten years, around 200 incidences of behavioural side-effects have been reported to the TGA in connection with montelukast. This includes 57 cases of depression, 60 cases of suicidal thoughts and 17 suicide attempts or incidents of intentional self-injury. There were seven cases where patients taking the drug did complete a suicide.
This is of course tragic. But these numbers need to be seen in the context of the number of people taking the drug. Over the same time period, more than 200,000 scripts for montelukast have been filled under the Pharmaceutical Benefits Scheme.
Overall, we don’t know conclusively that montelukast causes depression and suicide, just that it seems to increase the risk for some people.
We’re still not sure how the drug can act on the brain to lead to behaviour changes. Elif Bayraktar/Shutterstock And if it does change behaviour, we don’t fully understand how this happens. One hypothesis is that the drug and its breakdown products (or metabolites) affect brain chemistry.
Specifically, it might interfere with how the brain detoxifies the antioxidant glutathione or alter the regulation of other brain chemicals, such as neurotransmitters.
Why is the TGA making this change now?
The new risk warning requirement comes from a meeting of the Australian Advisory Committee on Medicines where they were asked to provide advice on ways to minimise the risk for the drug given current international recommendations.
Even though the 2024 review didn’t highlight any new risks, to align with international recommendations, and help address consumer concerns, the advisory committee recommended a boxed warning be added to drug information sheets.
If you have asthma and take montelukast (or your child does), you should not just stop taking the drug, because this could put you at risk of an attack that could be life threatening. If you’re concerned, speak to your doctor who can discuss the risks and benefits of the medication for you, and, if appropriate, prescribe a different medication.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Nial Wheate, Professor of Pharmaceutical Chemistry, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Overdosing on Chemo: A Common Gene Test Could Save Hundreds of Lives Each Year
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One January morning in 2021, Carol Rosen took a standard treatment for metastatic breast cancer. Three gruesome weeks later, she died in excruciating pain from the very drug meant to prolong her life.
Rosen, a 70-year-old retired schoolteacher, passed her final days in anguish, enduring severe diarrhea and nausea and terrible sores in her mouth that kept her from eating, drinking, and, eventually, speaking. Skin peeled off her body. Her kidneys and liver failed. “Your body burns from the inside out,” said Rosen’s daughter, Lindsay Murray, of Andover, Massachusetts.
Rosen was one of more than 275,000 cancer patients in the United States who are infused each year with fluorouracil, known as 5-FU, or, as in Rosen’s case, take a nearly identical drug in pill form called capecitabine. These common types of chemotherapy are no picnic for anyone, but for patients who are deficient in an enzyme that metabolizes the drugs, they can be torturous or deadly.
Those patients essentially overdose because the drugs stay in the body for hours rather than being quickly metabolized and excreted. The drugs kill an estimated 1 in 1,000 patients who take them — hundreds each year — and severely sicken or hospitalize 1 in 50. Doctors can test for the deficiency and get results within a week — and then either switch drugs or lower the dosage if patients have a genetic variant that carries risk.
Yet a recent survey found that only 3% of U.S. oncologists routinely order the tests before dosing patients with 5-FU or capecitabine. That’s because the most widely followed U.S. cancer treatment guidelines — issued by the National Comprehensive Cancer Network — don’t recommend preemptive testing.
The FDA added new warnings about the lethal risks of 5-FU to the drug’s label on March 21 following queries from KFF Health News about its policy. However, it did not require doctors to administer the test before prescribing the chemotherapy.
The agency, whose plan to expand its oversight of laboratory testing was the subject of a House hearing, also March 21, has said it could not endorse the 5-FU toxicity tests because it’s never reviewed them.
But the FDA at present does not review most diagnostic tests, said Daniel Hertz, an associate professor at the University of Michigan College of Pharmacy. For years, with other doctors and pharmacists, he has petitioned the FDA to put a black box warning on the drug’s label urging prescribers to test for the deficiency.
“FDA has responsibility to assure that drugs are used safely and effectively,” he said. The failure to warn, he said, “is an abdication of their responsibility.”
The update is “a small step in the right direction, but not the sea change we need,” he said.
Europe Ahead on Safety
British and European Union drug authorities have recommended the testing since 2020. A small but growing number of U.S. hospital systems, professional groups, and health advocates, including the American Cancer Society, also endorse routine testing. Most U.S. insurers, private and public, will cover the tests, which Medicare reimburses for $175, although tests may cost more depending on how many variants they screen for.
In its latest guidelines on colon cancer, the Cancer Network panel noted that not everyone with a risky gene variant gets sick from the drug, and that lower dosing for patients carrying such a variant could rob them of a cure or remission. Many doctors on the panel, including the University of Colorado oncologist Wells Messersmith, have said they have never witnessed a 5-FU death.
In European hospitals, the practice is to start patients with a half- or quarter-dose of 5-FU if tests show a patient is a poor metabolizer, then raise the dose if the patient responds well to the drug. Advocates for the approach say American oncology leaders are dragging their feet unnecessarily, and harming people in the process.
“I think it’s the intransigence of people sitting on these panels, the mindset of ‘We are oncologists, drugs are our tools, we don’t want to go looking for reasons not to use our tools,’” said Gabriel Brooks, an oncologist and researcher at the Dartmouth Cancer Center.
Oncologists are accustomed to chemotherapy’s toxicity and tend to have a “no pain, no gain” attitude, he said. 5-FU has been in use since the 1950s.
Yet “anybody who’s had a patient die like this will want to test everyone,” said Robert Diasio of the Mayo Clinic, who helped carry out major studies of the genetic deficiency in 1988.
Oncologists often deploy genetic tests to match tumors in cancer patients with the expensive drugs used to shrink them. But the same can’t always be said for gene tests aimed at improving safety, said Mark Fleury, policy director at the American Cancer Society’s Cancer Action Network.
When a test can show whether a new drug is appropriate, “there are a lot more forces aligned to ensure that testing is done,” he said. “The same stakeholders and forces are not involved” with a generic like 5-FU, first approved in 1962, and costing roughly $17 for a month’s treatment.
Oncology is not the only area in medicine in which scientific advances, many of them taxpayer-funded, lag in implementation. For instance, few cardiologists test patients before they go on Plavix, a brand name for the anti-blood-clotting agent clopidogrel, although it doesn’t prevent blood clots as it’s supposed to in a quarter of the 4 million Americans prescribed it each year. In 2021, the state of Hawaii won an $834 million judgment from drugmakers it accused of falsely advertising the drug as safe and effective for Native Hawaiians, more than half of whom lack the main enzyme to process clopidogrel.
The fluoropyrimidine enzyme deficiency numbers are smaller — and people with the deficiency aren’t at severe risk if they use topical cream forms of the drug for skin cancers. Yet even a single miserable, medically caused death was meaningful to the Dana-Farber Cancer Institute, where Carol Rosen was among more than 1,000 patients treated with fluoropyrimidine in 2021.
Her daughter was grief-stricken and furious after Rosen’s death. “I wanted to sue the hospital. I wanted to sue the oncologist,” Murray said. “But I realized that wasn’t what my mom would want.”
Instead, she wrote Dana-Farber’s chief quality officer, Joe Jacobson, urging routine testing. He responded the same day, and the hospital quickly adopted a testing system that now covers more than 90% of prospective fluoropyrimidine patients. About 50 patients with risky variants were detected in the first 10 months, Jacobson said.
Dana-Farber uses a Mayo Clinic test that searches for eight potentially dangerous variants of the relevant gene. Veterans Affairs hospitals use a 11-variant test, while most others check for only four variants.
Different Tests May Be Needed for Different Ancestries
The more variants a test screens for, the better the chance of finding rarer gene forms in ethnically diverse populations. For example, different variants are responsible for the worst deficiencies in people of African and European ancestry, respectively. There are tests that scan for hundreds of variants that might slow metabolism of the drug, but they take longer and cost more.
These are bitter facts for Scott Kapoor, a Toronto-area emergency room physician whose brother, Anil Kapoor, died in February 2023 of 5-FU poisoning.
Anil Kapoor was a well-known urologist and surgeon, an outgoing speaker, researcher, clinician, and irreverent friend whose funeral drew hundreds. His death at age 58, only weeks after he was diagnosed with stage 4 colon cancer, stunned and infuriated his family.
In Ontario, where Kapoor was treated, the health system had just begun testing for four gene variants discovered in studies of mostly European populations. Anil Kapoor and his siblings, the Canadian-born children of Indian immigrants, carry a gene form that’s apparently associated with South Asian ancestry.
Scott Kapoor supports broader testing for the defect — only about half of Toronto’s inhabitants are of European descent — and argues that an antidote to fluoropyrimidine poisoning, approved by the FDA in 2015, should be on hand. However, it works only for a few days after ingestion of the drug and definitive symptoms often take longer to emerge.
Most importantly, he said, patients must be aware of the risk. “You tell them, ‘I am going to give you a drug with a 1 in 1,000 chance of killing you. You can take this test. Most patients would be, ‘I want to get that test and I’ll pay for it,’ or they’d just say, ‘Cut the dose in half.’”
Alan Venook, the University of California-San Francisco oncologist who co-chairs the panel that sets guidelines for colorectal cancers at the National Comprehensive Cancer Network, has led resistance to mandatory testing because the answers provided by the test, in his view, are often murky and could lead to undertreatment.
“If one patient is not cured, then you giveth and you taketh away,” he said. “Maybe you took it away by not giving adequate treatment.”
Instead of testing and potentially cutting a first dose of curative therapy, “I err on the latter, acknowledging they will get sick,” he said. About 25 years ago, one of his patients died of 5-FU toxicity and “I regret that dearly,” he said. “But unhelpful information may lead us in the wrong direction.”
In September, seven months after his brother’s death, Kapoor was boarding a cruise ship on the Tyrrhenian Sea near Rome when he happened to meet a woman whose husband, Atlanta municipal judge Gary Markwell, had died the year before after taking a single 5-FU dose at age 77.
“I was like … that’s exactly what happened to my brother.”
Murray senses momentum toward mandatory testing. In 2022, the Oregon Health & Science University paid $1 million to settle a suit after an overdose death.
“What’s going to break that barrier is the lawsuits, and the big institutions like Dana-Farber who are implementing programs and seeing them succeed,” she said. “I think providers are going to feel kind of bullied into a corner. They’re going to continue to hear from families and they are going to have to do something about it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: