Bold Beans – by Amelia Christie-Miller
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know beans are one of the most healthful foods around, but how to include more of them, without getting boring?
This book has the answer, giving 80 exciting recipes, divided into the following sections:
- Speedy beans
- Bean snacks & sharing plates
- Brothy beans
- Bean bowls
- Hearty salads
- Bean feasts
The recipes are obviously all bean-centric, though if you have a particular dietary restriction, watch out for the warning labels on some (e.g. meat, fish, dairy, gluten, etc), and make a substitution if appropriate.
The recipes themselves have a happily short introductory paragraph, followed by all you’d expect from a recipe book (ingredients, measurements, method, picture)
There’s also a reference section, to learn about different kinds of beans and bean-related culinary methods that can be applied per your preferences.
Bottom line: if you’d like to include more beans in your daily diet but are stuck for making them varied and interesting, this is the book for you!
Click here to check out Bold Beans, and get your pulse racing (in a good way!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gentle Nutrition – by Rachel Hartley, RD, LD
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle here claims “a non-diet approach”, but doesn’t everything, nowadays? Even books titled “The such-and-such Diet” tend to also assure us “it’s not actually a diet; it’s just a way of eating”, as if a diet is not—by definition—a way of eating. Usually what they want to communicate is that it’s not a restrictive diet, usually meaning not restrictive in quantity, or not restrictive in food type (rarely both).
This book is about intuitive eating, which is about as non-restrictive as any dietary approach can be, since it doesn’t restrict food type at at all, and it doesn’t restrict quantity in advance—rather, we learn to pay closer attention to our full signals.
No wait, we don’t. This time, it’s not about “full”, it’s about “satisfied”. This comes in two forms:
- A principle somewhat akin to the “eat until 80% full” idea
- A principle of ensuring the good is culinarily satisfying
This latter is important, if we want to have a good relationship with eating, and it also helps reduce portion sizes, when we truly take the time to mindfully savor a tasty morsel, rather than wolf down a plate of mediocre food.
The style is one that balance being encouraging with delivering science to back up that encouragement. This not only means encouragement to take up this dietary approach, but also, encouragement to let go of things like calorie-counting and BMI.
The recipes arranged per meal type, and indeed include things not found in many healthy eating books, such as gyoza dumplings, gnocchi, wontons, and shortbread. The recipes are mostly not, by default, vegan, vegetarian, gluten-free, dairy-free, or such. So if you have your own food restriction(s), the number of usable recipes will be diminished, barring any substitutions you can make yourself.
Bottom line: this is more about about how to go about intuitive eating, than it is a book with a lot of nutritional information (though there is some of that too). If you’d like to get going with intuitive eating, then this book can help.
Click here to check out Gentle Nutrition, and nourish gently!
Share This Post
-
Top 10 Unhealthy Foods: How Many Do You Eat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The items on this list won’t come as a shocking surprise to you, but it can be a good opportunity to do a quick tally and see how many of these have snuck into your diet:
The things that take away health instead of adding it
Without further ado, they are…
- Alcohol: not only is it high in empty calories, but also it’s bad for pretty much everything, especially increasing the risks of liver disease, high blood pressure, and stroke.
- Processed snacks: low in nutrition; contain unhealthy fats, refined sugars, and artificial additives that often aren’t great.
- Potato chips: get their own category for being especially high in fat, sodium, and empty calories; contribute to heart disease and weight gain.
- Processed cheese: some kinds of cheese are gut-healthy in moderation, but this isn’t. Instead, it’s just loaded with saturated fats, sodium, and sugars, and is pretty much heart disease in a slice.
- Donuts: deep-fried, sugary, and made with refined flour; cause blood sugar spikes and crashes, and what’s bad for your blood sugars is bad for almost everything else.
- French fries & similar deep-fried foods: high in saturated fats and sodium; contribute to obesity and heart issues, are not great for blood sugars either.
- White bread: made with refined flour; cause blood sugar spikes and metabolic woes.
- Sodas: high in sugar or artificial sweeteners; can easily lead to weight gain, diabetes, and tooth decay.
- Processed meats: high in calories and salt; strongly associated with heart disease and cancer.
- Hot dogs & fast food burgers: get their own category for being the absolute worst of the above-mentioned processed meats.
This writer scored: no / rarely / no / no / no / rarely / rarely / rarely / no / no
How about you?
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
Chia Seeds vs Pumpkin Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chia seeds to pumpkin seeds, we picked the chia.
Why?
Both are great! But chia is best.
Note: we’re going to abbreviate them both to “chia” and “pumpkin”, respectively, but we’ll still be referring to the seeds throughout.
In terms of macros, pumpkin has a little more protein and notably higher carbs, whereas chia has nearly 2x the fiber, as well as more fat, and/but they are famously healthy fats. We’ll call this category a subjective win for chia, though you might disagree if you want to prioritize an extra 2g of protein per 100g (for pumpkin) over an extra 16g of fiber per 100g (for chia). Chia is also vastly preferable for omega-3.
When it comes to vitamins, pumpkin is marginally higher in vitamin A, while chia is a lot higher in vitamins B1, B2, B3, B9, C, and E. An easy win for chia.
In the category of minerals, for which pumpkin seeds are so famously a good source, chia has a lot more calcium, copper, iron, magnesium, manganese, phosphorus, and selenium. On the other hand, pumpkin has more potassium and zinc. Still, that’s a 7:2 win for chia.
Adding up the categories makes for a very compelling win for the humble chia seed.
Want to learn more?
You might like to read:
If You’re Not Taking Chia, You’re Missing Out: The Tiniest Seeds With The Most Value
Take care!
Share This Post
Related Posts
-
Creamy Fortifying Cauliflower Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As delicious as it is super-easy to make, this one is full of protein, fiber, healthy fats, and some of the most health-giving spices around.
You will need
- 1 quart low-sodium vegetable stock
- 1 large cauliflower, cut into florets
- 1 large onion, finely chopped
- 2 cans cannellini (or other white) beans, drained and rinsed
- 1 cup raw cashews, soaked in hot water for at least 5 minutes, and drained (if allergic, substitute chickpeas)
- 1 bulb (yes, a whole bulb) garlic, roughly chopped
- 5 tbsp nutritional yeast
- 10 fresh sprigs of thyme (keep them whole!)
- 1 large fresh sprig of rosemary (keep this whole too!)
- zest of 1 lemon
- 1 tbsp red chili flakes
- 1 tbsp black pepper, coarse ground
- 1 tsp MSG or 2 tsp low-sodium salt
- ½ tsp ground turmeric
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Tightly tie up the sprigs of rosemary and thyme with kitchen twine (shining a bright light on it and asking it invasive questions is optional)
2) Heat some olive oil to a medium heat in your biggest sauté pan or similar. Add the onions, and cook for about 10 minutes, stirring as necessary. We are not trying to outright caramelize them here, but we do want them browned a little.
3) Add the garlic and cook for another 2 minutes, stirring frequently.
4) Add the vegetable stock, and stir, ensuring no onion is stuck to the base of the pan. Add the cauliflower, cashews, beans, nooch, pepper, turmeric, and MSG/salt, stirring to combine. Don’t worry if the cauliflower isn’t all submerged; it’ll be fine in a little while.
5) Add the herbs, submerging them in the soup (still tied up bouquet garni style).
6) Bring to a boil, reduce to a simmer and cook for 15–20 minutes; the cauliflower will be soft when it’s ready.
7) Remove the bouquet garni, and blend the soup until thick and creamy. You can do this with an immersion blender, but to get the smoothest soup, you’ll need to use a stand blender. Either ensure yours is safe for hot liquids, or else allow to cool, blend, and reheat later. This is important, as otherwise your blender could explode.
8) Serve, using the lemon zest and chili for the garnish:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Some Surprising Truths About Hunger And Satiety
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How weight bias in health care can harm patients with obesity: Research
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Patients who weigh more than what medical authorities generally consider healthy often avoid seeing doctors for fear of being judged, insulted or misdiagnosed, decades of research find. Meanwhile, academic studies consistently show many health care professionals discriminate against heavier patients and that weight bias can drive people with obesity to gain weight.
Weight bias refers to negative attitudes, stereotypes and discrimination aimed at individuals with excess body fat. When scholars reviewed 41 studies about weight bias in health care, published from 1989 to 2021, they found it comes in many forms: contemptuous language, inappropriate gestures, expressing a preference for thinner patients, avoiding physical touch and eye contact, and attributing all of a person’s health issues to their weight.
“Weight bias has been reported in physicians, nurses, dietitians, physiotherapists, and psychologists, as well as nutritionists and exercise professionals, and it is as pervasive among medical professionals as it is within the general population,” write the authors of the research review, published in 2021 in the journal Obesity.
That’s a problem considering an estimated 4 out of 10 U.S. adults aged 20 years and older have obesity, a complex and often misunderstood illness that the American Medical Association voted in 2013 to recognize as a disease. By 2030, half of U.S. adults will have obesity, researchers project in a 2020 paper in the International Journal of Epidemiology.
Worldwide, the obesity rate among adults aged 18 and older was 13% in 2016, according to the World Health Organization. If current trends continue, the World Obesity Federation projects that, by 2035, 51% of the global population will be living with overweight or obesity.
The harms of weight bias
Weight stigma — the societal devaluation of people perceived to be carrying excess weight — drives weight bias. It’s so physically and emotionally damaging that a panel of 36 international experts issued a consensus statement in 2020 to raise awareness about and condemn it. Dozens of medical and academic organizations, including 15 scholarly journals, endorsed the document, published in Nature Medicine.
The release of a consensus statement is a significant event in research, considering it represents the collective position that experts in a particular field have taken on an issue, based on an analysis of all the available evidence.
Research to date indicates heavier individuals who experience weight bias and stigma often:
- Avoid doctors and other health care professionals, skipping routine screenings as well as needed treatments.
- Change doctors frequently.
- Are at a higher risk for depression, anxiety, mood disorders and other mental health problems.
- Avoid or put off exercise.
- Consume more food and calories.
- Gain weight.
- Have disrupted sleep.
The consensus statement notes that educating health care providers, journalists, policymakers and others about obesity is key to changing the narrative around the disease.
“Weight stigma is reinforced by misconceived ideas about body-weight regulation and lack of awareness of current scientific evidence,” write the experts, led by Francesco Rubino, the chair of metabolic and bariatric surgery at Kings College London.
“Despite scientific evidence to the contrary, the prevailing view in society is that obesity is a choice that can be reversed by voluntary decisions to eat less and exercise more. These assumptions mislead public health policies, confuse messages in popular media, undermine access to evidence-based treatments, and compromise advances in research.”
Weight bias and stigma appear to stimulate the secretion of the stress hormone cortisol and promote weight gain, researchers write in a 2016 paper published in Obesity.
A. Janet Tomiyama, a psychology professor at UCLA who directs the university’s Dieting, Stress, and Health research lab, describes weight stigma as “a ‘vicious cycle’ — a positive feedback loop wherein weight stigma begets weight gain.”
“This happens through increased eating behavior and increased cortisol secretion governed by behavioral, emotional, and physiological mechanisms, which are theorized to ultimately result in weight gain and difficulty of weight loss,” Tomiyama writes in her 2014 paper, “Weight Stigma is Stressful. A Review of Evidence for the Cyclic Obesity/Weight-Based Stigma Model.”
The consensus statement spotlights 13 recommendations for eliminating weight bias and stigma, some of which are specifically aimed at health care providers, the media, researchers or policymakers. One of the recommendations for the health care community: “[Health care providers] specialized in treating obesity should provide evidence of stigma-free practice skills. Professional bodies should encourage, facilitate, and develop methods to certify knowledge of stigma and its effects, along with stigma-free skills and practices.”
The one recommendation for the media: “We call on the media to produce fair, accurate, and non-stigmatizing portrayals of obesity. A commitment from the media is needed to shift the narrative around obesity.”
Why obesity is a complicated disease
It’s important to point out that having excess body fat does not, by itself, mean an individual is unhealthy, researchers explain in a 2017 article in The Conversation, which publishes research-based news articles and essays. But it is a major risk factor for cardiovascular disease, including stroke, as well as diabetes, some types of cancer, and musculoskeletal disorders such as osteoarthritis.
Doctors often look at patients’ body mass index — a number that represents their weight in relation to their height — to gauge the amount of fat on their bodies. A BMI of 18.5 to 24.9 is ideal, according to the U.S. Centers for Disease Control and Prevention. A BMI of 25.0 to 29.9, indicates excess body fat, or “overweight,” while a BMI of 30 and above indicates obesity.
In June, the American Medical Association announced a new policy clarifying how BMI can be used to diagnose obesity. Because it’s an imperfect measure for body fat, the organization suggests BMI be used in conjunction with other measures such as a patient’s waist circumference and skin fold thickness.
Two specialists who have been working for years to dispel myths and misconceptions about obesity are Fatima Cody Stanford, an obesity physician and associate professor at Harvard Medical School, and Rebecca Puhl, the deputy director of the Rudd Center for Food Policy and Obesity at the University of Connecticut.
Cody Stanford has called obesity “a brain disease” because the brain tells the body how much to eat and what to do with the food consumed. One pathway in the brain directs the body to eat less and store less fat, she explains in a February 2023 podcast produced by the American Medical Association.
“For people that signal really great down this pathway, they tend to be very lean, not struggle with their weight in the same way that people that have excess weight do,” she says during the podcast, adding that people with obesity receive signals from an alternate pathway that “tells us to eat more and store more.”
Academic studies demonstrate that a wide variety of factors can affect weight regulation, including sleep quality and duration, gut health, genetics, medication, access to healthy foods and even early life experiences.
For example, a 2020 paper in the journal JAMA Network Open suggests female infants born by cesarean delivery have a higher risk of obesity during adulthood than female infants born by vaginal delivery. The study of 33,226 U.S. women born between 1946 and 1964 found that a cesarean delivery is associated with an 11% higher risk of developing obesity and a 46% higher risk of developing type 2 diabetes.
Scholars have also found that traumatic childhood experiences such as abuse and neglect are linked to adult obesity, according to a research review published in 2020.
Income inequality seems to play a role as well. When researchers from the Johns Hopkins Bloomberg School of Public Health studied the link between income inequality and obesity for a sample of 36,665 U.S. adults, they discovered women with lower incomes are more likely to have obesity than women with higher incomes.
Their analysis indicates the opposite is true for men, whose odds of obesity rise with their income, the researchers write in a 2021 paper in the International Journal of Environmental Research and Public Health.
Weight bias among doctor trainees
While scholars have learned a lot about obesity and weight bias in recent decades, the information might not be reaching people training to become doctors. A study published in October finds that some resident physicians believe obesity to be the result of poor choices and weak willpower.
Researchers asked 3,267 resident physicians who graduated from a total of 49 U.S. medical schools a series of questions to gauge their knowledge of obesity and attitudes toward heavier patients. What they learned: Nearly 40% of resident physicians agreed with the statement, “Fat people tend to be fat pretty much through their own fault.” Almost half agreed with the statement, “Some people are fat because they have no willpower.”
The study also reveals that about one-third of participants said they “feel more irritated when treating an obese patient than a non-obese patient.”
“Notably, more than a quarter of residents expressed slight-to-strong agreement with the item ‘I dislike treating obese patients,’” the researchers write.
Another takeaway from the paper: Resident physicians specializing in orthopedic surgery, anesthesiology and urology expressed the highest levels of dislike of heavier patients. Of the 16 medical specialties represented, residents in family medicine, psychiatry and pediatrics reported the lowest levels of dislike.
Kimberly Gudzune, medical director of the American Board of Obesity Medicine, asserts that doctors and medical students need to be educated about obesity. The topic “is grossly neglected” in medical schools and medical training programs worldwide, research has found.
Many physicians don’t understand obesity, Gudzune explains in a July 2023 interview on the internal medicine podcast “The Curbsiders.”
“I think back to when I was a medical student, when I was a resident, I really didn’t learn much about obesity and how to treat it, yet it’s a problem that affects the majority of our patients,” she tells podcast listeners. “I think there’s a lot of evidence out there showing that primary care physicians don’t really know where to start.”
In 2011, the American Board of Obesity Medicine established a program through which doctors could become certified in obesity medicine. Since then, a total of 6,729 U.S. doctors have earned certification, the vast majority of whom specialize in family and internal medicine.
What health care providers think
The experts who created the consensus statement on weight bias and stigma noted health care providers’ shortcomings in the document. They write that the common themes they discovered in the research include “contemptuous, patronizing, and disrespectful treatment” of patients, a lack of training, poor communication and assumptions about weight gain.
Puhl, the deputy director of the Rudd Center at the University of Connecticut, is a pioneer in weight bias research and one of the experts who wrote the consensus statement. During an episode of “The Leading Voices in Food,” a podcast created by Duke University’s World Food Policy Center, she shares details about what she has learned over the years.
“[Health care providers’] views that patients with obesity are lazy or lacking control, are to blame for their weight or noncompliant with treatment,” she says during the interview. “We know, for example, that some physicians spend less time in their appointments with patients [who] have a larger body size. They give them less education about health. They’re more reluctant to perform certain screenings. They talk about treating patients with obesity as being a greater waste of their time than providing care to thinner patients. And we know that patients seem to be aware of these biases from providers and that can really contribute to patients avoiding health care because they just don’t want to repeat those negative experiences of bias.”
To set the record straight, the experts who wrote the the consensus statement listed the following five common assumptions as being “at odds with a definitive body of biological and clinical evidence.”
1. Body weight = calories in – calories out.
This equation oversimplifies the relationship between body weight and energy consumed and used, the experts write. “Both variables of the equation depend on factors additional to just eating and exercising. For instance, energy intake depends on the amount of food consumed, but also on the amount of food-derived energy absorbed through the gastrointestinal tract, which in turn is influenced by multiple factors, such as digestive enzymes, bile acids, microbiota, gut hormones, and neural signals, none of which are under voluntary control.”
2. Obesity is primarily caused by voluntary overeating and a sedentary lifestyle.
According to the experts, overeating and forgoing exercise might be symptoms of obesity rather than the root causes. There are many possible causes and contributors “including geneticand epigenetic factors, foodborne factors, sleep deprivation and circadian dysrhythmia, psychological stress, endocrine disruptors, medications, and intrauterine and intergenerational effects. These factors do not require overeating or physical inactivity to explain excess weight.” they write.
3. Obesity is a lifestyle choice.
“People with obesity typically recognize obesity as a serious health problem, rather than a conscious choice,” the experts write. “Given the negative effects of obesity on quality of life, the well-known risks of serious complications and reduced life expectancy associated with it, it is a misconception to define obesity as a choice.”
4. Obesity is a condition, not a disease.
The criteria generally used to determine disease status “are clearly fulfilled in many individuals with obesity as commonly defined, albeit not all,” the experts explain. “These criteria include specific signs or symptoms (such as increased adiposity), reduced quality of life, and/or increased risk of further illness, complications, and deviation from normal physiology — or well-characterized pathophysiology (for example, inflammation, insulin resistance, and alterations of hormonal signals regulating satiety and appetite).”
5. Severe obesity is usually reversible by voluntarily eating less and exercising more.
“A large body of clinical evidence has shown that voluntary attempts to eat less and exercise more render only modest effects on body weight in most individuals with severe obesity,” the experts write. “When fat mass decreases, the body responds with reduced resting energy expenditure and changes in signals that increase hunger and reduce satiety (for example, leptin, ghrelin). These compensatory metabolic and biologic adaptations promote weight regain and persist for as long as persons are in the reduced-energy state, even if they gain some weight back.”
Health care facility improvements
The expert panel also determined that many health care facilities aren’t equipped to treat people with obesity. Examination gowns, blood pressure cuffs, chairs and examination tables often are too small, patients have reported.
When researchers from the University of Minnesota, Minneapolis Veterans Affairs Medical Center and Mayo Clinic studied the quality of care that patients with obesity receive, they learned that a clinic’s physical environment can have a big effect on a patient’s experience.
They write in a 2015 study published in Obesity Reviews: “Waiting room chairs with armrests can be uncomfortable or too small. Equipment such as scales, blood pressure cuffs, examination gowns and pelvic examination instruments are often designed for use with smaller patients. When larger alternatives are not available, or are stored in a place that suggests infrequent use, it can signal to patients that their size is unusual and that they do not belong. These experiences, which are not delivered with malicious intent, can be humiliating.”
When medical equipment is the wrong size, it may not work correctly. For instance, chances are high that a blood pressure reading will be inaccurate if a health care professional uses a blood pressure cuff that’s too small on a patient with obesity, a 2022 paper finds.
To create a comfortable environment for patients with high body weights, the Rudd Center for Food Policy and Obesity recommends that health care facilities provide, among other things, extra-large exam gowns, chairs that can support more than 300 pounds and do not have arms, and wide exam tables that are bolted to the floor so they don’t move.
The consensus statement also recommends improvements to health care facilities.
“Given the prevalence of obesity and obesity-related diseases,” the 36 international experts write, “appropriate infrastructure for the care and management of people with obesity, including severe obesity, must be standard requirement for accreditation of medical facilities and hospitals.”
Source list:
Weight Bias Among Health Care Professionals: A Systematic Review and Meta-Analysis
Blake J. Lawrence; et al. Obesity, November 2021.Joint International Consensus Statement for Ending Stigma of Obesity
Francesco Rubino, et al. Nature Medicine, March 2020.Perceived Weight Discrimination and Chronic Biochemical Stress: A Population-Based Study Using Cortisol in Scalp Hair
Sarah E. Jackson, Clemens Kirschbaum and Andrew Steptoe. Obesity, December 2016.Weight Stigma is Stressful. A Review of Evidence for the Cyclic Obesity/Weight-Based Stigma Model
A. Janet Tomiyama. Appetite, November 2014.Association of Birth by Cesarean Delivery with Obesity and Type 2 Diabetes Among Adult Women
Jorge E. Chavarro. JAMA Network Open, April 2020.Adverse Childhood Experiences and Adult Obesity: A Systematic Review of Plausible Mechanisms and Meta-Analysis of Cross-Sectional Studies
David A. Wiss and Timothy D. Brewerton. Physiology & Behavior, September 2020.Income Inequality and Obesity among U.S. Adults 1999–2016: Does Sex Matter?
Hossein Zare, Danielle D. Gaskin and Roland J. Thorpe Jr. International Journal of Environmental Research and Public Health, July 2021.Comparisons of Explicit Weight Bias Across Common Clinical Specialties of U.S. Resident Physicians
Samantha R. Philip, Sherecce A. Fields, Michelle Van Ryn and Sean M. Phelan. Journal of General Internal Medicine, October 2023.Impact of Weight Bias and Stigma on Quality of Care and Outcomes for Patients with Obesity
S.M. Phelan; et al. Obesity Reviews, April 2015.One Size Does Not Fit All: Impact of Using A Regular Cuff For All Blood Pressure Measurements
Tammy. M. Brady; et al. Circulation, April 2022.This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Knowledge That Harvard Medical School’s Clinical Instructor Dr. Monique Tello Thinks Everyone SHOULD Have About Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anyone (who has not had a double mastectomy, anyway) can get breast cancer.
Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
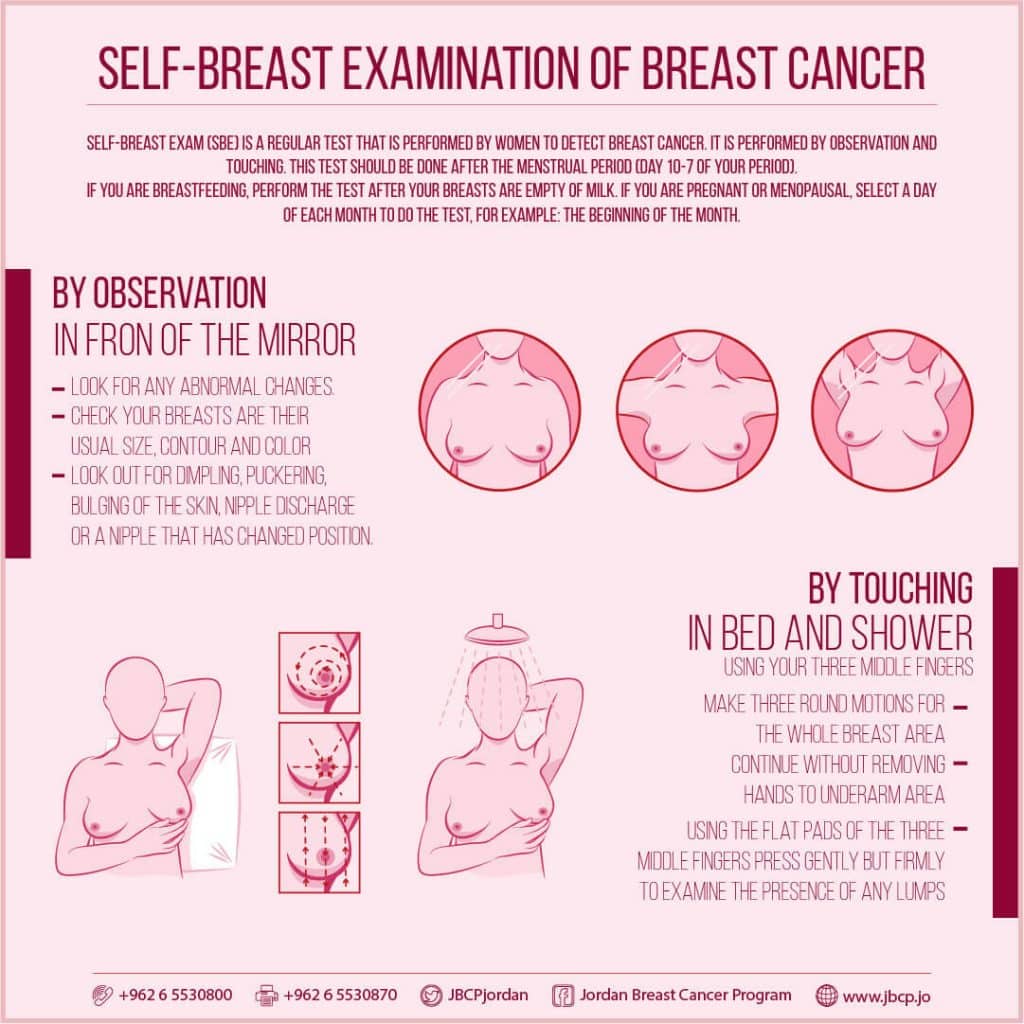
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:
This graphic created by the Jordan Breast Cancer Program (check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it.
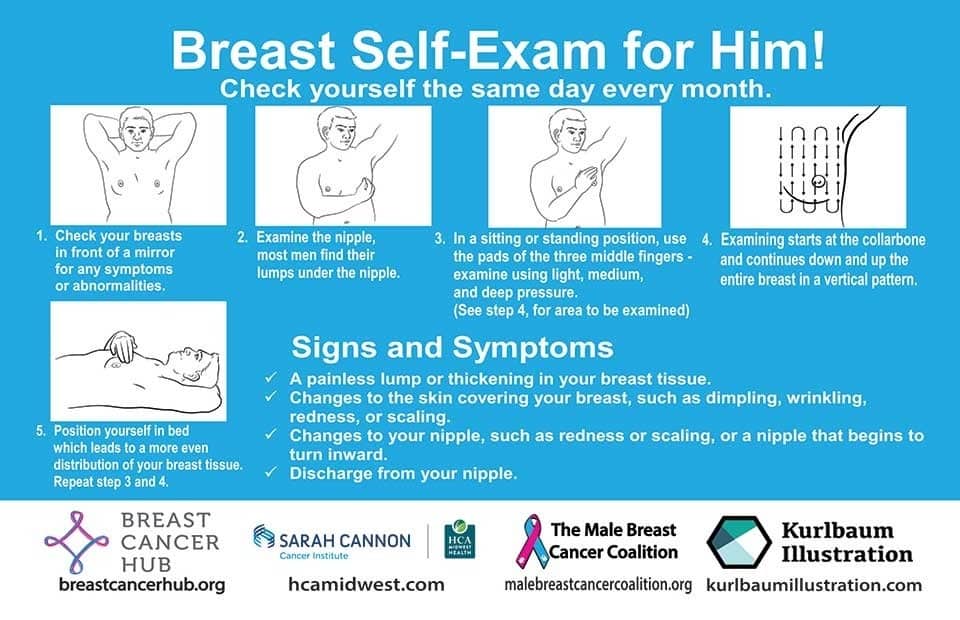
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?
So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to! Take care of yourself; you’re important.
Pssst! Did you scroll past the diagrams, looking for the online 4-minute test promised by the subtitle? If so, scroll back up; the link is in the middle!
Harvard Medical School’s Clinical Instructor’s Five-Point Plan for Heart Health
Dr. Monique Tello, M.D., M.P.H., is a practicing physician at Massachusetts General Hospital, director of research and academic affairs for the MGH DGM Healthy Lifestyle Program, clinical instructor at Harvard Medical School, and author of the evidence-based lifestyle change guide Healthy Habits for Your Heart.
Here are what she says are the five most important factors to help keep your ticker ticking:
5. Have (at most) a moderate alcohol intake! While there are polyphenols such as resveratrol in red wine that could boost heart health, there’s so little per glass that you may need 100–1000 glasses to get the dosage that provides benefits in mouse studies. If you’re not a mouse, it may not be as beneficial, and Dr. Tello recommends drinking no more than one glass per day of any alcohol. What constitutes a glass? It varies from one kind of drink to another, so here’s a handy guide.
4. Don’t smoke. Best of all to never start. But if you did, quit. Simple as that. There is no healthy amount of smoking. While paradoxically, quitting smoking may of course be stressful to you, the long term gains are considered more than worth it. As with all advice, do consult your own physician for guidance, as individual circumstances may vary, and that may change the best approach for you.
3. Maintain a healthy body weight. While BMI (Body Mass Index) is not a perfect system, it’s a system in popular use, and Dr. Tello recommends keeping a BMI between 18.5 and 24.9.
What’s your BMI? It takes into account your height and weight; here’s a Quick BMI Calculator for your convenience.
2. Keep a healthy level of physical activity—which ideally means at least 30 minutes per day vigorous activity, but obviously if you’re not used to this, take it slowly and build up over time. Even just small lifestyle changes (walking where possible, taking the stairs instead of the elevator where possible, etc) can add up to a big difference.
1. Enjoy a healthy diet. This is the single most important thing, and the best modern scientific consensus holds that the best diet contains plenty of vegetables, fruits and nuts, whole grains, and omega-3 fatty acids, while it avoids processed meats, sugar-sweetened beverages, trans fats (what are trans fats?), and too much sodium.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: