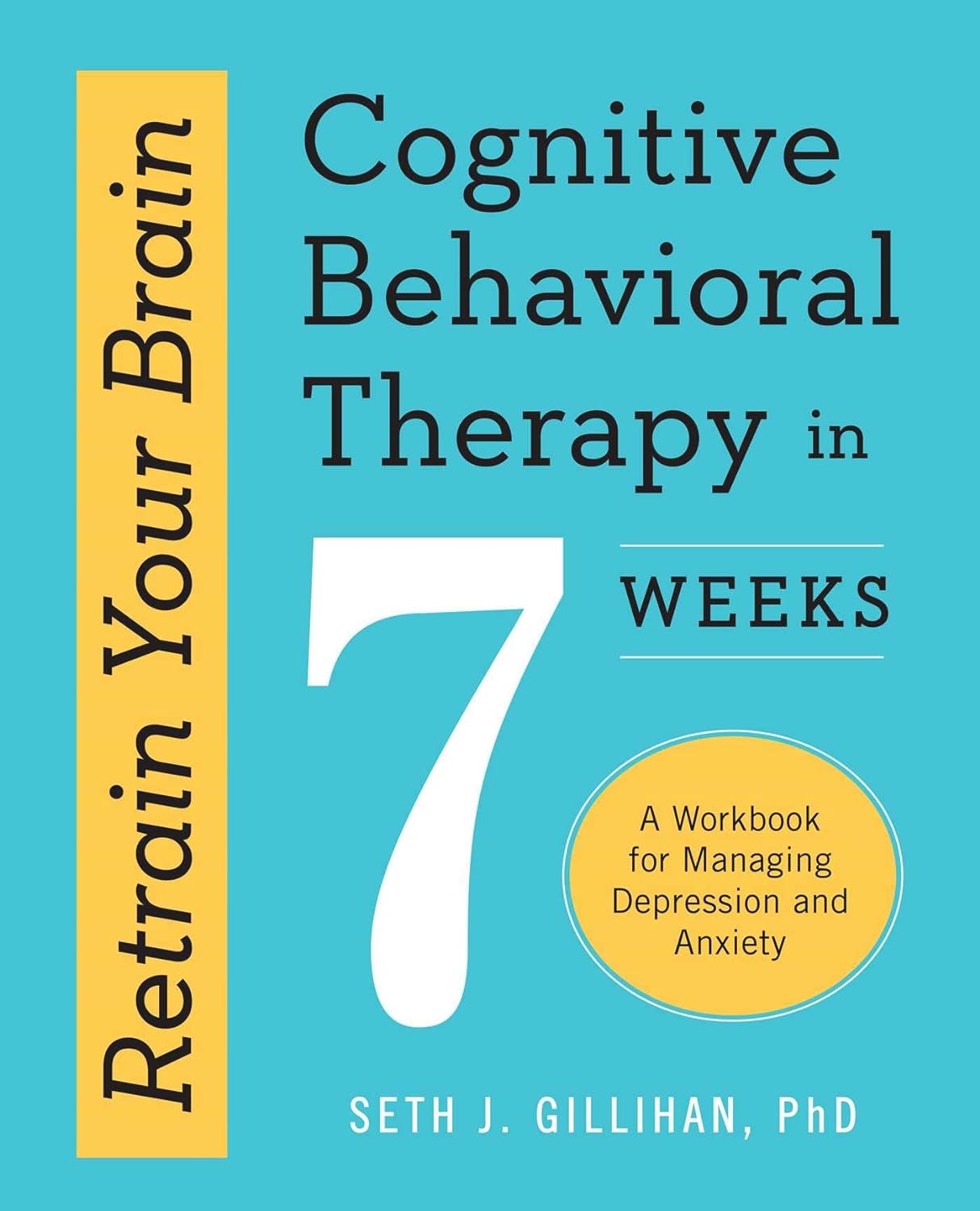
Retrain Your Brain – by Dr. Seth Gillihan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
15-Minute Arabic”, “Sharpen Your Chess Tactics in 24 Hours”, “Change Your Life in 7 Days”, “Cognitive Behavioral Therapy in 7 weeks”—all real books from this reviewer’s shelves.
The thing with books with these sorts of time periods in the titles is that the time period in the title often bears little relation to how long it takes to get through the book. So what’s the case here?
You’ll probably get through it in more like 7 days, but the pacing is more important than the pace. By that we mean:
Dr. Gillihan starts by assuming the reader is at best “in a rut”, and needs to first pick a direction to head in (the first “week”) and then start getting one’s life on track (the second “week”).
He then gives us, one by one, an array of tools and power-ups to do increasingly better. These tools aren’t just CBT, though of course that features prominently. There’s also mindfulness exercises, and holistic / somatic therapy too, for a real “bringing it all together” feel.
And that’s where this book excels—at no point is the reader left adrift with potential stumbling-blocks left unexamined. It’s a “whole course”.
Bottom line: whether it takes you 7 hours or 7 months, “Cognitive Behavioral Therapy in 7 Weeks” is a CBT-and-more course for people who like courses to work through. It’ll get you where you’re going… Wherever you want that to be for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cynthia’s Thoughts on Intermittent Fasting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Myth of Breakfast and Snacking
Here at 10almonds we love addressing misconceptions in the health world.
When it comes to eating habits and fasting, we’ve written our own pieces on how to break your fast (otherwise known as break-fast, or breakfast), alongside a general breakdown of intermittent fasting, and a much-requested piece on fasting specifically for women.
Cynthia Thurlow, though, instead of just writing a few articles, has dedicated the majority of her working years to intermittent fasting and, in her TEDx talk (below), makes a strong argument challenging the long-held belief that breakfast is the most important meal of the day.
Cynthia Thurlow’s Two Main Points
Thurlow argues that it’s not what you eat but when you eat that has a more profound impact on health and aging. And she argues this is crucial regardless of your age.
Complementing her views on fasting are her views on snacking; she argues that snacking all day long is outdated advice and can overtax the digestive system, leading to various health issues.
Practical Tips for Starting Intermittent Fasting
To begin intermittent fasting, Thurlow suggests starting with a 12-13 hour fasting window and gradually increasing it to 16 hours.
In terms of food choice, she recommends eating whole, unprocessed foods during eating periods as well as staying well-hydrated with water, coffee, or tea.
But you won’t see results immediately; Thurlow advises giving the strategy a solid 30 days to see results and consulting a healthcare provider if there are any existing health conditions.
You can dive deeper and join the 15 million other people who have listened to her thoughts on fasting by watching her TEDx talk below:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Strawberries vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing strawberries to cherries, we picked the cherries.
Why?
Both are great, and an argument could be made for either! But here’s our rationale:
In terms of macros, as with most fruits they are both mostly water, and have similar carbs and fiber. Nominally, cherries have the lower glycemic index, so we could call this category nominally a win for cherries, but honestly, they’re both low-GI foods and nobody is getting metabolic disease from eating strawberries, so it’s fairer to consider this category a tie.
Looking at the vitamins, strawberries have more of vitamins C, B9, E, and K, while cherries have more of vitamins A, B1, B2, B3, B5, and choline. Thus, a modest win for cherries here.
When it comes to minerals, strawberries see their day: strawberries have more iron, magnesium, manganese, and phosphorus, while cherries have more calcium, copper, and potassium. By the numbers, a win for strawberries.
So far, so tied!
What swings it into cherries’ favor is cherries’ slew of specific phytochemical benefits, including cherry-specific anti-inflammatory properties, sleep-improving abilities, and post-exercise recovery boosts, as well as anti-diabetic benefits above and beyond the normal “this is a fruit” level.
In short, both are very respectable fruits, but cherries have some extra qualities that are just special.
Of course, as ever, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Cherries’ Health Benefits Simply Pop
Enjoy!
Share This Post
-
Keep Cellulite At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Does anything actually get rid of cellulite? Nothing seems to❞
Let’s get the bad news over with in one go:
Nothing (that the scientific world currently knows of) can get rid of cellulite permanently, nor completely guard against it proactively. Which, given that it affects up to 98% of women to some degree, and often shows up not long after puberty (though it can appear at any time and often increases later in life), any pre-emptive health regime would need to be started as a child in any case.
As with many things that predominantly affect women, the world of medicine isn’t entirely sure what causes it, let alone how to effectively treat it.
Obviously hormones are implicated, namely estrogen.
Obviously adiposity is implicated, because one can’t have dimples in one’s fat if one doesn’t have enough fat to dimple.
Other hypothesized contributory factors include genetics, poor diet, inactivity, unhealthy lifestyle (in ways not previously mentioned, e.g. use of alcohol, tobacco, etc), accumulated toxins, and pregnancy.
Here’s an old paper (from 2004); today’s reviews say pretty much the same thing, but we love how succinctly (albeit, somewhat depressingly) this abstract states how little we know and how little we can do:
Cellulite: a review of its physiology and treatment
However, all is not lost!
There are some things that can affect how much cellulite we get, and there are some things that can reduce it, and even some things that can get rid of it completely—albeit temporarily.
First, a quick refresher on what it actually is, physiologically speaking: cellulite occurs when connective tissue bands pull the skin down in places, where fat tissue has been able to squeeze through. One of the reasons it is hypothesized women get this more than men is because our fat is not merely different in distribution and overall percentage, but also in how the fat cells stack up; we generally have have of a vertical stacking structure going on, while men generally have a more horizontal structure. This means that it can be easier for ours to get moved about differently, causing the connective tissue to pull on the skin unevenly in places.
With that in mind…
Prevention is, as we say, probably impossible if your body is running on estrogen. However, those contributory factors we mentioned above? Most of those are modifiable, including these things that it is hypothesized can reduce it:
Diet: as it seems to be worsened by inflammation (what isn’t?), an anti-inflammatory diet is recommended.
Exercise: there are three things here: 1) exercises to improve circulation and thus the body’s ability to sort things out by itself 2) HIIT exercise to reduce body fat percentage, if one has a high enough starting body fat percentage for that to be a healthy goal 3) mobility exercises, to ensure our connective tissues are the right amount of mobile.
Creams and lotions
These reduce the superficial appearance of cellulite, without actually treating the thing itself. Mostly they are caffeine-based, which when used topically increases blood flow and works as a local diuretic, reducing the water content of the fat cells, diminishing the appearance of the cellulite by making each fat cell physically smaller (while still containing the same amount of fat, and it’ll bounce back in size as soon as the body can restore osmotic balance).
Medical procedures
There are too many of these to discuss them all separately, but they all work on the principle of breaking up the tough bands of connective tissue to eliminate the dimpling of cellulite.
The methods they use vary from ultrasound to cryolipolysis to lasers to “vacuum-assisted precise tissue release”, which involves a suction pump and a multipronged robotic assembly with needles to administer anaesthetic as it goes and small blades to cut the connective tissues under the skin:
Tissue Stabilized–Guided Subcision for the Treatment of Cellulite
That last one definitely sounds like the least fun, but it’s also the only one that doesn’t take months to maybe see results.
Cellulite can and almost certainly will come back after all of these.
Home remedies
Aside from at-home versions of the above (not the robots with vacuum pumps and needles and microblades, hopefully, but for example homemade caffeine creams), and of course diet and exercise which can be considered “home remedies”, there are two more things worth mentioning:
Dry brushing: using a body brush to, as the name suggests, simply brush one’s skin. The “dry” aspect here is simply that it’s not done in the bath or shower; it’s done while dry. It can improve local circulation of blood and lymph, allowing for better detoxification and redistribution of needed bodily resources.
Here’s an example dry brushing body brush on Amazon; this writer has one and hates it, but I’ve also tried with other kinds of brush and hate them too, so it seems to be a me thing rather than a brush thing, and I have desisted in trying, now. Maybe you will like it better; many people do.
Self-massage: or massage by someone else, if that’s an option for you and you prefer. In this case, it works by a different mechanism than dry brushing; this time it’s working by the same principle as the medical techniques described in the previous section; it’s physically breaking down the toughened bits of connective tissue.
Here’s an example wooden massage roller on Amazon; this writer has one and loves it; it’s sooooooo good. I got it as a matter of general maintenance for my fascia, but it’s also very good if I get a muscular pain now and again. As for cellulite, I personally get just a little cellulite sometimes (in the backs of my thighs), and whenever I use this regularly, it goes away for at least a while.
A quick note in closing
Cellulite is normal for women and is not unhealthy. Much like gray hair for example, it’s something that can be increased by poor health, but the thing itself isn’t intrinsically unhealthy, and most of us get it to some degree at some point.
Nevertheless, aesthetic factors can also have a role to play in mental health, and we tend to feel best when we like the way our body looks. If for you that means wanting less/no cellulite, then the above are some ways towards that.
As a bonus, most of the nonmedical options are directly good for the physical health anyway, so doing them is of course good.
In particular that last one (the wooden massage roller), because that connective tissue we talked about? It matters for a lot more than just cellulite, and is heavily implicated in a lot of kinds of chronic pain, so it pays to keep it in good health:
Fascia: Why (And How) You Should Take Care Of Yours
(that article, also written by this same writer by the way, suggests a vibrating foam roller—those are very popular; I just really love my wooden one, and find it more effective)
Take care!
Share This Post
Related Posts
-
Fruit & Veg In The Fridge: Pros & Cons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝What effect does refrigeration have on the nutritional value of fruit and vegetables??❞
It’s difficult to give a single definitive answer, because naturally there are a lot of different fruits and vegetables, and a lot of different climates. The answer may be different for tomatoes in Alaska vs bananas in Arizona!
However, we can still generalize at least somewhat
Refrigeration will generally slow down any degradation process, and in the case of fruit and vegetables, that can mean slowing down their “ripening” too, as applicable.
However…
Refrigeration will also impede helpful bioactivity too, and that includes quite a list of things.
Here’s a good study that’s quite illustrative; we’d summarize the conclusions but the rather long title already does that nicely:
So, this really is a case of “there are pros and cons, but probably more cons on balance”.
In practical terms, a good take-away from this can be twofold:
- don’t keep fruit and veg in the fridge unless the ambient temperature really requires it
- if the ambient temperature does require it, it’s best to get the produce in fresh each day if that’s feasible, to minimize time spent in the fridge
An extra thing not included there: often when it comes to the spoilage of fruit and veg, the problem is that it respires and oxidizes; reducing the temperature does lower the rate of those, but often a far better way is to remove the oxygen. So for example, if you get carried away and chop too many carrot batons for your hummus night, then putting them in a sealed container can go a long way to keeping them fresh.
See also: How Does the Nutritional Value of Fruits and Vegetables Change Over Time?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Vagus Nerve (And How You Can Make Use Of It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Vagus Nerve: The Brain-Gut Highway
The longest cranial nerve is the vagus nerve; it runs all the way from your brain to your colon. It’s very important, and (amongst other tasks) it largely regulates your parasympathetic nervous system, and autonomous functions like:
- Breathing
- Heart rate
- Vasodilation & vasoconstriction
- Blood pressure
- Reflex actions (e.g. coughing, sneezing, swallowing, vomiting, hiccuping)
That’s great, but how does knowing about it help us?
Because of vagal maneuvers! This means taking an action to stimulate the vagus nerve, and prompt it to calm down various bodily functions that need calming down. This can take the form of:
- Massage
- Electrostimulation
- Diaphragmatic breathing
Massage is perhaps the simplest; “vagus” means “wandering”, and the nerve is accessible in various places, including behind the ears. That’s the kind of thing that’ easier to show than tell, though, so we’ll include a video at the end.
Electrostimulation is the fanciest, and has been used to treat migraines and cluster headaches. Check out, for example:
Update on noninvasive neuromodulation for migraine treatment-Vagus nerve stimulation
Diaphragmatic breathing means breathing from the diaphragm—the big muscular tissue that sits under your lungs. You might know it as “abdominal breathing”, and refers to breathing “to the abdomen” rather than merely to the chest.
Even though your lungs are obviously in your chest not your abdomen, breathing with a focus on expanding the abdomen (rather than the chest) when breathing in, will result in much deeper breathing as the diaphragm allows the lungs to fill downwards as well as outwards.
Why this helps when it comes to the vagus nerve is simply that the vagus nerve passes by the diaphragm, such that diaphragmatic breathing will massage the vagus nerve deep inside your body.
More than just treating migraines
Vagus nerve stimulation has also been researched and found potentially helpful for managing:
- Depression, inflammation, and heart disease
- Diabetes and glycemic issues in general
- Multiple sclerosis and autoimmune disease in general
- Alzheimer’s disease and dementia in general
- Rheumatoid arthritis (we already mentioned inflammation and autoimmune diseases, but this is an interesting paper so we included it)
All this is particularly important as we get older, because vagal response reduces with age, and vagus nerve stimulation, which improves vagal tone, makes it easier not just to manage the aforementioned maladies, but also simply to relax more easily and more deeply.
See: Influence of age and gender on autonomic regulation of heart
We promised a video for the massage, so here it is:
! Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Reason You’re Alone
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you are feeling lonely, then there are likely reasons why, as Kurtzgesagt explains:
Why it happens and how to fix it
Many people feel lonely and disconnected, often not knowing how to make new friends. And yet, social connection strongly predicts happiness, while lack of it is linked to diseases and a shorter life.
One mistake that people make is thinking it has to be about shared interests; that can help, but proximity and shared time are much more important.
Another stumbling block for many is that adult responsibilities and distractions (work, kids, technology) often take priority over friendships—but loneliness is surprisingly highest among young people, worsened by the pandemic’s impact on social interactions.
And even when friendships are made, they fade without attention, often accidentally, impacting both people involved. Other friendships can be lost following big life changes such as moving house or the end of a relationship. And for people above a certain advanced age, friendship groups can shrink due to death, if one’s friends are all in the same age group.
But, all is not lost. We can make friends with people of any age, and old friendships can be revived by a simple invitation. We can also take a “build it and they will come” approach, by organizing events and being the one who invites others.
It’s easy to fear rejection—most people do—but it’s worth overcoming for the potential rewards. That said, building friendships requires time, patience, caring about others, and being open about yourself, which can involve a degree of vulnerability too.
In short: be laid-back while still prioritizing friendships, show genuine interest, and stay open to social opportunities.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Beat Loneliness & Isolation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: