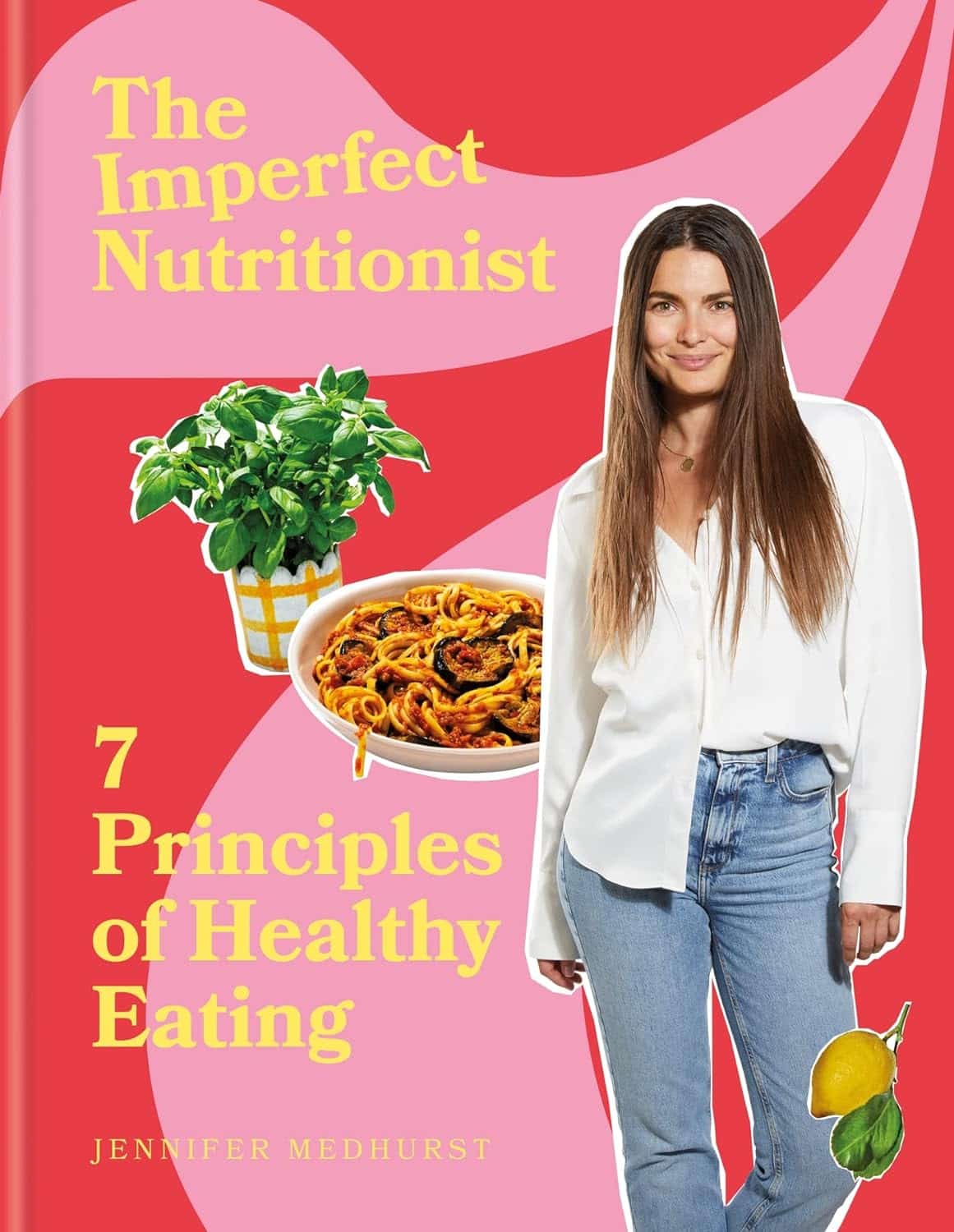
The Imperfect Nutritionist – by Jennifer Medhurst
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The idea of the “imperfect nutritionist” is to note that we’re all different with slightly different needs and sometimes very different preferences (or circumstances!) and having a truly perfect diet is probably a fool’s errand. Should we just give up, then? Not at all:
What we can do, Medhust argues, is find what’s best for us, realistically.
It’s better to have an 80% perfect diet 80% of the time, than to have a totally perfect diet for four and a half meals before running out of steam (and ingredients).
As for the “seven principles” mentioned in the title… we’re not going to keep those a mystery; they are:
- Focusing on wholefood
- Being diverse
- Knowing your fats
- Including fermented, prebiotic and probiotic foods
- Reducing refined carbohydrates
- Being aware of liquids
- Eating mindfully
The first part of the book is a treatise on how to implement those principles in your diet generally; the second part of the book is a recipe collection—70 recipes, with “these ingredients will almost certainly be available at your local supermarket” as a baseline. No instances of “the secret to being a good chef is knowing how to source fresh ingredients; ask your local greengrocer where to find spring-harvested perambulatory truffle-cones” here!
Basically, it focusses on adding healthy foods per your personal preferences and circumstances, and building these up into a repertoire of meals that will keep you and your family happy and healthy.
Pick Up Your Copy Of The Imperfect Nutritionist From Amazon Today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
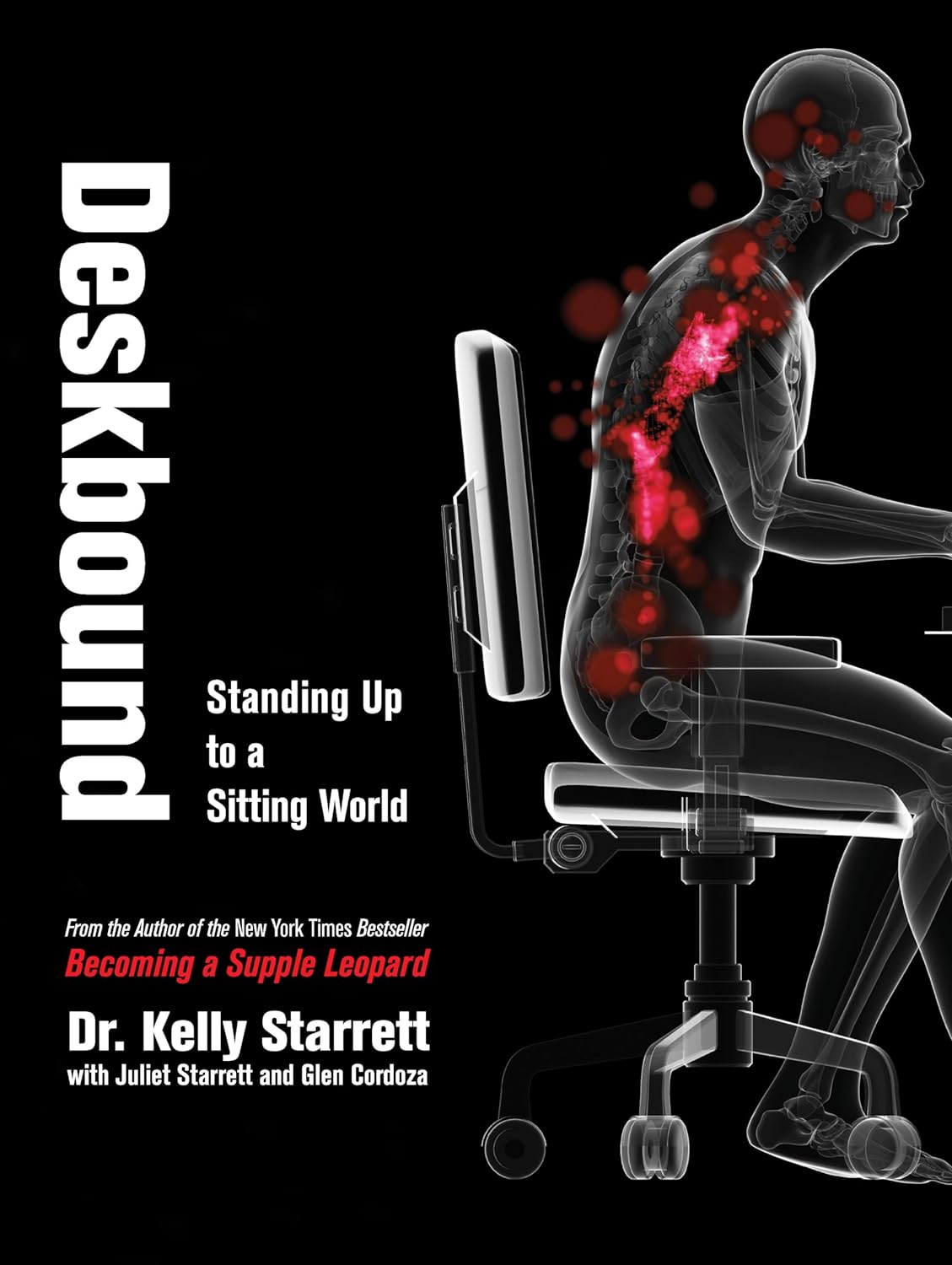
Deskbound – by Kelly Starrett and Glen Cordoza
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all heard that “sitting is the new smoking”, and whether or not that’s an exaggeration (the jury’s out), one thing that is clear is that sitting is very bad.
Popular advice is “here’s how to sit with good posture and stretch your neck sometimes”… but that advice tends to come from companies that pay people to sit for a long time. They might not be the a very unbiased source.
Starrett and Cordoza offer better. After one opening chapter covering the multifarious ways sitting ruins our health, the rest of the book is all advice, covering:
- The principles of how the body is supposed to be
- The most important movements that we should be doing
- A dynamic workstation setup
- This is great, because “get a standing desk” tends to present more questions than answers, and can cause as much harm as good if done wrong
- The authors also cover how to progressively cut down on sitting, rather than try to go cold-turkey.
- They also recognize that not everyone can stand at all, and…
- Optimizing the sitting position, for when we must sit
- Exercises to maintain our general mobility and compensate about as well as we can for the body-unfriendly nature of modern life.
The book is mostly explanations, so at 682 pages, you can imagine it’s not just “get up, lazybones!”. Rather, things are explained in such detail (and with many high-quality medical diagrams) so that we can truly understand them.
Most of us have gone through life knowing we should have “better posture” and “move more”… but without the details, that can be hard to execute correctly, and worse, we can even sabotage our bodies unknowingly with incorrect form.
This book straightens all that out very comprehensively, and we highly recommend it.
Share This Post
-
How Old Is Too Old For HRT?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I think you guys do a great job. Wondering if I can suggest a topic? Older women who were not offered hormone replacement therepy because of a long term study that was misread. Now, we need science to tell us if we are too old to benefit from begininng to take HRT. Not sure how old your readers are on average but it would be a great topic for older woman. Thanks❞
Thank you for the kind words, and the topic suggestion!
About the menopause and older age thereafter
We’ve talked a bit before about the menopause, for example:
What You Should Have Been Told About The Menopause Beforehand
And we’ve even discussed the unfortunate social phenomenon of post-menopausal women thinking “well, that’s over and done with now, time to forget about that”, because spoiler, it will never be over and done with—your body is always changing every day, and will continue to do so until you no longer have a body to change.
This means, therefore, that since changes are going to happen no matter what, the onus is on us to make the changes as positive (rather than negative) as possible:
Menopause, & When Not To Let Your Guard Down
About cancer risk
It sounds like you know this one, but for any who were unaware: indeed, there was an incredibly overblown and misrepresented study, and even that was about older forms of HRT (being conjugated equine estrogens, instead of bioidentical estradiol):
As for those who have previously had breast cancer or similar, there is also:
The Hormone Therapy That Reduces Breast Cancer Risk & More
Is it too late?
Fortunately, there is a quick and easy test to know whether you are too old to benefit:
First, find your pulse, by touching the first two fingers of one hand, against the wrist of the other. If you’re unfamiliar with where to find the pulse at the wrist, here’s a quick explainer.
Or if you prefer a video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Did you find it?
Good; in that case, it’s not too late!
Scientists have tackled this question, looking at women of various ages, and finding that when comparing age groups taking HRT, disease risk changes do not generally vary much by age i.e., someone at 80 gets the same relative benefit from HRT as someone at 50, with no extra risks from the HRT. For example, if taking HRT at 50 reduces a risk by n% compared to an otherwise similar 50-year-old not on HRT, then doing so at 80 reduces the same risk by approximately the same percentage, compared to an otherwise similar 80-year-old not on HRT.
There are a couple of exceptions, such as in the case of already having advanced atherosclerotic lesions (in which specific case HRT could increase inflammation; not something it usually does), or in the case of using conjugated equine estrogens instead of modern bioidentical estradiol (as we talked about before).
Thus, for the most part, HRT is considered safe and effective regardless of age:
How old is too old for hormone therapy?
👆 that’s from 2015 though, so how about a new study, from 2024?
❝Compared with never use or discontinuation of menopausal hormone therapy after age 65 years, the use of estrogen monotherapy beyond age 65 years was associated with significant risk reductions in mortality (19% or adjusted hazards ratio, 0.81; 95% CI, 0.79-0.82), breast cancer (16%), lung cancer (13%), colorectal cancer (12%), congestive heart failure (CHF) (5%), venous thromboembolism (3%), atrial fibrillation (4%), acute myocardial infarction (11%), and dementia (2%).❞
❝Among senior Medicare women, the implications of menopausal hormone therapy use beyond age 65 years vary by types, routes, and strengths. In general, risk reductions appear to be greater with low rather than medium or high doses, vaginal or transdermal rather than oral preparations, and with estradiol rather than conjugated estrogen.❞
Read in full: Use of menopausal hormone therapy beyond age 65 years and its effects on women’s health outcomes by types, routes, and doses
As for more immediately-enjoyable benefits (improved mood, healthier skin, better sexual function, etc), yes, those also are benefits that people enjoy at least into their eighth decade:
See: Use of hormone therapy in Swedish women aged 80 years or older
What about…
Statistically speaking, most people who take HRT have a great time with it and consider it life-changing in a good way. However, nothing is perfect; sometimes going on HRT can have a shaky start, and for those people, there may be some things that need addressing. So for that, check out:
HRT Side Effects & Troubleshooting
And also, while estrogen monotherapy is very common, it is absolutely worthwhile to consider also taking progesterone alongside it:
Progesterone Menopausal HRT: When, Why, And How To Benefit
Enjoy!
Share This Post
-
What’s behind rising heart attack rates in younger adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Deaths from heart attacks have been in decline for decades, thanks to improved diagnosis and treatments. But, among younger adults under 50 and those from communities that have been marginalized, the trend has reversed.
More young people have suffered heart attacks each year since the 2000s—and the reasons why aren’t always clear.
Here’s what you need to know about heart attack trends in younger adults.
Heart attack deaths began declining in the 1980s
Heart disease has been a leading cause of death in the United States for more than a century, but rates have declined for decades as diagnosis and treatments improved. In the 1950s, half of all Americans who had heart attacks died, compared to one in eight today.
A 2023 study found that heart attack deaths declined 4 percent a year between 1999 and 2020.
The downward trend plateaued in the 2000s as heart attacks in young adults rose
In 2012, the decline in heart disease deaths in the U.S. began to slow. A 2018 study revealed that a growing number of younger adults were suffering heart attacks, with women more affected than men. Additionally, younger adults made up one-third of heart attack hospitalizations, with one in five heart attack patients being under 40.
The following year, data showed that heart attack rates among adults under 40 had increased steadily since 2006. Even more troubling, young patients were just as likely to die from heart attacks as patients more than a decade older.
Why are more younger adults having heart attacks?
Heart attacks have historically been viewed as a condition that primarily affects older adults. So, what has changed in recent decades that puts younger adults at higher risk?
Higher rates of obesity, diabetes, and high blood pressure
Several leading risk factors for heart attacks are rising among younger adults.
Between 2009 and 2020, diabetes and obesity rates increased in Americans ages 20 to 44.During the same period, hypertension, or high blood pressure, rates did not improve in younger adults overall and worsened in young Hispanic people. Notably, young Black adults had hypertension rates nearly twice as high as the general population.
Hypertension significantly increases the risk of heart attack and cardiovascular death in young adults.
Increased substance use
Substance use of all kinds increases the risk of cardiovascular issues, including heart attacks. A recent study found that cardiovascular deaths associated with substance use increased by 4 percent annually between 1999 and 2019.
The rise in substance use-related deaths has accelerated since 2012 and was particularly pronounced among women, younger adults (25-39), American Indians and Alaska Natives, and those in rural areas.
Alcohol was linked to 65 percent of the deaths, but stimulants (like methamphetamine) and cannabis were the substances associated with the greatest increase in cardiovascular deaths during the study period.
Poor mental health
Depression and poor mental health have been linked to cardiovascular issues in young adults. A 2023 study of nearly 600,000 adults under 50 found that depression and self-reported poor mental health are a risk factor for heart disease, regardless of socioeconomic or other cardiovascular risk factors.
Adults under 50 years consistently report mental health conditions at around twice the rate of older adults. Additionally, U.S. depression rates have trended up and reached an all-time high in 2023, when 17.8 percent of adults reported having depression.
Depression rates are rising fastest among women, adults under 44, and Black and Hispanic populations.
COVID-19
COVID-19 can cause real, lasting damage to the heart, increasing the risk of certain cardiovascular diseases for up to a year after infection. Vaccination reduces the risk of heart attack and other cardiovascular events caused by COVID-19 infection.
The first year of the pandemic marked the largest single-year spike in heart-related deaths in five years, including a 14 percent increase in heart attacks. In the second year of the pandemic, heart attacks in young adults increased by 30 percent.
Heart attack prevention
Not every heart attack is preventable, but everyone can take steps to reduce their risks. The American Heart Association recommends managing health conditions that increase heart disease risk, including diabetes, obesity, and high blood pressure.
Lifestyle changes like improving diet, reducing substance use, and increasing physical activity can also help reduce heart attack risk.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Cardiac Failure Explained – by Dr. Warrick Bishop
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The cover of this book makes it look like it’ll be a flashy semi-celebrity doctor keen to sell his personalized protocol, along with eleventy-three other books, but actually, what’s inside this one is very different:
We (hopefully) all know the basics of heart health, but this book takes it a lot further. Starting with the basics, then the things that it’s easy to feel like you should know but actually most people don’t, then into much more depth.
The format is much more like a university textbook than most pop-science books, and everything about the way it’s written is geared for maximum learning. The one thing it does keep in common with pop-science books as a genre is heavy use of anecdotes to illustrate points—but he’s just as likely to use tables, diagrams, callout boxes, emboldening of key points, recap sections, and so forth. And for the most part, this book is very information-dense.
Dr. Bishop also doesn’t just stick to what’s average, and talks a lot about aberrations from the norm, what they mean and what they do and yes, what to do about them.
On the one hand, it’s more information dense than the average reader can reasonably expect to need… On the other hand, isn’t it great to finish reading a book feeling like you just did a semester at medical school? No longer will you be baffled by what is going on in your (or perhaps a loved one’s) cardiac health.
Bottom line: if you’d like to know cardiac health inside out, this book is an excellent place to start.
Click here to check out Cardiac Failure Explained, and get to the heart of things!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Is Making The Ringing In Your Ears Worse?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Rachael Cook, an audiologist at Applied Hearing Solutions in Phoenix, Arizona, shares her professional insights into managing tinnitus.
If you’re unfamiliar with Tinnitus, it is an auditory condition characterized by a ringing, buzzing, or humming sound, and ffects nearly 10% of the population. We’ve written on Tinnitus, and how it can disrupt your life, in this article.
Key Triggers for Tinnitus
Several everyday habits can make your tinnitus louder. Caffeine and nicotine increase blood pressure, restricting blood flow to the cochlea and worsening tinnitus. Common medications, such as pain relievers, high-dose antibiotics, and antidepressants, can also exacerbate tinnitus, especially with higher or long-term dosages.
Impact of Diet and Sleep
Dietary choices significantly impact tinnitus. Alcohol and salt alter the fluid balance in the cochlea, increasing tinnitus perception. Alcohol changes blood flow patterns and neurotransmitter production, while high salt intake has similar effects. Poor sleep quality elevates stress levels, making it harder to ignore tinnitus signals. Addressing sleep disorders like sleep apnea and insomnia can help manage tinnitus symptoms.
Importance of Treating Hearing Loss
Untreated hearing loss worsens tinnitus. Nearly 90% of individuals with tinnitus have some hearing loss. Hearing aids can reduce tinnitus perception by restoring missing sounds and reducing the brain’s internal compensatory signals. Combining hearing aids with sound therapy is said to provide even greater relief.
Read more about hearing loss in our article on the topic.
Otherwise, for a great guide on managing tinnitus, we recommend watching Dr. Cook’s video:
Here’s hoping your ear’s aren’t ringing too much whilst watching the video!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Five Advance Warnings of Multiple Sclerosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Five Advance Warnings of Multiple Sclerosis
First things first, a quick check-in with regard to how much you know about multiple sclerosis (MS):
- Do you know what causes it?
- Do you know how it happens?
- Do you know how it can be fixed?
If your answer to the above questions is “no”, then take solace in the fact that modern science doesn’t know either.
What we do know is that it’s an autoimmune condition, and that it results in the degradation of myelin, the “insulator” of nerves, in the central nervous system.
- How exactly this is brought about remains unclear, though there are several leading hypotheses including autoimmune attack of myelin itself, or disruption to the production of myelin.
- Treatments look to reduce/mitigate inflammation, and/or treat other symptoms (which are many and various) on an as-needed basis.
If you’re wondering about the prognosis after diagnosis, the scientific consensus on that is also “we don’t know”:
Read: Personalized medicine in multiple sclerosis: hope or reality?
this paper, like every other one we considered putting in that spot, concludes with basically begging for research to be done to identify biomarkers in a useful fashion that could help classify many distinct forms of MS, rather than the current “you have MS, but who knows what that will mean for you personally because it’s so varied” approach.
The Five Advance Warning Signs
Something we do know! First, we’ll quote directly the researchers’ conclusion:
❝We identified 5 health conditions associated with subsequent MS diagnosis, which may be considered not only prodromal but also early-stage symptoms.
However, these health conditions overlap with prodrome of two other autoimmune diseases, hence they lack specificity to MS.❞
So, these things are a warning, five alarm bells, but not necessarily diagnostic criteria.
Without further ado, the five things are:
- depression
- sexual disorders
- constipation
- cystitis
- urinary tract infections
❝This association was sufficiently robust at the statistical level for us to state that these are early clinical warning signs, probably related to damage to the nervous system, in patients who will later be diagnosed with multiple sclerosis.
The overrepresentation of these symptoms persisted and even increased over the five years after diagnosis.❞
Read the paper for yourself:
Hot off the press! Published only yesterday!
Want to know more about MS?
Here’s a very comprehensive guide:
National clinical guideline for diagnosis and management of multiple sclerosis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: