Parent Effectiveness Training – by Dr. Thomas Gordon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you want your home (or workplace, for that matter) to be a place of peace? This book literally got the author nominated for a Nobel Peace Prize. Can’t really get much higher praise than that.
The title is “Parent Effectiveness Training”, but in reality, the advice in the book is applicable to all manner of relationships, including:
- romantic relationships
- friends
- colleagues
- …and really any human interaction.
It covers some of the same topics we did today (and more) in much more detail than we ever could in a newsletter. It lays out formulae to use, gives plenty of examples, and/but is free from undue padding.
- Pros: this isn’t one of those “should have been an article” books. It has so much valuable content.
- Cons: It is from the 1970s* so examples may feel “dated” now.
In addition to going into much more detail on some of the topics covered in today’s issue of 10almonds, Dr. Gordon also talks in-depth about the concept of “problem-ownership”.
In a nutshell, that means: whose problem is a given thing? Who “has” what problem? Everyone needs to be on the same page about everyone else’s problems in the situation… as well as their own, which is not always a given!
Dr. Gordon presents, in short, tools not just to resolve conflict, but also to pre-empt it entirely. With these techniques, we can identify and deal with problems (together!) well before they arise.
Everybody wins.
Get your copy of “Parent Effectiveness Training” from Amazon today!
*Note: There is an updated edition on the market, and that’s what you’ll find upon following the above link. This reviewer (hi!) has a battered old paperback from the 1970s and cannot speak for what was changed in the new edition. However: if the 70s one is worth more than its weight in gold (and it is), the new edition is surely just as good, if not better!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Could not getting enough sleep increase your risk of type 2 diabetes?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not getting enough sleep is a common affliction in the modern age. If you don’t always get as many hours of shut-eye as you’d like, perhaps you were concerned by news of a recent study that found people who sleep less than six hours a night are at higher risk of type 2 diabetes.
So what can we make of these findings? It turns out the relationship between sleep and diabetes is complex.
The study
Researchers analysed data from the UK Biobank, a large biomedical database which serves as a global resource for health and medical research. They looked at information from 247,867 adults, following their health outcomes for more than a decade.
The researchers wanted to understand the associations between sleep duration and type 2 diabetes, and whether a healthy diet reduced the effects of short sleep on diabetes risk.
As part of their involvement in the UK Biobank, participants had been asked roughly how much sleep they get in 24 hours. Seven to eight hours was the average and considered normal sleep. Short sleep duration was broken up into three categories: mild (six hours), moderate (five hours) and extreme (three to four hours). The researchers analysed sleep data alongside information about people’s diets.
Some 3.2% of participants were diagnosed with type 2 diabetes during the follow-up period. Although healthy eating habits were associated with a lower overall risk of diabetes, when people ate healthily but slept less than six hours a day, their risk of type 2 diabetes increased compared to people in the normal sleep category.
The researchers found sleep duration of five hours was linked with a 16% higher risk of developing type 2 diabetes, while the risk for people who slept three to four hours was 41% higher, compared to people who slept seven to eight hours.
One limitation is the study defined a healthy diet based on the number of servings of fruit, vegetables, red meat and fish a person consumed over a day or a week. In doing so, it didn’t consider how dietary patterns such as time-restricted eating or the Mediterranean diet may modify the risk of diabetes among those who slept less.
Also, information on participants’ sleep quantity and diet was only captured at recruitment and may have changed over the course of the study. The authors acknowledge these limitations.
Why might short sleep increase diabetes risk?
In people with type 2 diabetes, the body becomes resistant to the effects of a hormone called insulin, and slowly loses the capacity to produce enough of it in the pancreas. Insulin is important because it regulates glucose (sugar) in our blood that comes from the food we eat by helping move it to cells throughout the body.
We don’t know the precise reasons why people who sleep less may be at higher risk of type 2 diabetes. But previous research has shown sleep-deprived people often have increased inflammatory markers and free fatty acids in their blood, which impair insulin sensitivity, leading to insulin resistance. This means the body struggles to use insulin properly to regulate blood glucose levels, and therefore increases the risk of type 2 diabetes.
Further, people who don’t sleep enough, as well as people who sleep in irregular patterns (such as shift workers), experience disruptions to their body’s natural rhythm, known as the circadian rhythm.
This can interfere with the release of hormones like cortisol, glucagon and growth hormones. These hormones are released through the day to meet the body’s changing energy needs, and normally keep blood glucose levels nicely balanced. If they’re compromised, this may reduce the body’s ability to handle glucose as the day progresses.
These factors, and others, may contribute to the increased risk of type 2 diabetes seen among people sleeping less than six hours.
Millions of people around the world have diabetes. WESTOCK PRODUCTIONS/Shutterstock While this study primarily focused on people who sleep eight hours or less, it’s possible longer sleepers may also face an increased risk of type 2 diabetes.
Research has previously shown a U-shaped correlation between sleep duration and type 2 diabetes risk. A review of multiple studies found getting between seven to eight hours of sleep daily was associated with the lowest risk. When people got less than seven hours sleep, or more than eight hours, the risk began to increase.
The reason sleeping longer is associated with increased risk of type 2 diabetes may be linked to weight gain, which is also correlated with longer sleep. Likewise, people who don’t sleep enough are more likely to be overweight or obese.
Good sleep, healthy diet
Getting enough sleep is an important part of a healthy lifestyle and may reduce the risk of type 2 diabetes.
Based on this study and other evidence, it seems that when it comes to diabetes risk, seven to eight hours of sleep may be the sweet spot. However, other factors could influence the relationship between sleep duration and diabetes risk, such as individual differences in sleep quality and lifestyle.
While this study’s findings question whether a healthy diet can mitigate the effects of a lack of sleep on diabetes risk, a wide range of evidence points to the benefits of healthy eating for overall health.
The authors of the study acknowledge it’s not always possible to get enough sleep, and suggest doing high-intensity interval exercise during the day may offset some of the potential effects of short sleep on diabetes risk.
In fact, exercise at any intensity can improve blood glucose levels.
Giuliana Murfet, Casual Academic, Faculty of Health, University of Technology Sydney and ShanShan Lin, Senior Lecturer, School of Public Health, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
STI rates are increasing among midlife and older adults. We need to talk about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, the rates of common sexually transmissible infections (STIs) are increasing among people aged over 50. In some cases, rates are rising faster than among younger people.
Recent data from the United States Centers for Disease Control and Prevention shows that, among people aged 55 and older, rates of gonorrhoea and chlamydia, two of the most common STIs, more than doubled between 2012 and 2022.
Australian STI surveillance data has reflected similar trends. Between 2013 and 2022, there was a steady increase in diagnoses of chlamydia, gonorrhoea and syphilis among people aged 40 and older. For example, there were 5,883 notifications of chlamydia in Australians 40 plus in 2013, compared with 10,263 in 2022.
A 2020 study of Australian women also showed that, between 2000 and 2018, there was a sharper increase in STI diagnoses among women aged 55–74 than among younger women.
While the overall rate of common STIs is highest among young adults, the significant increase in STI diagnoses among midlife and older adults suggests we need to pay more attention to sexual health across the life course.
Fit Ztudio/Shutterstock Why are STI rates rising among older adults?
STI rates are increasing globally for all age groups, and an increase among midlife and older people is in line with this trend.
However, increases of STIs among older people are likely due to a combination of changing sex and relationship practices and hidden sexual health needs among this group.
The “boomer” generation came of age in the 60s and 70s. They are the generation of free love and their attitude to sex, even as they age, is quite different to that of generations before them.
Given the median age of divorce in Australia is now over 43, and the internet has ushered in new opportunities for post-separation dating, it’s not surprising that midlife and older adults are exploring new sexual practices or finding multiple sexual partners.
People may start new relationships later in life. Tint Media/Shutterstock It’s also possible midlife and older people have not had exposure to sexual health education in school or do not relate to current safe sex messages, which tend to be directed toward young people. Condoms may therefore seem unnecessary for people who aren’t trying to avoid pregnancy. Older people may also lack confidence negotiating safe sex or accessing STI screening.
Hidden sexual health needs
In contemporary life, the sex lives of older adults are largely invisible. Ageing and older bodies are often associated with loss of power and desirability, reflected in the stereotype of older people as asexual and in derogatory jokes about older people having sex.
With some exceptions, we see few positive representations of older sexual bodies in film or television.
Older people’s sexuality is also largely invisible in public policy. In a review of Australian policy relating to sexual and reproductive health, researchers found midlife and older adults were rarely mentioned.
Sexual health policy generally targets groups with the highest STI rates, which excludes most older people. As midlife and older adults are beyond childbearing years, they also do not feature in reproductive health policy. This means there is a general absence of any policy related to sex or sexual health among midlife or older adults.
Added to this, sexual health policy tends to be focused on risk rather than sexual wellbeing. Sexual wellbeing, including freedom and capacity to pursue pleasurable sexual experiences, is strongly associated with overall health and quality of life for adults of all ages. Including sexual wellbeing as a policy priority would enable a focus on safe and respectful sex and relationships across the adult life course.
Without this priority, we have limited knowledge about what supports sexual wellbeing as people age and limited funding for initiatives to engage with midlife or older adults on these issues.
Midlife and older adults may have limited knowledge about STIs. Southworks/Shutterstock How can we support sexual health and wellbeing for older adults?
Most STIs are easily treatable. Serious complications can occur, however, when STIs are undiagnosed and untreated over a long period. Untreated STIs can also be passed on to others.
Late diagnosis is not uncommon as some STIs can have no symptoms and many people don’t routinely screen for STIs. Older, heterosexual adults are, in general, less likely than other groups to seek regular STI screening.
For midlife or older adults, STIs may also be diagnosed late because some doctors do not initiate testing due to concerns they will cause offence or because they assume STI risk among older people is negligible.
Many doctors are reluctant to discuss sexual health with their older patients unless the patient explicitly raises the topic. However, older people can be embarrassed or feel awkward raising matters of sex.
Resources for health-care providers and patients to facilitate conversations about sexual health and STI screening with older patients would be a good first step.
To address rising rates of STIs among midlife and older adults, we also need to ensure sexual health promotion is targeted toward these age groups and improve accessibility of clinical services.
More broadly, it’s important to consider ways to ensure sexual wellbeing is prioritised in policy and practice related to midlife and older adulthood.
A comprehensive approach to older people’s sexual health, that explicitly places value on the significance of sex and intimacy in people’s lives, will enhance our ability to more effectively respond to sexual health and STI prevention across the life course.
Jennifer Power, Associate Professor and Principal Research Fellow, Australian Research Centre in Sex, Health and Society, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
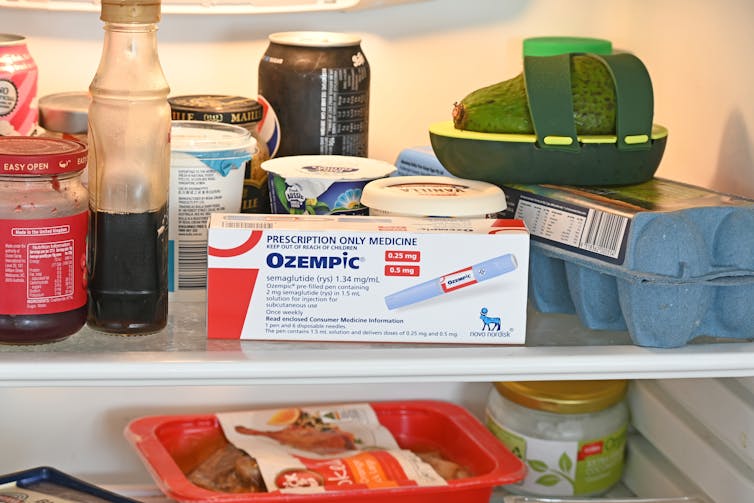
People on Ozempic may have fewer heart attacks, strokes and addictions – but more nausea, vomiting and stomach pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ozempic and Wegovy are increasingly available in Australia and worldwide to treat type 2 diabetes and obesity.
The dramatic effects of these drugs, known as GLP-1s, on weight loss have sparked huge public interest in this new treatment option.
However, the risks and benefits are still being actively studied.
In a new study in Nature Medicine, researchers from the United States reviewed health data from about 2.4 million people who have type 2 diabetes, including around 216,000 people who used a GLP-1 drug, between 2017 and 2023.
The researchers compared a range of health outcomes when GLP-1s were added to a person’s treatment plan, versus managing their diabetes in other ways, often using glucose-lowering medications.
Overall, they found people who used GLP-1s were less likely to experience 42 health conditions or adverse health events – but more likely to face 19 others.
myskin/Shutterstock What conditions were less common?
Cardiometabolic conditions
GLP-1 use was associated with fewer serious cardiovascular and coagulation disorders. This includes deep vein thrombosis, pulmonary embolism, stroke, cardiac arrest, heart failure and myocardial infarction.
Neurological and psychiatric conditions
GLP-1 use was associated with fewer reported substance use disorders or addictions, psychotic disorders and seizures.
Infectious conditions
GLP-1 use was associated with fewer bacterial infections and pneumonia.
What conditions were more common?
Gastrointestinal conditions
Consistent with prior studies, GLP-1 use was associated with gastrointestinal conditions such as nausea, vomiting, gastritis, diverticulitis and abdominal pain.
Other adverse effects
Increased risks were seen for conditions such as low blood pressure, syncope (fainting) and arthritis.
People who took Ozempic were more likely to experience stomach upsets than those who used other type 2 diabetes treatments. Douglas Cliff/Shutterstock How robust is this study?
The study used a large and reputable dataset from the US Department of Veterans Affairs. It’s an observational study, meaning the researchers tracked health outcomes over time without changing anyone’s treatment plan.
A strength of the study is it captures data from more than 2.4 million people across more than six years. This is much longer than what is typically feasible in an intervention study.
Observational studies like this are also thought to be more reflective of the “real world”, because participants aren’t asked to follow instructions to change their behaviour in unnatural or forced ways, as they are in intervention studies.
However, this study cannot say for sure that GLP-1 use was the cause of the change in risk of different health outcomes. Such conclusions can only be confidently made from tightly controlled intervention studies, where researchers actively change or control the treatment or behaviour.
The authors note the data used in this study comes from predominantly older, white men so the findings may not apply to other groups.
Also, the large number of participants means that even very small effects can be detected, but they might not actually make a real difference in overall population health.
Observational studies track outcomes over time, but can’t say what caused the changes. Jacob Lund/Shutterstock Other possible reasons for these links
Beyond the effect of GLP-1 in the body, other factors may explain some of the findings in this study. For example, it’s possible that:
- people who used GLP-1 could be more informed about treatment options and more motivated to manage their own health
- people who used GLP-1 may have received it because their health-care team were motivated to offer the latest treatment options, which could lead to better care in other areas that impact the risk of various health outcomes
- people who used GLP-1 may have been able to do so because they lived in metropolitan centres and could afford the medication, as well as other health-promoting services and products, such as gyms, mental health care, or healthy food delivery services.
Did the authors have any conflicts of interest?
Two of the study’s authors declared they were “uncompensated consultants” for Pfizer, a global pharmaceutical company known for developing a wide range of medicines and vaccines. While Pfizer does not currently make readily available GLP-1s such as Ozempic or Wegovy, they are attempting to develop their own GLP-1s, so may benefit from greater demand for these drugs.
This research was funded by the US Department of Veterans Affairs, a government agency that provides a wide range of services to military veterans.
No other competing interests were reported.
Diabetes vs weight-loss treatments
Overall, this study shows people with type 2 diabetes using GLP-1 medication generally have more positive health outcomes than negative health outcomes.
However, the study didn’t include people without type 2 diabetes. More research is needed to understand the effects of these medications in people without diabetes who are using them for other reasons, including weight loss.
While the findings highlight the therapeutic benefits of GLP-1 medications, they also raise important questions about how to manage the potential risks for those who choose to use this medication.
The findings of this study can help many people, including:
- policymakers looking at ways to make GLP-1 medications more widely available for people with various health conditions
- health professionals who have regular discussions with patients considering GLP-1 use
- individuals considering whether a GLP-1 medication is right for them.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
The Glucose Goddess Method – by Jessie Inchausspé
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Inchausspé’s excellent book “Glucose Revolution”. So what does this book add?
This book is for those who found that book a little dense. While this one still gives the same ten “hacks”, she focuses on the four that have the biggest effect, and walks the reader by the hand through a four-week programme of implementing them.
The claim of 100+ recipes is a little bold, as some of the recipes are things like vinegar, vinegar+water, vinegar+water but now we’re it’s in a restaurant, lemon+water, lemon+water but now it’s in a bottle, etc. However, there are legitimately a lot of actual recipes too.
Where this book’s greatest strength lies is in making everything super easy, and motivating. It’s a fine choice for being up-and-running quickly and easily without wading through the 300-odd pages of science in her previous book.
Bottom line: if you’ve already happily and sustainably implemented everything from her previous book, you can probably skip this one. However, if you’d like an easier method to implement the changes that have the biggest effect, then this is the book for you.
Click here to check out The Glucose Goddess Method, and build it into your life the easy way!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ice Cream vs Fruit Sorbet – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing ice cream to fruit sorbet, we picked the ice cream.
Why?
Well, neither are great!
But the deciding factor is simple: ice cream has more nutrients to go with its sugar.
While “fruit is good” is a very reliable truism in and of itself, sorbet tends to be made with fruit juice (or at best, purée, which for these purposes is more or less the same) and sugar. The small vitamin content is nowhere near enough to make up for this. The fiber having been removed by juicing or puréeing, the fruit juice with added sugar is basically shooting glucose and fructose into your veins while doing little else.
Fruit juice (even freshly-pressed) is nowhere near in the same league of healthiness as actual fruit!
See also: Which Sugars Are Healthier, And Which Are Just The Same?
Ice cream, meanwhile, is also not exactly a health food. But it has at least some minerals worth speaking of (mostly: calcium, potassium, phosphorus), and some fat that a) can be used b) helps slightly slow the absorption of the sugars.
In short: please do not consider either of these things to be a health food. But if you’re going to choose one or the other (and are not lactose-intolerant), then ice cream has some small positives to go with its negatives.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Paving The Way To Good Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Michelle Tollefson. She’s a gynecologist, and a menopause and lifestyle medicine expert. She’s also a breast cancer survivor, and, indeed, thriver.
So, what does she want us to know?
A Multivector Approach To Health
There’s a joke that goes: a man is trapped in a flooding area, and as the floodwaters rise, he gets worried and begins to pray, but he is interrupted when some people come by on a raft and offer him to go with them. He looks at the rickety raft and says “No, you go on, God will spare me”. He returns to his prayer, and is further interrupted by a boat and finally a helicopter, and each time he gives the same response. He drowns, and in the afterlife he asks God “why didn’t you spare me from the flood?”, and God replies “I sent a raft, a boat, and a helicopter; what more did you want?!”
People can be a bit the same when it comes to different approaches to cancer and other serious illness. They are offered chemotherapy and say “No, thank you, eating fruit will spare me”.
Now, this is not to trivialize those who decline aggressive cancer treatments for other reasons such as “I am old and would rather not go through that; I’d rather have a shorter life without chemo than a longer life with it”—for many people that’s a valid choice.
But it is to say: lifestyle medicine is, mostly, complementary medicine.
It can be very powerful! It can make the difference between life and death! Especially when it comes to things like cancer, diabetes, heart disease, etc.
But it’s not a reason to decline powerful medical treatments if/when those are appropriate. For example, in Dr. Tollefson’s case…
Synergistic health
Dr. Tollefson, herself a lifestyle medicine practitioner and gynecologist (and having thus done thousands of clinical breast exams for other people, screening for breast cancer), says she owes her breast cancer survival to two things, or rather two categories of things:
- a whole-food, plant predominant diet, daily physical activity, prioritizing sleep, minimizing stress, and a strong social network
- a bilateral mastectomy, 16 rounds of chemotherapy, removal of her ovaries, and several reconstructive surgeries
Now, one may wonder: if the first thing is so good, why need the second?
Or on the flipside: if the second thing was necessary, what was the point of the first?
And the answer she gives is: the first thing was the reason she was able to make it through the second thing.
And on the next level: the second thing was the reason she’s still around to talk about the first thing.
In other words: she couldn’t have done it with just one or the other.
A lot of medicine in general, and lifestyle medicine in particular, is like this. If we note that such-and-such a thing decreases our risk of cancer mortality by 4%, that’s a small decrease, but it can add up (and compound!) if it’s surrounded by other things that also each decrease the risk by 12%, 8%, 15%, and so on.
Nor is this only confined to cancer, nor only to the positives.
Let’s take cardiovascular disease: if a person smokes, drinks, eats red meat, stresses, and has a wild sleep schedule, you can imagine those risk factors add up and compound.
If this person and another with a heart-healthy lifestyle both have a stroke (it can happen to anyone, even if it’s less likely in this case), and both need treatment, then two things are true:
- They are both still going to need treatment (medicines, and possibly a thrombectomy)
- The second person is most likely to recover, and most likely to recover more quickly and easily
The second person can be said to have paved the way to their recovery, with their lifestyle.
Which is really important, because a lot of people think “what’s the point in living so healthily if [disease] strikes anyway?” and the answer is:
A very large portion of your recovery is predicated on how you lived your life before The Bad Thing™ happened, and that can be the difference between bouncing back quickly and a long struggle back to health.
Or the difference between a long struggle back to health, or a short struggle followed by rapid decline and death.
In short:
Play the odds, improve your chances with lifestyle medicine. Enjoy those cancer-fighting fruits:
Top 8 Fruits That Prevent & Kill Cancer
…but also, get your various bits checked when appropriate; we know, mammograms and prostate checks etc are not usually the highlight of most people’s days, but they save lives. And if it turns out you need serious medical interventions, consider them seriously.
And, by all means, enjoy mood-boosting nutraceuticals such as:
12 Foods That Fight Depression & Anxiety
…but also recognize that sometimes, your brain might have an ongoing biochemical problem that a tablespoon of pumpkin seeds isn’t going to fix.
And absolutely, you can make lifestyle adjustments to reduce the risks associated with menopause, for example:
Menopause, & How Lifestyle Continues To Matter “Postmenopause”
…but also be aware that if the problem is “not enough estrogen”, sometimes to solution is “take estrogen”.
And so on.
Want to know Dr. Tollefson’s lifestyle recommendations?
Most of them will not be a surprise to you, and we mentioned some of them above (a whole-food, plant predominant diet, daily physical activity, prioritizing sleep, minimizing stress, and a strong social network), but for more specific recommendations, including numbers etc, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: