A short history of sunscreen, from basting like a chook to preventing skin cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australians have used commercial creams, lotions or gels to manage our skin’s sun exposure for nearly a century.
But why we do it, the preparations themselves, and whether they work, has changed over time.
In this short history of sunscreen in Australia, we look at how we’ve slathered, slopped and spritzed our skin for sometimes surprising reasons.
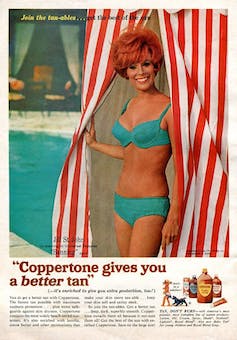
At first, suncreams helped you ‘tan with ease’
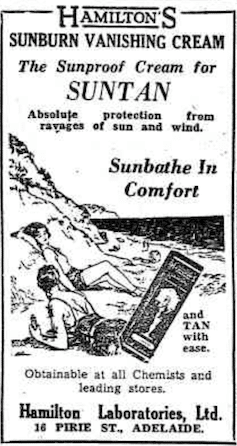
Trove/NLA
Sunscreens have been available in Australia since the 30s. Chemist Milton Blake made one of the first.
He used a kerosene heater to cook batches of “sunburn vanishing cream”, scented with French perfume.
His backyard business became H.A. Milton (Hamilton) Laboratories, which still makes sunscreens today.
Hamilton’s first cream claimed you could “
Sunbathe in Comfort and TAN with ease”. According to modern standards, it would have had an SPF (or sun protection factor) of 2.
The mirage of ‘safe tanning’
A tan was considered a “modern complexion” and for most of the 20th century, you might put something on your skin to help gain one. That’s when “safe tanning” (without burning) was thought possible.
SenseiAlan/Flickr, CC BY-SA
Sunburn was known to be caused by the UVB component of ultraviolet (UV) light. UVA, however, was thought not to be involved in burning; it was just thought to darken the skin pigment melanin. So, medical authorities advised that by using a sunscreen that filtered out UVB, you could “safely tan” without burning.
But that was wrong.
From the 70s, medical research suggested UVA penetrated damagingly deep into the skin, causing ageing effects such as sunspots and wrinkles. And both UVA and UVB could cause skin cancer.
Sunscreens from the 80s sought to be “broad spectrum” – they filtered both UVB and UVA.
Researchers consequently recommended sunscreens for all skin tones, including for preventing sun damage in people with dark skin.
Delaying burning … or encouraging it?
Up to the 80s, sun preparations ranged from something that claimed to delay burning, to preparations that actively encouraged it to get that desirable tan – think, baby oil or coconut oil. Sun-worshippers even raided the kitchen cabinet, slicking olive oil on their skin.
One manufacturer’s “sun lotion” might effectively filter UVB; another’s merely basted you like a roast chicken.
Since labelling laws before the 80s didn’t require manufacturers to list the ingredients, it was often hard for consumers to tell which was which.
At last, SPF arrives to guide consumers
In the 70s, two Queensland researchers, Gordon Groves and Don Robertson, developed tests for sunscreens – sometimes experimenting on students or colleagues. They printed their ranking in the newspaper, which the public could use to choose a product.
An Australian sunscreen manufacturer then asked the federal health department to regulate the industry. The company wanted standard definitions to market their products, backed up by consistent lab testing methods.
In 1986, after years of consultation with manufacturers, researchers and consumers, Australian Standard AS2604 gave a specified a testing method, based on the Queensland researchers’ work. We also had a way of expressing how well sunscreens worked – the sun protection factor or SPF.
This is the ratio of how long it takes a fair-skinned person to burn using the product compared with how long it takes to burn without it. So a cream that protects the skin sufficiently so it takes 40 minutes to burn instead of 20 minutes has an SPF of 2.
Manufacturers liked SPF because businesses that invested in clever chemistry could distinguish themselves in marketing. Consumers liked SPF because it was easy to understand – the higher the number, the better the protection.
Australians, encouraged from 1981 by the Slip! Slop! Slap! nationwide skin cancer campaign, could now “slop” on a sunscreen knowing the degree of protection it offered.
How about skin cancer?
It wasn’t until 1999 that research proved that using sunscreen prevents skin cancer. Again, we have Queensland to thank, specifically the residents of Nambour. They took part in a trial for nearly five years, carried out by a research team led by Adele Green of the Queensland Institute of Medical Research. Using sunscreen daily over that time reduced rates of squamous cell carcinoma (a common form of skin cancer) by about 60%.
Follow-up studies in 2011 and 2013 showed regular sunscreen use almost halved the rate of melanoma and slowed skin ageing. But there was no impact on rates of basal cell carcinoma, another common skin cancer.
By then, researchers had shown sunscreen stopped sunburn, and stopping sunburn would prevent at least some types of skin cancer.
What’s in sunscreen today?
An effective sunscreen uses one or more active ingredients in a cream, lotion or gel. The active ingredient either works:
-
“chemically” by absorbing UV and converting it to heat. Examples include PABA (para-aminobenzoic acid) and benzyl salicylate, or
-
“physically” by blocking the UV, such as zinc oxide or titanium dioxide.
Physical blockers at first had limited cosmetic appeal because they were opaque pastes. (Think cricketers with zinc smeared on their noses.)
With microfine particle technology from the 90s, sunscreen manufacturers could then use a combination of chemical absorbers and physical blockers to achieve high degrees of sun protection in a cosmetically acceptable formulation.
Where now?
Australians have embraced sunscreen, but they still don’t apply enough or reapply often enough.
Although some people are concerned sunscreen will block the skin’s ability to make vitamin D this is unlikely. That’s because even SPF50 sunscreen doesn’t filter out all UVB.
There’s also concern about the active ingredients in sunscreen getting into the environment and whether their absorption by our bodies is a problem.
Sunscreens have evolved from something that at best offered mild protection to effective, easy-to-use products that stave off the harmful effects of UV. They’ve evolved from something only people with fair skin used to a product for anyone.
Remember, slopping on sunscreen is just one part of sun protection. Don’t forget to also slip (protective clothing), slap (hat), seek (shade) and slide (sunglasses).
Laura Dawes, Research Fellow in Medico-Legal History, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How often should you really weigh yourself?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Few topics are more debated in health than the value of the humble bathroom scale. Some experts advocate daily self-weigh-ins to promote accountability for weight management, particularly when we’re following a diet and exercise program to lose weight.
Others suggest ditching self-weigh-ins altogether, arguing they can trigger negative psychological responses and unhealthy behaviours when we don’t like, or understand, the number we see on the scale.
Many, like me, recommend using scales to weigh yourself weekly, even when we’re not trying to lose weight. Here’s why.
Diva Plavalaguna/Pexels 1. Weighing weekly helps you manage your weight
Research confirms regular self-weighing is an effective weight loss and management strategy, primarily because it helps increase awareness of our current weight and any changes.
A systematic review of 12 studies found participants who weighed themselves weekly or daily over several months lost 1–3 BMI (body mass index) units more and regained less weight than participants who didn’t weight themselves frequently. The weight-loss benefit was evident with weekly weighing; there was no added benefit with daily weighing.
Weighing regularly means we know when our weight changes. Andres Ayrton/Pexels Self-weigh-ins are an essential tool for weight management as we age. Adults tend to gain weight progressively through middle age. While the average weight gain is typically between 0.5–1kg per year, this modest accumulation of weight can lead to obesity over time. Weekly weighing and keeping track of the results helps avoid unnecessary weight gain.
Tracking our weight can also help identify medical issues early. Dramatic changes in weight can be an early sign of some conditions, including problems with our thyroid, digestion and diabetes.
2. Weekly weighing accounts for normal fluctuations
Our body weight can fluctuate within a single day and across the days of the week. Studies show body weight fluctuates by 0.35% within the week and it’s typically higher after the weekend.
Daily and day-to-day body weight fluctuations have several causes, many linked to our body’s water content. The more common causes include:
The type of food we’ve consumed
When we’ve eaten a dinner higher in carbohydrates, we’ll weigh more the next day. This change is a result of our bodies temporarily carrying more water. We retain 3–4 grams of water per gram of carbohydrate consumed to store the energy we take from carbs.
Our water content also increases when we consume foods higher in salt. Our bodies try to maintain a balance of sodium and water. When the concentration of salt in our bloodstream increases, a mechanism is triggered to restore balance by retaining water to dilute the excess salt.
The morning after a big pasta dinner, we’ll carry more water weight. Dana Tentis/Pexels Our food intake
Whether it’s 30 grams of nuts or 65 grams of lean meat, everything we eat and drink has weight, which increases our body weight temporarily while we digest and metabolise what we’ve consumed.
Our weight also tends to be lower first thing in the morning after our food intake has been restricted overnight and higher in the evening after our daily intake of food and drinks.
Exercise
If we weigh ourselves at the gym after a workout, there’s a good chance we’ll weigh less due to sweat-induced fluid loss. The amount of water lost varies depending on things like our workout intensity and duration, the temperature and humidity, along with our sweat rate and hydration level. On average, we lose 1 litre of sweat during an hour of moderate-intensity exercise.
Hormonal changes
Fluctuations in hormones within your menstrual cycle can also affect fluid balance. Women may experience fluid retention and temporarily gain 0.5–2kg of weight at this time. Specifically, the luteal phase, which represents the second half of a woman’s cycle, results in a shift of fluid from your blood plasma to your cells, and bloating.
Most of our weight fluctuations are water-related. Engin Akyurt/Unsplash Bowel movements
Going to the bathroom can lead to small but immediate weight loss as waste is eliminated from the body. While the amount lost will vary, we generally eliminate around 100 grams of weight through our daily bowel movements.
All of these fluctuations are normal, and they’re not indicative of significant changes in our body fat or muscle mass. However, seeing these fluctuations can lead to unnecessary stress and a fixation with our weight.
3. Weekly weighing avoids scale obsession and weight-loss sabotage
Weighing too frequently can create an obsession with the number on the scales and do more harm than good.
Often, our reaction when we see this number not moving in the direction we want or expect is to further restrict our food intake or embark on fad dieting. Along with not being enjoyable or sustainable, fad diets also ultimately increase our weight gain rather than reversing it.
This was confirmed in a long-term study comparing intentional weight loss among more than 4,000 twins. The researchers found the likelihood of becoming overweight by the age of 25 was significantly greater for a twin who dieted to lose 5kg or more. This suggests frequent dieting makes us more susceptible to weight gain and prone to future weight gain.
So what should you do?
Weighing ourselves weekly gives a more accurate measure of our weight trends over time.
Aim to weigh yourself on the same day, at the same time and in the same environment each week – for example, first thing every Friday morning when you’re getting ready to take a shower, after you’ve gone to the bathroom, but before you’ve drunk or eaten anything.
Weigh yourself at the same time on the same day of the week. Alexanderstock23/Shutterstock Use the best quality scales you can afford. Change the batteries regularly and check their accuracy by using a “known” weight – for example, a 10kg weight plate. Place the “known” weight on the scale and check the measurement aligns with the “known” weight.
Remember, the number on the scale is just one part of health and weight management. Focusing solely on it can overshadow other indicators, such as how your clothes fit. It’s also essential to pay equal attention to how we’re feeling, physically and emotionally.
Stop weighing yourself – at any time interval – if it’s triggering anxiety or stress, and get in touch with a health-care professional to discuss this.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Charles Perkins Centre Research Program Leader, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Our ‘food environments’ affect what we eat. Here’s how you can change yours to support healthier eating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In January, many people are setting new year’s resolutions around healthy eating. Achieving these is often challenging – it can be difficult to change our eating habits. But healthy diets can enhance physical and mental health, so improving what we eat is a worthwhile goal.
One reason it’s difficult to change our eating habits relates to our “food environments”. This term describes:
The collective physical, economic, policy and sociocultural surroundings, opportunities and conditions that influence people’s food and beverage choices and nutritional status.
Our current food environments are designed in ways that often make it easier to choose unhealthy foods than healthy ones. But it’s possible to change certain aspects of our personal food environments, making eating healthier a little easier.
Unhealthy food environments
It’s not difficult to find fast-food restaurants in Australian cities. Meanwhile, there are junk foods at supermarket checkouts, service stations and sporting venues. Takeaway and packaged foods and drinks routinely come in large portion sizes and are often considered tastier than healthy options.
Our food environments also provide us with various prompts to eat unhealthy foods via the media and advertising, alongside health and nutrition claims and appealing marketing images on food packaging.
At the supermarket, unhealthy foods are often promoted through prominent displays and price discounts.
We’re also exposed to various situations in our everyday lives that can make healthy eating challenging. For example, social occasions or work functions might see large amounts of unhealthy food on offer.
Not everyone is affected in the same way
People differ in the degree to which their food consumption is influenced by their food environments.
This can be due to biological factors (for example, genetics and hormones), psychological characteristics (such as decision making processes or personality traits) and prior experiences with food (for example, learned associations between foods and particular situations or emotions).
People who are more susceptible will likely eat more and eat more unhealthy foods than those who are more immune to the effects of food environments and situations.
Those who are more susceptible may pay greater attention to food cues such as advertisements and cooking smells, and feel a stronger desire to eat when exposed to these cues. Meanwhile, they may pay less attention to internal cues signalling hunger and fullness. These differences are due to a combination of biological and psychological characteristics.
These people might also be more likely to experience physiological reactions to food cues including changes in heart rate and increased salivation.
It’s common to eat junk food in front of the TV.
PR Image Factory/ShutterstockOther situational cues can also prompt eating for some people, depending on what they’ve learned about eating. Some of us tend to eat when we’re tired or in a bad mood, having learned over time eating provides comfort in these situations.
Other people will tend to eat in situations such as in the car during the commute home from work (possibly passing multiple fast-food outlets along the way), or at certain times of day such as after dinner, or when others around them are eating, having learned associations between these situations and eating.
Being in front of a TV or other screen can also prompt people to eat, eat unhealthy foods, or eat more than intended.
Making changes
While it’s not possible to change wider food environments or individual characteristics that affect susceptibility to food cues, you can try to tune into how and when you’re affected by food cues. Then you can restructure some aspects of your personal food environments, which can help if you’re working towards healthier eating goals.
Although both meals and snacks are important for overall diet quality, snacks are often unplanned, which means food environments and situations may have a greater impact on what we snack on.
Foods consumed as snacks are often sugary drinks, confectionery, chips and cakes. However, snacks can also be healthy (for example, fruits, nuts and seeds).
Try removing unhealthy foods, particularly packaged snacks, from the house, or not buying them in the first place. This means temptations are removed, which can be especially helpful for those who may be more susceptible to their food environment.
Planning social events around non-food activities can help reduce social influences on eating. For example, why not catch up with friends for a walk instead of lunch at a fast-food restaurant.
Creating certain rules and habits can reduce cues for eating. For example, not eating at your desk, in the car, or in front of the TV will, over time, lessen the effects of these situations as cues for eating.
You could also try keeping a food diary to identify what moods and emotions trigger eating. Once you’ve identified these triggers, develop a plan to help break these habits. Strategies may include doing another activity you enjoy such as going for a short walk or listening to music – anything that can help manage the mood or emotion where you would have typically reached for the fridge.
Write (and stick to) a grocery list and avoid shopping for food when hungry. Plan and prepare meals and snacks ahead of time so eating decisions are made in advance of situations where you might feel especially hungry or tired or be influenced by your food environment.
Georgie Russell, Senior Lecturer, Institute for Physical Activity and Nutrition (IPAN), Deakin University and Rebecca Leech, NHMRC Emerging Leadership Fellow, School of Exercise and Nutrition Sciences, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
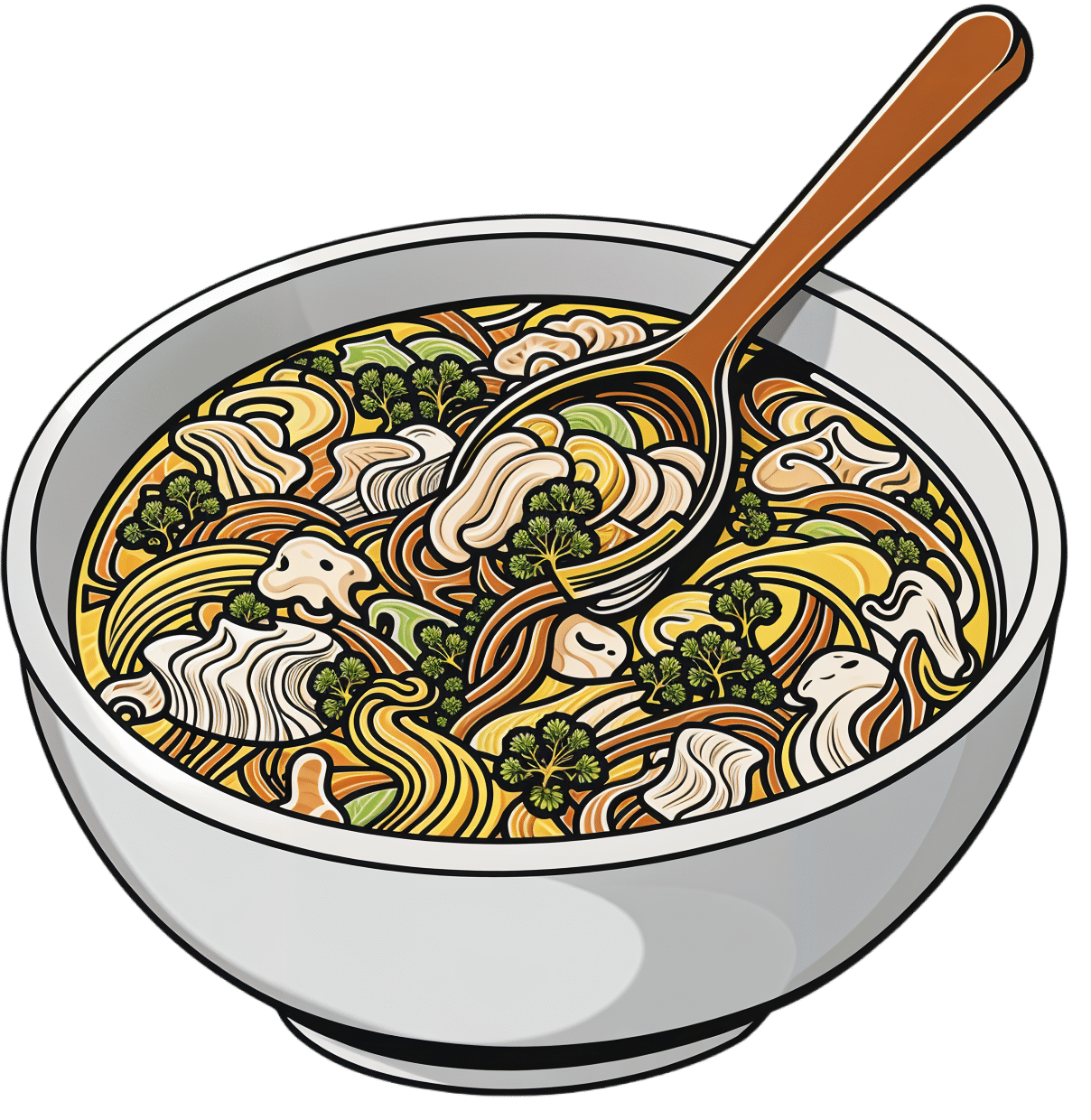
Hot And Sour Shiitake Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a popular, easy, and delicious soup that nonetheless is not found in many western kitchens, despite being enjoyed in restaurants/take-out. Best of all, making it at home means that you know all the ingredients, can account for quality, and also can customize it per your preferences (i.e. how much heat/sourness you like).
You will need
- 3 cups shiitake mushrooms, sliced
- 3 cups bok choy, chopped
- 2 cups cherry tomatoes, quartered
- 1 cup carrot, grated
- 3 spring onions, chopped
- 2 shallots, sliced lengthways
- 2 serrano chilis (or similar), sliced thinly
- 2 tbsp apple cider vinegar
- 1 tbsp lemon juice
- 1 tbsp fresh ginger, sliced into 1″ strips
- 1 tsp black pepper, coarse ground
- ½ bulb garlic, crushed
- 6 cups low-sodium vegetable stock. Ideally you will have made it yourself from vegetable cuttings that you saved in the freezer until you had enough to make stock from, but if that’s not an option, then low-sodium vegetable stock cubes can be purchased and used.
- Garnish: ¼ cup (or 4 tbsp) cilantro, chopped, or if you have the soap gene, then this time we recommend chopped basil as the subsitution
Method
(we suggest you read everything at least once before doing anything)
1) Put the ginger in a big pot with the stock; cover and simmer for about 20 minutes (otherwise the ginger flavor will remain mostly concentrated in the ginger strips).
2) Bring it to a boil and add the bok choy, mushrooms, shallots, chili peppers, and the carrot; simmer for another 5 minutes
3) Add the remaining ingredients except for the garnish, and simmer for another 5 minutes
4) Serve, adding the garnish
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The (Longevity) Magic of Mushrooms
- Our Top 5 Spices: How Much Is Enough For Benefits?
- An Apple (Cider Vinegar) A Day…
- Enjoy Bitter/Hot/Sour/Pungent Foods For Your Heart & Brain
- Brain Food? The Eyes Have It!
- Some Surprising Truths About Hunger And Satiety
Take care!
Share This Post
Related Posts
-
Ouch. That ‘Free’ Annual Checkup Might Cost You. Here’s Why.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Kristy Uddin, 49, went in for her annual mammogram in Washington state last year, she assumed she would not incur a bill because the test is one of the many preventive measures guaranteed to be free to patients under the 2010 Affordable Care Act. The ACA’s provision made medical and economic sense, encouraging Americans to use screening tools that could nip medical problems in the bud and keep patients healthy.
So when a bill for $236 arrived, Uddin — an occupational therapist familiar with the health care industry’s workings — complained to her insurer and the hospital. She even requested an independent review.
“I’m like, ‘Tell me why am I getting this bill?’” Uddin recalled in an interview. The unsatisfying explanation: The mammogram itself was covered, per the ACA’s rules, but the fee for the equipment and the facility was not.
That answer was particularly galling, she said, because, a year earlier, her “free” mammogram at the same health system had generated a bill of about $1,000 for the radiologist’s reading. Though she fought that charge (and won), this time she threw in the towel and wrote the $236 check. But then she dashed off a submission to the KFF Health News-NPR “Bill of the Month” project:
“I was really mad — it’s ridiculous,” she later recalled. “This is not how the law is supposed to work.”
The ACA’s designers might have assumed that they had spelled out with sufficient clarity that millions of Americans would no longer have to pay for certain types of preventive care, including mammograms, colonoscopies, and recommended vaccines, in addition to doctor visits to screen for disease. But the law’s authors didn’t reckon with America’s ever-creative medical billing juggernaut.
Over the past several years, the medical industry has eroded the ACA’s guarantees, finding ways to bill patients in gray zones of the law. Patients going in for preventive care, expecting that it will be fully covered by insurance, are being blindsided by bills, big and small.
The problem comes down to deciding exactly what components of a medical encounter are covered by the ACA guarantee. For example, when do conversations between doctor and patient during an annual visit for preventive services veer into the treatment sphere? What screenings are needed for a patient’s annual visit?
A healthy 30-year-old visiting a primary care provider might get a few basic blood tests, while a 50-year-old who is overweight would merit additional screening for Type 2 diabetes.
Making matters more confusing, the annual checkup itself is guaranteed to be “no cost” for women and people age 65 and older, but the guarantee doesn’t apply for men in the 18-64 age range — though many preventive services that require a medical visit (such as checks of blood pressure or cholesterol and screens for substance abuse) are covered.
No wonder what’s covered under the umbrella of prevention can look very different to medical providers (trying to be thorough) and billers (intent on squeezing more dollars out of every medical encounter) than it does to insurers (who profit from narrower definitions).
For patients, the gray zone has become a billing minefield. Here are a few more examples, gleaned from the Bill of the Month project in just the past six months:
Peter Opaskar, 46, of Texas, went to his primary care doctor last year for his preventive care visit — as he’d done before, at no cost. This time, his insurer paid $130.81 for the visit, but he also received a perplexing bill for $111.81. Opaskar learned that he had incurred the additional charge because when his doctor asked if he had any health concerns, he mentioned that he was having digestive problems but had already made an appointment with his gastroenterologist. So, the office explained, his visit was billed as both a preventive physical and a consultation. “Next year,” Opasker said in an interview, if he’s asked about health concerns, “I’ll say ‘no,’ even if I have a gunshot wound.”
Kevin Lin, a technology specialist in Virginia in his 30s, went to a new primary care provider to take advantage of the preventive care benefit when he got insurance; he had no physical complaints. He said he was assured at check-in that he wouldn’t be charged. His insurer paid $174 for the checkup, but he was billed an additional $132.29 for a “new patient visit.” He said he has made many calls to fight the bill, so far with no luck.
Finally, there’s Yoori Lee, 46, of Minnesota, herself a colorectal surgeon, who was shocked when her first screening colonoscopy yielded a bill for $450 for a biopsy of a polyp — a bill she knew was illegal. Federal regulations issued in 2022 to clarify the matter are very clear that biopsies during screening colonoscopies are included in the no-cost promise. “I mean, the whole point of screening is to find things,” she said, stating, perhaps, the obvious.
Though these patient bills defy common sense, room for creative exploitation has been provided by the complex regulatory language surrounding the ACA. Consider this from Ellen Montz, deputy administrator and director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare & Medicaid Services, in an emailed response to queries and an interview request on this subject: “If a preventive service is not billed separately or is not tracked as individual encounter data separately from an office visit and the primary purpose of the office visit is not the delivery of the preventive item or service, then the plan issuer may impose cost sharing for the office visit.”
So, if the doctor decides that a patient’s mention of stomach pain does not fall under the umbrella of preventive care, then that aspect of the visit can be billed separately, and the patient must pay?
And then there’s this, also from Montz: “Whether a facility fee is permitted to be charged to a consumer would depend on whether the facility usage is an integral part of performing the mammogram or an integral part of any other preventive service that is required to be covered without cost sharing under federal law.”
But wait, how can you do a mammogram or colonoscopy without a facility?
Unfortunately, there is no federal enforcement mechanism to catch individual billing abuses. And agencies’ remedies are weak — simply directing insurers to reprocess claims or notifying patients they can resubmit them.
In the absence of stronger enforcement or remedies, CMS could likely curtail these practices and give patients the tools to fight back by offering the sort of clarity the agency provided a few years ago regarding polyp biopsies — spelling out more clearly what comes under the rubric of preventive care, what can be billed, and what cannot.
The stories KFF Health News and NPR receive are likely just the tip of an iceberg. And while each bill might be relatively small compared with the stunning $10,000 hospital bills that have become all too familiar in the United States, the sorry consequences are manifold. Patients pay bills they do not owe, depriving them of cash they could use elsewhere. If they can’t pay, those bills might end up with debt-collection agencies and, ultimately, harm their credit score.
Perhaps most disturbing: These unexpected bills might discourage people from seeking preventive screenings that could be lifesaving, which is why the ACA deemed them “essential health benefits” that should be free.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Herbs For Evidence-Based Health & Healing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Herbs have been used since prehistoric times to treat injuries and illnesses, but which ones actually work, as opposed to being “old wives’ tales”?
Even today, in pharmacies herbals products may come with a disclaimer “based on traditional use only”, which, in scientific terms, means it likely performs no better than placebo.
This is a “Saturday Life Hacks” edition, not a “Research Review Monday”, so we won’t be doing any deep-dives today, and will instead keep things short and snappy. We’ll also spotlight one main benefit, rather than trying to cover all bases, as we often have room to do on a Monday!
Basil
Helps boost immunity:
Chamomile
Significantly reduces symptoms of osteoarthritis:
(This one challenged your writer’s resolve as it does so many things, it was hard to pick just one. So, she went with one that’s less known that “settling the stomach” and “relieving PMS” and “relaxation” and so forth)
Echinacea
Significantly reduces the risk of catching a cold (but won’t help once you’ve caught it):
Echinacea for preventing and treating the common cold
Elderberry
Significantly hastens recovery from upper respiratory viral infections:
Evening Primrose
Fights neuropathy, along with many other benefits:
An updated review on pharmacological activities and phytochemical constituents of evening primrose
Fennel
Antinflammatory, along with many other benefits:
Ginkgo biloba
Antioxidant effects provide anti-aging benefits:
Advances in the Studies of Ginkgo Biloba Leaves Extract on Aging-Related Diseases
Ginseng
Combats fatigue:
Ginseng as a Treatment for Fatigue: A Systematic Review
Lavender
Enjoyed for its sedative effects, which is really does have:
Evidence for Sedative Effects of the Essential Oil of Lavender after Inhalation
Sage
Helps fight HIV type 1 and Herpes simplex type 2 (and probably other viruses, but that’s what we have the science for right now):
Aqueous extracts from peppermint, sage and lemon balm leaves display potent anti-HIV-1 activity
Valerian
Inconclusive data; “traditional use only” for restful sleep.
Can’t have everything!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Menopause: 50 Things You Need to Know – by Dr. Felice Gersh
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can you list 50 important facts about the menopause? If not, you’ll surely find things to learn in here.
The book is divided into three main sections:
- What to expect in perimenopause
- What to expect in early menopause
- What to expect in late menopause
Each section comes with an alarming array of symptoms, ranging from perimenopause fatigue and acne to late menopause tooth loss and vaginal prolapse. This is not to say that everyone will experience everything (fortunately), but rather, that these are the things that can happen and should not arrive unexpected.
Helpfully, of course, Dr. Gersh also gives advice on how to improve your energy and skin health, as well as keep your teeth and vagina in place. And similar professional insights for the rest of the “50 things you need to know”.
The style is like one big (182 pages) patient information leaflet—thus, very clear, explaining everything, and offering reassurance where possible and also what things are reasonable cause for seeking personalized medical attention.
Bottom line: if menopause is in your future, present, or very near past, this is an excellent book for you.
Click here to check out Menopause: 50 Things You Need To Know, and know them!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: