14 Powerful Strategies To Prevent Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia risk starts climbing very steeply after the age of 65, but it’s not entirely predetermined. Dr. Brad Stanfield, a primary care physician, has insights:
The strategies
We’ll not keep them a mystery; they are:
- Cognitive stimulation: which means genuinely challenging mental activities using a variety of mental faculties. This will usually mean that anything that is just “same old, same old” all the time will stop giving benefits after a short while once it becomes rote, and you’ll need something harder and/or different.
- Hearing health: being unable to participate in conversations increases dementia risk; hearing aids can help.
- Eyesight health: similar to the above; regular eye tests are good, and the use of glasses where appropriate.
- Depression management: midlife depression is linked to later life dementia, likely in large part due to social isolation and a lack of stimulation, but either way, treating depression earlier reduces later dementia risk.
- Exercising regularly: what’s good for the heart is good for the brain; the brain is a hungry organ and the blood is what feeds it (and removes things that shouldn’t be there)
- Head injury avoidance: even mild head injuries can cause problems down the road. Protecting one’s head in sports, and even while casually cycling, is important.
- Smoking cessation: just don’t smoke; if you smoke, make it a top priority to quit unless you are given direct strong medical advice to the contrary (there are cases, few and far between, whereby quitting smoking genuinely needs to be deferred until after something else is dealt with first, but they are a lot rarer than a lot of people who are simply afraid of quitting would like to believe)
- Cholesterol management: again, healthy blood means a healthy brain, and that goes for triglycerides too.
- Weight management: obesity, especially waist to hip ratio (indicating visceral abdominal fat specifically) is associated with many woes, including dementia.
- Diabetes management: once again, healthy blood means a healthy brain, and that goes for blood sugar management too.
- Blood pressure management: guess what, healthy blood still means a healthy brain, and that goes for blood pressure too.
- Alcohol reduction/cessation: alcohol is bad for pretty much everything, and for most people who drink, quitting is probably the top thing to do after quitting smoking.
- Social engagement: while we all may have our different preferences on a scale of introversion to extroversion, we are fundamentally a social species and thrive best with social contact, even if it’s just a few people.
- Air pollution reduction: avoiding pollutants, and filtering the air we breathe where pollutants are otherwise unavoidable, makes a measurable difference to brain health outcomes.
For more information on all of these (except the last two, which really he only mentions in passing), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Reduce Your Alzheimer’s Risk ← our own main feature on the topic
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The first pig kidney has been transplanted into a living person. But we’re still a long way from solving organ shortages
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a world first, we heard last week that US surgeons had transplanted a kidney from a gene-edited pig into a living human. News reports said the procedure was a breakthrough in xenotransplantation – when an organ, cells or tissues are transplanted from one species to another. https://www.youtube.com/embed/cisOFfBPZk0?wmode=transparent&start=0 The world’s first transplant of a gene-edited pig kidney into a live human was announced last week.
Champions of xenotransplantation regard it as the solution to organ shortages across the world. In December 2023, 1,445 people in Australia were on the waiting list for donor kidneys. In the United States, more than 89,000 are waiting for kidneys.
One biotech CEO says gene-edited pigs promise “an unlimited supply of transplantable organs”.
Not, everyone, though, is convinced transplanting animal organs into humans is really the answer to organ shortages, or even if it’s right to use organs from other animals this way.
There are two critical barriers to the procedure’s success: organ rejection and the transmission of animal viruses to recipients.
But in the past decade, a new platform and technique known as CRISPR/Cas9 – often shortened to CRISPR – has promised to mitigate these issues.
What is CRISPR?
CRISPR gene editing takes advantage of a system already found in nature. CRISPR’s “genetic scissors” evolved in bacteria and other microbes to help them fend off viruses. Their cellular machinery allows them to integrate and ultimately destroy viral DNA by cutting it.
In 2012, two teams of scientists discovered how to harness this bacterial immune system. This is made up of repeating arrays of DNA and associated proteins, known as “Cas” (CRISPR-associated) proteins.
When they used a particular Cas protein (Cas9) with a “guide RNA” made up of a singular molecule, they found they could program the CRISPR/Cas9 complex to break and repair DNA at precise locations as they desired. The system could even “knock in” new genes at the repair site.
In 2020, the two scientists leading these teams were awarded a Nobel prize for their work.
In the case of the latest xenotransplantation, CRISPR technology was used to edit 69 genes in the donor pig to inactivate viral genes, “humanise” the pig with human genes, and knock out harmful pig genes. https://www.youtube.com/embed/UKbrwPL3wXE?wmode=transparent&start=0 How does CRISPR work?
A busy time for gene-edited xenotransplantation
While CRISPR editing has brought new hope to the possibility of xenotransplantation, even recent trials show great caution is still warranted.
In 2022 and 2023, two patients with terminal heart diseases, who were ineligible for traditional heart transplants, were granted regulatory permission to receive a gene-edited pig heart. These pig hearts had ten genome edits to make them more suitable for transplanting into humans. However, both patients died within several weeks of the procedures.
Earlier this month, we heard a team of surgeons in China transplanted a gene-edited pig liver into a clinically dead man (with family consent). The liver functioned well up until the ten-day limit of the trial.
How is this latest example different?
The gene-edited pig kidney was transplanted into a relatively young, living, legally competent and consenting adult.
The total number of gene edits edits made to the donor pig is very high. The researchers report making 69 edits to inactivate viral genes, “humanise” the pig with human genes, and to knockout harmful pig genes.
Clearly, the race to transform these organs into viable products for transplantation is ramping up.
From biotech dream to clinical reality
Only a few months ago, CRISPR gene editing made its debut in mainstream medicine.
In November, drug regulators in the United Kingdom and US approved the world’s first CRISPR-based genome-editing therapy for human use – a treatment for life-threatening forms of sickle-cell disease.
The treatment, known as Casgevy, uses CRISPR/Cas-9 to edit the patient’s own blood (bone-marrow) stem cells. By disrupting the unhealthy gene that gives red blood cells their “sickle” shape, the aim is to produce red blood cells with a healthy spherical shape.
Although the treatment uses the patient’s own cells, the same underlying principle applies to recent clinical xenotransplants: unsuitable cellular materials may be edited to make them therapeutically beneficial in the patient.
CRISPR technology is aiming to restore diseased red blood cells to their healthy round shape. Sebastian Kaulitzki/Shutterstock We’ll be talking more about gene-editing
Medicine and gene technology regulators are increasingly asked to approve new experimental trials using gene editing and CRISPR.
However, neither xenotransplantation nor the therapeutic applications of this technology lead to changes to the genome that can be inherited.
For this to occur, CRISPR edits would need to be applied to the cells at the earliest stages of their life, such as to early-stage embryonic cells in vitro (in the lab).
In Australia, intentionally creating heritable alterations to the human genome is a criminal offence carrying 15 years’ imprisonment.
No jurisdiction in the world has laws that expressly permits heritable human genome editing. However, some countries lack specific regulations about the procedure.
Is this the future?
Even without creating inheritable gene changes, however, xenotransplantation using CRISPR is in its infancy.
For all the promise of the headlines, there is not yet one example of a stable xenotransplantation in a living human lasting beyond seven months.
While authorisation for this recent US transplant has been granted under the so-called “compassionate use” exemption, conventional clinical trials of pig-human xenotransplantation have yet to commence.
But the prospect of such trials would likely require significant improvements in current outcomes to gain regulatory approval in the US or elsewhere.
By the same token, regulatory approval of any “off-the-shelf” xenotransplantation organs, including gene-edited kidneys, would seem some way off.
Christopher Rudge, Law lecturer, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Blood-Brain Barrier Breach Blamed For Brain-Fog
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Move Over, Leaky Gut. Now It’s A Leaky Brain.
…which is not a headline that promises good news, and indeed, the only good news about this currently is “now we know another thing that’s happening, and thus can work towards a treatment for it”.
Back in February (most popular media outlets did not rush to publish this, as it rather goes against the narrative of “remember when COVID was a thing?” as though the numbers haven’t risen since the state of emergency was declared over), a team of Irish researchers made a discovery:
❝For the first time, we have been able to show that leaky blood vessels in the human brain, in tandem with a hyperactive immune system may be the key drivers of brain fog associated with long covid❞
~ Dr. Matthew Campbell (one of the researchers)
Let’s break that down a little, borrowing some context from the paper itself:
- the leaky blood vessels are breaching the blood-brain-barrier
- that’s a big deal, because that barrier is our only filter between our brain and Things That Definitely Should Not Go In The Brain™
- a hyperactive immune system can also be described as chronic inflammation
- in this case, that includes chronic neuroinflammation which, yes, is also a major driver of dementia
You may be wondering what COVID has to do with this, and well:
- these blood-brain-barrier breaches were very significantly associated (in lay terms: correlated, but correlated is only really used as an absolute in write-ups) with either acute COVID infection, or Long Covid.
- checking this in vitro, exposure of brain endothelial cells to serum from patients with Long Covid induced the same expression of inflammatory markers.
How important is this?
As another researcher (not to mention: professor of neurology and head of the school of medicine at Trinity) put it:
❝The findings will now likely change the landscape of how we understand and treat post-viral neurological conditions.
It also confirms that the neurological symptoms of long covid are measurable with real and demonstrable metabolic and vascular changes in the brain.❞
~ Dr. Colin Doherty (see mini-bio above)
You can read a pop-science article about this here:
Irish researchers discover underlying cause of “brain fog” linked with long covid
…and you can read the paper in full here:
Want to stay safe?
Beyond the obvious “get protected when offered boosters/updates” (see also: The Truth About Vaccines), other good practices include the same things most people were doing when the pandemic was big news, especially avoiding enclosed densely-populated places, washing hands frequently, and looking after your immune system. For that latter, see also:
Beyond Supplements: The Real Immune-Boosters!
Take care!
Share This Post
- the leaky blood vessels are breaching the blood-brain-barrier
-
Best Salt for Neti Pots?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: What kind of salt is best for neti pots?
A: Non-iodised salt is usually recommended, but really, any human-safe salt is fine. By this we mean for example:
- Sodium chloride (like most kitchen salts),
- Potassium chloride (as found in “reduced sodium” kitchen salts), or
- Magnesium sulfate (also known as epsom salts).
Share This Post
Related Posts
-
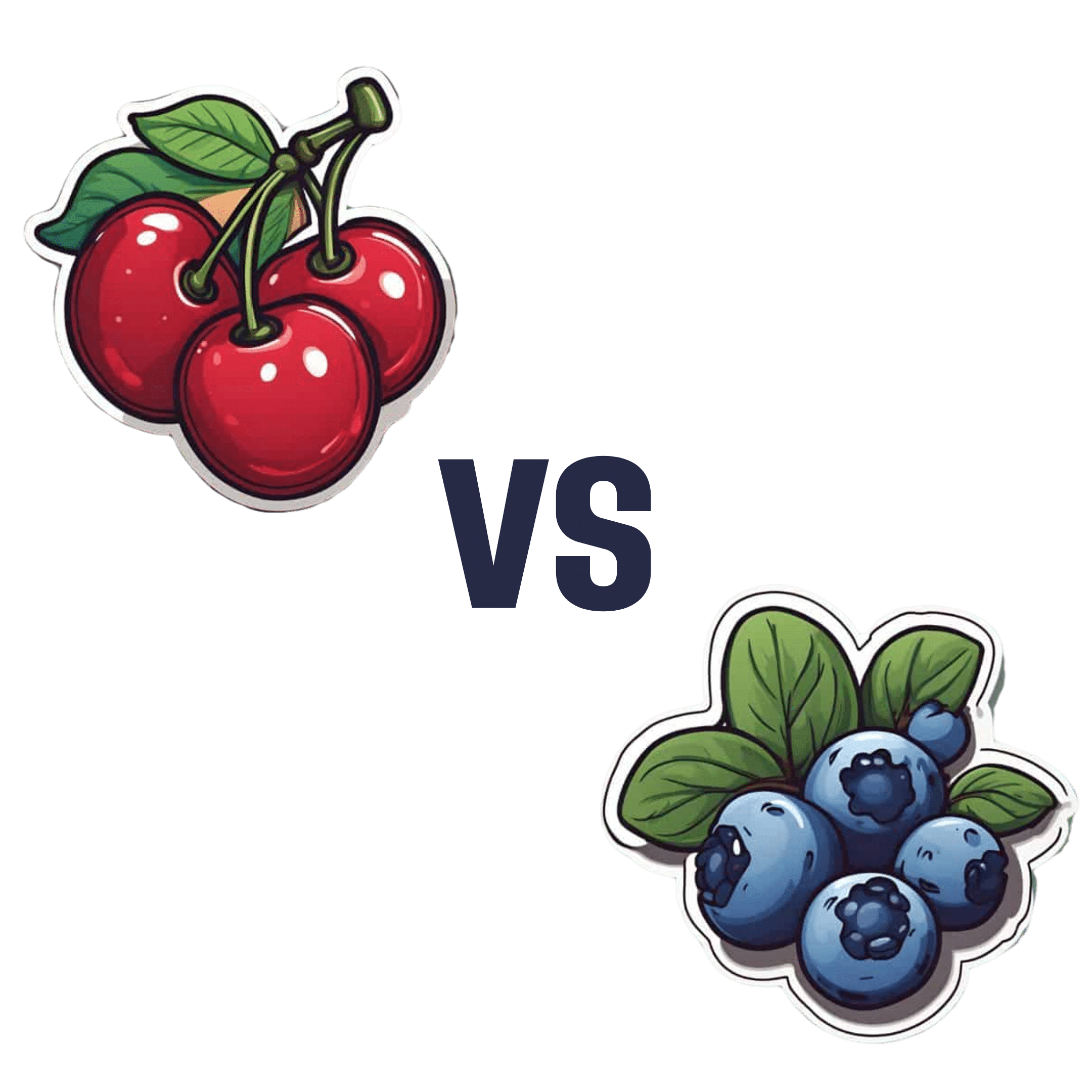
Cherries vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cherries to blueberries, we picked the blueberries.
Why?
It was close! And blueberries only won by virtue of taking an average value for cherries; we could have (if you’ll pardon the phrase) cherry-picked tart cherries for extra benefits that’d put them ahead of blueberries. That’s how close it is.
In terms of macros, they are almost identical, so nothing to set them apart there.
In the category of vitamins, they are mostly comparable except that blueberries have a lot more vitamin K, and cherries have a lot more vitamin A. Since vitamin K is the vitamin that’s scarcer in general, we’ll call blueberries’ vitamin K content a win.
Blueberries do also have about 6x more vitamin E, with a cup of blueberries containing about 10% of the daily requirement (and cherries containing almost none). Another small win for blueberries.
When it comes to minerals, they are mostly comparable; the largest point of difference is that blueberries contain more manganese while cherries contain more copper; nothing to decide between them here.
We’re down to counting amino acids and antioxidants now, so blueberries have a lot more cystine and tyrosine. They also have slightly more of amino acids that they both only have trace amounts of. And as for antioxidants? Blueberries contain notably more quercetin.
So, blueberries win the day—but if we had specified tart cherries rather than taking an average, they could have come out on top. Enjoy both!
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Flexible Dieting Really Means
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Flexibility Is The Dish Of The Day
This is Alan Aragon. Notwithstanding not being a “Dr. Alan Aragon”, he’s a research scientist with dozens of peer-reviewed nutrition science papers to his name, as well as being a personal trainer and fitness educator. Most importantly, he’s an ardent champion of making people’s pursuit of health and fitness more evidence-based.
We’ll be sharing some insights from a book of his that we haven’t reviewed yet, but we will link it at the bottom of today’s article in any case.
What does he want us to know?
First, get out of the 80s and into the 90s
In the world of popular dieting, the 80s were all about calorie-counting and low-fat diets. They did not particularly help.
In the 90s, it was discovered that not only was low-fat not the way to go, but also, regardless of the diet in question, rigid dieting leads to “disinhibition”, that is to say, there comes a point (usually not far into a diet) whereby one breaks the diet, at which point, the floodgates open and the dieter binges unhealthily.
Aragon would like to bring our attention to a number of studies that found this in various ways over the course of the 90s measuring various different metrics including rigid vs flexible dieting’s impacts on BMI, weight gain, weight loss, lean muscle mass changes, binge-eating, anxiety, depression, and so forth), but we only have so much room here, so here’s a 1999 study that’s pretty much the culmination of those:
Flexible vs. Rigid Dieting Strategies: Relationship with Adverse Behavioral Outcomes
So in short: trying to be very puritan about any aspect of dieting will not only not work, it will backfire.
Next, get out of the 90s into the 00s
…which is not only fun if you read “00s” out loud as “naughties”, but also actually appropriate in this case, because it is indeed important to be comfortable being a little bit naughty:
In 2000, Dr. Marika Tiggemann found that dichotomous perceptions of food (e.g. good/bad, clean/dirty, etc) were implicated as a dysfunctional cognitive style, and predicted not only eating disorders and mood disorders, but also adverse physical health outcomes:
Dieting and Cognitive Style: The Role of Current and Past Dieting Behaviour and Cognitions
This was rendered clearer, in terms of physical health outcomes, by Dr. Susan Byrne & Dr. Emma Dove, in 2009:
❝Weight loss was negatively associated with pre-treatment depression and frequency of treatment attendance, but not with dichotomous thinking. Females who regard their weight as unacceptably high and who think dichotomously may experience high levels of depression irrespective of their actual weight, while depression may be proportionate to the degree of obesity among those who do not think dichotomously❞
Aragon’s advice based on all this: while yes, some foods are better than others, it’s more useful to see foods as being part of a spectrum, rather than being absolutist or “black and white” about it.
Next: hit those perfect 10s… Imperfectly
The next decade expanded on this research, as science is wont to do, and for this one, Aragon shines a spotlight on Dr. Alice Berg’s 2018 study with obese women averaging 69 years of age, in which…
In other words (and in fact, to borrow Dr. Berg’s words from that paper),
❝encouraging a flexible approach to eating behavior and discouraging rigid adherence to a diet may lead to better intentional weight loss for overweight and obese older women❞
You may be wondering: what did this add to the studies from the 90s?
And the key here is: rather than being observational, this was interventional. In other words, rather than simply observing what happened to people who thought one way or another, this study took people who had a rigid, dichotomous approach to food, and gave them a 6-month behavioral intervention (in other words, support encouraging them to be more flexible and open in their approach to food), and found that this indeed improved matters for them.
Which means, it’s not a matter of fate or predisposition, as it could have been back in the 90s, per “some people are just like that; who’s to say which factor causes which”. Instead, now we know that this is an approach that can be adopted, and it can be expected to work.
Beyond weight loss
Now, so far we’ve talked mostly about weight loss, and only touched on other health outcomes. This is because:
- weight loss a very common goal for many
- it’s easy to measure so there’s a lot of science for it
Incidentally, if it’s a goal of yours, here’s what 10almonds had to say about that, along with two follow-up articles for other related goals:
Spoiler: we agree with Aragon, and recommend a relaxed and flexible approach to all three of these things
Aragon’s evidence-based approach to nutrition has found that this holds true for other aspects of healthy eating, too. For example…
To count or not to count?
It’s hard to do evidence-based anything without counting, and so Aragon talks a lot about this. Indeed, he does a lot of counting in scientific papers of his own, such as:
and
The effect of protein timing on muscle strength and hypertrophy: a meta-analysis
…as well as non-protein-related but diet-related topics such as:
But! For the at-home health enthusiast, Aragon recommends that the answer to the question “to count or not to count?” is “both”:
- Start off by indeed counting and tracking everything that is important to you (per whatever your current personal health intervention is, so it might be about calories, or grams of protein, or grams of carbs, or a certain fat balance, or something else entirely)
- Switch to a more relaxed counting approach once you get used to the above. By now you probably know the macros for a lot of your common meals, snacks, etc, and can tally them in your head without worrying about weighing portions and knowing the exact figures.
- Alternatively, count moderately standardized portions of relevant foods, such as “three servings of beans or legumes per day” or “no more than one portion of refined carbohydrates per day”
- Eventually, let habit take the wheel. Assuming you have established good dietary habits, this will now do you just fine.
This latter is the point whereby the advice (that Aragon also champions) of “allow yourself an unhealthy indulgence of 10–20% of your daily food”, as a budget of “discretionary calories”, eventually becomes redundant—because chances are, you’re no longer craving that donut, and at a certain point, eating foods far outside the range of healthiness you usually eat is not even something that you would feel inclined to do if offered.
But until that kicks in, allow yourself that budget of whatever unhealthy thing you enjoy, and (this next part is important…) do enjoy it.
Because it is no good whatsoever eating that cream-filled chocolate croissant and then feeling guilty about it; that’s the dichotomous thinking we had back in the 80s. Decide in advance you’re going to eat and enjoy it, then eat and enjoy it, then look back on it with a sense of “that was enjoyable” and move on.
The flipside of this is that the importance of allowing oneself a “little treat” is that doing so actively helps ensure that the “little treat” remains “little”. Without giving oneself permission, then suddenly, “well, since I broke my diet, I might as well throw the whole thing out the window and try again on Monday”.
On enjoying food fully, by the way:
Mindful Eating: How To Get More Nutrition Out Of The Same Food
Want to know more from Alan Aragon?
Today we’ve been working heavily from this book of his; we haven’t reviewed it yet, but we do recommend checking it out:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Your Metabolism Says About How Aggressive Breast Cancer Is Likely To Be For You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ll get straight to it:
More than 120 million Americans have diabetes or pre-diabetes, and Triple-Negative Breast Cancer (TNBC)* is the most aggressive breast cancer form.
These may seem like unrelated statements, until we consider that patients with obesity-driven** diabetes have much worse TNBC outcomes.
*The “triple-negative” refers to:
- the cancer cells don’t have estrogen receptors
- the cancer cells don’t have progesterone receptors
- the cancer cells don’t make the protein HER2, or at least not in clinically relevant amounts.
**with regard to “obesity-driven”, that is what it is called, and the presence of excess fat does play an important role as we will see, but the fundamental culprit is insulin resistance, as we will also see.
The connection
Superficially, the connection between obesity-driven diabetes and worse TNBC outcomes could be put down to “a person who is already unhealthy will generally fare worse in most health things than an otherwise healthy person”. And, in and of itself, that’s a fair point. Comorbidities certainly do tend to flock together and make each other worse.
On the flipside, this does also mean that the more points of good health we have in our favor, the greater our chances of faring better if something (such as a cancer) does strike us regardless. So, there’s a fair motivation to always keep on top of all aspects of health, so far as reasonably possible.
However, there’s more to it than that.
Dr. Naomi Ko et al., a team of researchers at Boston University, found that diabetes alters breast cancer biology, making TNBC more aggressive and increasing the risk of brain metastasis (i.e., the cancer spreading to the brain).
Specifically, exosomes from fat cells carry microRNAs that worsen TNBC behavior, enhancing the cancer’s:
- cell growth
- movement
- survival under stress
- brain colonization
This also means that certain microRNA patterns predict breast cancer progression and/or survival.
You can find the paper itself here:
Insulin Resistance Increases TNBC Aggressiveness and Brain Metastasis via Adipocyte-derived Exosomes
Why this matters
The researchers argue that their findings suggest the need for special monitoring and treatment for TNBC patients with metabolic disorders like diabetes, and that treating underlying conditions (such as diabetes) alongside cancer is likely to improve outcomes.
On an individual level rather than systemic (assuming you, dear reader, to be a private individual who is not, for example, in charge of health policy for a region, or something like that), what this means is:
We must avoid carrying too much excess fat yes, and/but we must also particularly focus on avoiding/reversing insulin resistance, which can be a silent killer even without excess adiposity, because the noticeable signs and symptoms (including blood sugar irregularities) occur only well into insulin resistance, when the poor overworked pancreas can no longer crank out enough insulin to keep things ticking over.
With that in mind, do check out in particular the two following articles:
How To Lose Weight (Healthily!) ← if applicable. If on the other hand you’re already in the “healthy” body fat percentage range of 20–25% for women or 15–20% for men, then losing what fat you have will not be beneficial, and may even be harmful, depending on other factors.
How To Avoid & Reverse Insulin Resistance ← this one’s super-important!
And of course:
How To Triple Your Breast Cancer Survival Chances
And if you want to get really well-informed, then we highly recommend checking out:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: