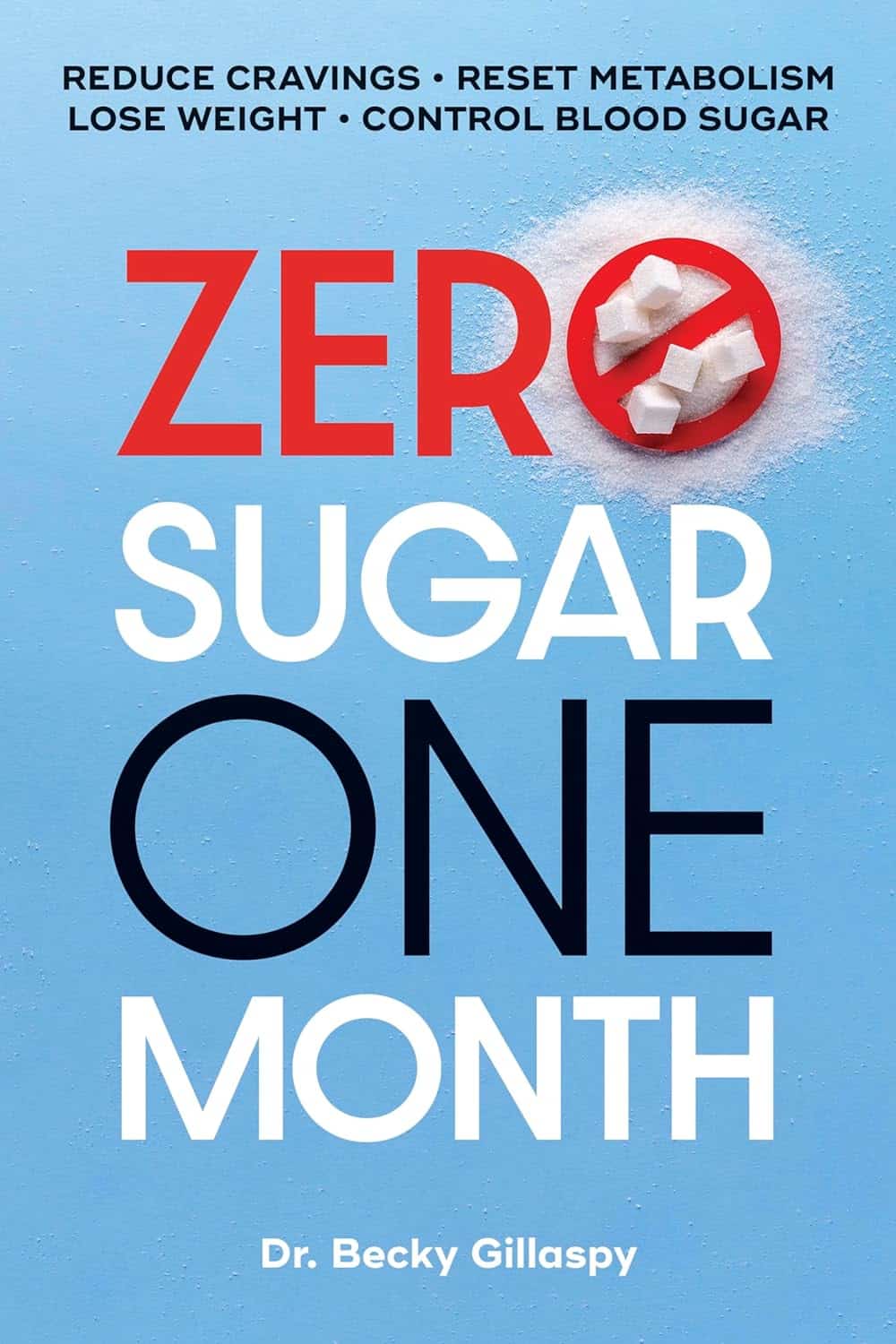
Zero Sugar / One Month – by Becky Gillaspy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about the evils of sugar before, so what makes this one different?
This one has a focus on helping the reader quit it. It assumes we already know the evils of sugar (though it does cover that too).
It looks at the mechanisms of sugar addiction (habits-based and physiological), and how to safely and painlessly cut through those to come out the other side, free from sugar.
The author gives a day-by-day plan, for not only eliminating sugar, but also adding and including things to fill the gap it leaves, keeping us sated, energized, and happy along the way.
In the category of subjective criticism, it does also assume we want to lose weight, which may not be the case for many readers. But that’s a by-the-by and doesn’t detract from the useful guide to quitting sugar, whatever one’s reasons.
Bottom line: if you would like to quit sugar but find it hard, this book thinks of everything and walks you by the hand, making it easy.
Click here to check out Zero Sugar / One Month, and reap the health benefits!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Snooze-Button Controversy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
To Snooze Or Not To Snooze? (Science Has Answers)
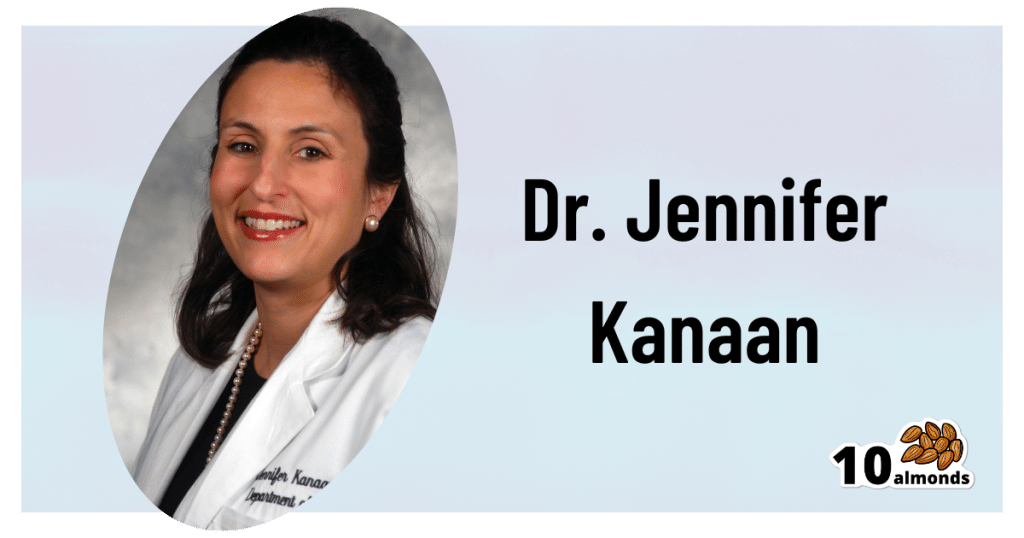
This is Dr. Jennifer Kanaan. She’s a medical doctor with a focus on pulmonary critical care, sleep disorders, and sleep medicine.
What does she want to tell us?
She wants us to be wary of the many news articles that have jumped on a certain recent sleep study, such as:
- Is hitting the snooze button really a bad idea? Study sheds light on the impact of morning alarms on sleep and cognition
- Hitting Snooze May Help You Feel Less Sleepy and More Alert, Research Says
- Is it okay to press the snooze button?
- Hitting Snooze May Help You Feel Less Sleepy and More Alert, Research Says
- Hitting the snooze button on your alarm doesn’t make you more tired
For the curious, here is the paper itself, by Dr. Tina Sundelin et al. It’s actually two studies, by the way, but one paper:
The authors of this study concluded:
❝There were no clear effects of snoozing on the cortisol awakening response, morning sleepiness, mood, or overnight sleep architecture.
A brief snooze period may thus help alleviate sleep inertia, without substantially disturbing sleep, for late chronotypes and those with morning drowsiness.❞
Notably, people tend to snooze because an alarm clock will, if not “smart” about it, wake us up mid sleep-cycle more often than not, and that will produce a short “sleep hangover”. By snoozing, we are basically re-rolling the dice on being woken up between sleep cycles, and thus feeling more refreshed.
What’s Dr. Kanaan’s counterpoint?
Dr. Kanaan says:
❝If you’re coming in and out of sleep for 30 minutes, after the alarm goes off the first time, you’re costing yourself 30 minutes of uninterrupted, quality, restorative sleep. This study doesn’t change that fact.❞
She advises that rather than snoozing, we should prioritize getting good sleep in the first place, and once we do wake up, mid sleep-cycle or not, get sunlight. That way, our brain will start promptly scrubbing melatonin and producing the appropriate wakefulness hormones instead. That means serotonin, and also a spike of cortisol.
Remember: cortisol is only bad when it’s chronically elevated. It’s fine, and even beneficial, to have a short spike of cortisol. We make it for a reason!
If you’d like to hear more from Dr. Kanaan, you might like this interview with her at the University of Connecticut:
Want the best of both worlds?
A great option to avoid getting woken in the middle of a sleep cycle, and also not needing to hit snooze, is a sunrise alarm clock. Specifics of these devices vary, but for example, the kind this writer has starts gently glowing an hour before the set alarm time,and gradually gets brighter and lighter over the course of the hour.
We don’t sell them, but here’s an example sunrise alarm clock on Amazon, for your convenience
Share This Post
-
High-Protein Plant-Based Diet for Beginners – by Maya Howard with Ariel Warren
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Seasoned vegans (well-seasoned vegans?) will know that getting enough protein from a plant-based diet is really not the challenge that many think it is, but for those just embarking on cutting out the meat, it’s not useful to say “it’s easy!”; it’s useful to show how.
That’s what this book does. And not just by saying “these foods” and leaving people to wonder if they need to eat a pound of tofu each day to get their protein in. Instead, recipes. Enough for a 4-week meal plan, and the idea is that after a month of eating that way, it won’t be nearly so mysterious.
The recipes are very easy to execute, while still having plenty of flavor (which is what happens when one uses a lot of flavorsome main ingredients and then seasons them well too). The ingredients are not obscure, and you should be able to find everything easily in any medium-sized supermarket.
As for the well-roundedness of the diet, we’ll mention that the “with Ariel Warren” in the by-line means that while the book was principally authored by Maya Howard (who is, at time of writing, a nutritionist-in-training), she had input throughout from Ariel Warren (a Registered Dietician Nutritionist) to ensure she didn’t go off-piste anyway and it gets the professional stamp of approval.
Bottom line: if you’d like to cook plant based while still prioritizing protein and you’re not sure how to make that exciting and fun instead of a chore, then this book will show you how to please your taste buds and improve your body composition at the same time.
Click here to check out High-Protein Plant-Based Diet for Beginners, and dig in!
Share This Post
-
Peas vs Broad Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peas to broad beans, we picked the peas.
Why?
Both are great of course, but…
Looking at the macros to start with, peas have more protein and more fiber. The differences aren’t huge, but they are clear.
In terms of vitamins, peas have more of vitamins A, B1, B2, B3, B5, B6, B9, E, K, and choline (some with very large margins, some with small), while broad beans contain a little more vitamin C (the margin is quite narrow though).
When it comes to minerals, peas have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while broad beans have more sodium. So this category wasn’t close.
Adding up the win from each of the categories makes for a clear triple-win for peas.
Easy-peasy!
Want to learn more?
You might like to read:
Take care!
Share This Post
Related Posts
-
Shame and blame can create barriers to vaccination
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Understanding the stigma surrounding infectious diseases like HIV and mpox may help community health workers break down barriers that hinder access to care.
Looking back in history can provide valuable lessons to confront stigma in health care today, especially toward Black, Latine, LGBTQ+, and other historically underserved communities disproportionately affected by COVID-19 and HIV.
Public Good News spoke with Sam Brown, HIV prevention and wellness program manager at Civic Heart, a community-based organization in Houston’s historic Third Ward, to understand the effects of stigma around sexual health and vaccine uptake.
Brown shared more about Civic Heart’s efforts to provide free confidential testing for sexually transmitted infections, counseling and referrals, and information about COVID-19, flu, and mpox vaccinations, as well as the lessons they’re learning as they strive for vaccine equity.
Here’s what Brown said.
[Editor’s note: This content has been edited for clarity and length.]
PGN: Some people on social media have spread the myth that vaccines cause AIDS or other immune deficiencies when the opposite is true: Vaccines strengthen our immune systems to help protect against disease. Despite being frequently debunked, how do false claims like these impact the communities you serve?
Sam Brown: Misinformation like that is so hard to combat. And it makes the work and the path to overall community health hard because people will believe it. In the work that we do, 80 percent of it is changing people’s perspective on something they thought they knew.
You know, people don’t even transmit AIDS. People transmit HIV. So, a vaccine causing immunodeficiency doesn’t make sense.
With the communities we serve, we might have a person that will believe the myth, and because they believe it, they won’t get vaccinated. Then later, they may test positive for COVID-19.
And depending on social determinants of health, it can impact them in a whole heap of ways: That person is now missing work, they’re not able to provide for their family—if they have a family. It’s this mindset that can impact a person’s life, their income, their ability to function.
So, to not take advantage of something like a vaccine that’s affordable, or free for the most part, just because of misinformation or a misunderstanding—that’s detrimental, you know.
For example, when we talk to people in the community, many don’t know that they can get mpox from their pet, or that it’s zoonotic—that means that it can be transferred between different species or different beings, from animals to people. I see a lot of surprise and shock [when people learn this].
It’s difficult because we have to fight the misinformation and the stigma that comes with it. And it can be a big barrier.
People misunderstand. [They] think that “this is something that gay people or the LGBTQ+ community get,” which is stigmatizing and comes off as blaming. And blaming is the thing that leads us to be misinformed.
PGN: In the last couple years, your organization’s HIV Wellness program has taken on promoting COVID-19, flu, and mpox vaccines to the communities you serve. How do you navigate conversations between sexual health and infectious diseases? Can you share more about your messaging strategies?
S.B.: As we promoted positive sexual health and HIV prevention, we saw people were tired of hearing about HIV. They were tired of hearing about how PrEP works, or how to prevent HIV.
But, when we had an outbreak of syphilis in Houston just last year, people were more inclined to test because of the severity of the outbreak.
So, what our team learned is that sometimes you have to change the message to get people what they need.
We changed our message to highlight more syphilis information and saw that we were able to get more people tested for HIV because we correlated how syphilis and HIV are connected and how a person can be susceptible to both.
Using messages that the community wants and pairing them with what the community needs has been better for us. And we see that same thing with COVID-19, the flu, and RSV. Sometimes you just can’t be married to a message. We’ve had to be flexible to meet our clients where they are to help them move from unsafe practices to practices that are healthy and good for them and their communities.
PGN: You’ve mentioned how hard it is to combat stigma in your work. How do you effectively address it when talking to people one-on-one?
S.B.: What I understand is that no one wants to feel shame. What I see people respond to is, “Here’s an opportunity to do something different. Maybe there was information that you didn’t know that caused you to make a bad decision. And now here’s an opportunity to gain information so that you can make a better decision.”
People want to do what they want to do; they want to live how they want to live. And we all should be able to do that as long as it’s not hurting anyone, but also being responsible enough to understand that, you know, COVID-19 is here.
So, instead of shaming and blaming, it’s best to make yourself aware and understand what it is and how to treat it. Because the real enemy is the virus—it’s the infection, not the people.
When we do our work, we want to make sure that we come from a strengths-based approach. We always look at what a client can do, what that client has. We want to make sure that we’re empowering them from that point. So, even if they choose not to prioritize our message right now, we can’t take that personally. We’ll just use it as a chance to try a new way of framing it to help people understand what we’re trying to say.
And sometimes that can be difficult, even for organizations. But getting past that difficulty comes with a greater opportunity to impact someone else.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Exercise to Stop Your Legs From Giving Out
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Doug Weiss, seniors-specialist physio, has an exercise that stops your knees from being tricked into collapsing (which is very common) by a misfiring (also common) reflex.
Step up…
Setup to step up thus:
- Use a sturdy support like a countertop or chair.
- Have an aerobic step or similar firm surface to step onto.
When you’re ready:
- Stand facing away from the step.
- Place one hand on the support for stability.
- Step backwards up onto the step with your right leg, then your left leg, so both feet are on the step.
- Step forward to come back down.
Once you’re confident of the series of movements, do it without the support, and do it for a few minutes each day. Don’t worry about how easy it becomes; this is not, first and foremost, a strength-training exercise; you don’t have to start adding weights or anything (although of course you can if you want).
How it works: there’s a part of you called the Golgi tendon organ, and it can trigger a Golgi tendon reflex, which is one of the body’s equivalents of a steam valve. However, instead of letting off steam to avoid a boiler explosion, it collapses a joint to save it from overload. However, if not exercised regularly, it can get overly sensitive, causing it to mistake your mere bodyweight for an overload. So, it collapses, thinking it is saving you from snapping a tendon, but it’s not. By exercising in the way described, the Golgi tendon reflex will go back to only being triggered by an actual overload, not the mere act of stepping.
Writer’s note: this one’s interesting to me as I have a) a strong lower body b) hypermobile joints that thus occasionally just fold like laundry regardless. Could it be that this will fix that? I guess I’ll find out 🙂
Meanwhile, for more on all of the above plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
What Nobody Teaches You About Strengthening Your Knees
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Beetroot vs Sweet Potato – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to sweet potato, we picked the sweet potato.
Why?
Quite a straightforward one today!
In terms of macros, sweet potato has more protein, carbs, and fiber. The glycemic index of both of these root vegetables is similar (and in each case varies similarly depending on how it is cooked), so we’ll call the winner the one that’s more nutritionally dense—the sweet potato.
Looking at vitamins next, beetroot has more vitamin B9 (and is in fact a very good source of that, unlike sweet potato), and/but sweet potato is a lot higher in vitamins A, B1, B2, B3, B5, B6, B7, C, E, K, and choline. And we’re talking for example more than 582x more vitamin A, more than 17x more vitamin E, more than a 10x more vitamin K, and at least multiples more of the other vitamins mentioned. So this category’s not a difficult one to call for sweet potato.
When it comes to minerals, beetroot has more selenium, while sweet potato has more calcium, copper, magnesium, manganese, phosphorus, and potassium. They’re approximately equal in iron and zinc. Another win for sweet potato.
Of course, enjoy both. But if you’re looking for the root vegetable that’ll bring the most nutrients, it’s the sweet potato.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what else it can do
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: