With all this bird flu around, how safe are eggs, chicken or milk?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Enzo Palombo, Swinburne University of Technology
Recent outbreaks of bird flu – in US dairy herds, poultry farms in Australia and elsewhere, and isolated cases in humans – have raised the issue of food safety.
So can the virus transfer from infected farm animals to contaminate milk, meat or eggs? How likely is this?
And what do we need to think about to minimise our risk when shopping for or preparing food?

How safe is milk?
Bird flu (or avian influenza) is a bird disease caused by specific types of influenza virus. But the virus can also infect cows. In the US, for instance, to date more than 80 dairy herds in at least nine states have been infected with the H5N1 version of the virus.
Investigations are under way to confirm how this happened. But we do know infected birds can shed the virus in their saliva, nasal secretions and faeces. So bird flu can potentially contaminate animal-derived food products during processing and manufacturing.
Indeed, fragments of bird flu genetic material (RNA) were found in cow’s milk from the dairy herds associated with infected US farmers.
However, the spread of bird flu among cattle, and possibly to humans, is likely to have been caused through contact with contaminated milking equipment, not the milk itself.
The test used to detect the virus in milk – which uses similar PCR technology to lab-based COVID tests – is also highly sensitive. This means it can detect very low levels of the bird flu RNA. But the test does not distinguish between live or inactivated virus, just that the RNA is present. So from this test alone, we cannot tell if the virus found in milk is infectious (and capable of infecting humans).

Does that mean milk is safe to drink and won’t transmit bird flu? Yes and no.
In Australia, where bird flu has not been reported in dairy cattle, the answer is yes. It is safe to drink milk and milk products made from Australian milk.
In the US, the answer depends on whether the milk is pasteurised. We know pasteurisation is a common and reliable method of destroying concerning microbes, including influenza virus. Like most viruses, influenza virus (including bird flu virus) is inactivated by heat.
Although there is little direct research on whether pasteurisation inactivates H5N1 in milk, we can extrapolate from what we know about heat inactivation of H5N1 in chicken and eggs.
So we can be confident there is no risk of bird flu transmission via pasteurised milk or milk products.
However, it’s another matter for unpasteurised or “raw” US milk or milk products. A recent study showed mice fed raw milk contaminated with bird flu developed signs of illness. So to be on the safe side, it would be advisable to avoid raw milk products.
How about chicken?
Bird flu has caused sporadic outbreaks in wild birds and domestic poultry worldwide, including in Australia. In recent weeks, there have been three reported outbreaks in Victorian poultry farms (two with H7N3 bird flu, one with H7N9). There has been one reported outbreak in Western Australia (H9N2).
The strains of bird flu identified in the Victorian and Western Australia outbreaks can cause human infection, although these are rare and typically result from close contact with infected live birds or contaminated environments.
Therefore, the chance of bird flu transmission in chicken meat is remote.
Nonetheless, it is timely to remind people to handle chicken meat with caution as many dangerous pathogens, such as Salmonella and Campylobacter, can be found on chicken carcasses.
Always handle chicken meat carefully when shopping, transporting it home and storing it in the kitchen. For instance, make sure no meat juices cross-contaminate other items, consider using a cool bag when transporting meat, and refrigerate or freeze the meat within two hours.
Avoid washing your chicken before cooking to prevent the spread of disease-causing microbes around the kitchen.
Finally, cook chicken thoroughly as viruses (including bird flu) cannot survive cooking temperatures.
Are eggs safe?
The recent Australian outbreaks have occurred in egg-laying or mixed poultry flocks, so concerns have been raised about bird flu transmission via contaminated chicken eggs.
Can flu viruses contaminate chicken eggs and potentially spread bird flu? It appears so. A report from 2007 said it was feasible for influenza viruses to enter through the eggshell. This is because influenza virus particles are smaller (100 nanometres) than the pores in eggshells (at least 200 nm).
So viruses could enter eggs and be protected from cleaning procedures designed to remove microbes from the egg surface.
Therefore, like the advice about milk and meat, cooking eggs is best.
The US Food and Drug Administration recommends cooking poultry, eggs and other animal products to the proper temperature and preventing cross-contamination between raw and cooked food.
In a nutshell
If you consume pasteurised milk products and thoroughly cook your chicken and eggs, there is nothing to worry about as bird flu is inactivated by heat.
The real fear is that the virus will evolve into highly pathogenic versions that can be transmitted from human to human.
That scenario is much more frightening than any potential spread though food.
Enzo Palombo, Professor of Microbiology, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Measles cases are rising—here’s how to protect your family
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The U.S. is currently experiencing a spike in measles cases across several states. Measles a highly contagious and potentially life-threatening disease caused by a virus. The measles-mumps-rubella (MMR) vaccine prevents measles; unvaccinated people put themselves and everyone around them at risk, including babies who are too young to receive the vaccine.
Read on to learn more about measles: what it is, how to stay protected, and what to do if a measles outbreak happens near you.
What are the symptoms of measles?
Measles symptoms typically begin 10 to 14 days after exposure. The disease starts with a fever followed by a cough, runny nose, and red eyes and then produces a rash of tiny red spots on the face and body. Measles can affect anyone, but is most serious for children under 5, immunocompromised people, and pregnant people, who may give birth prematurely or whose babies may have low birth weight as a result of a measles infection.
Measles isn’t just a rash—the disease can cause serious health problems and even death. About one in five unvaccinated people in the U.S. who get measles will be hospitalized and could suffer from pneumonia, dehydration, or brain swelling.
If you get measles, it can also damage your immune system, making you more vulnerable to other diseases.
How do you catch measles?
Measles spreads through the air when an infected person coughs or sneezes. It’s so contagious that unvaccinated people have a 90 percent chance of becoming infected if exposed.
An infected person can spread measles to others before they have symptoms.
Why are measles outbreaks happening now?
The pandemic caused many children to miss out on routine vaccinations, including the MMR vaccine. Delayed vaccination schedules coincided with declining confidence in vaccine safety and growing resistance to vaccine requirements.
Skepticism about the safety and effectiveness of COVID-19 vaccines has resulted in some people questioning or opposing the MMR vaccine and other routine immunizations.
How do I protect myself and my family from measles?
Getting an MMR vaccine is the best way to prevent getting sick with measles or spreading it to others. The CDC recommends that children receive the MMR vaccine at 12 to 15 months and again at 4 to 6 years, before starting kindergarten.
One dose of the MMR vaccine provides 93 percent protection and two doses provide 97 percent protection against all strains of measles. Because some children are too young to be immunized, it’s important that those around them are vaccinated to protect them.
Is the MMR vaccine safe?
The MMR vaccine has been rigorously tested and monitored over 50 years and determined to be safe. Adverse reactions to the vaccine are extremely rare.
Receiving the MMR vaccine is much safer than contracting measles.
What do I do if there’s a measles outbreak in my community?
Anyone who is not fully vaccinated for measles should be immunized with a measles vaccine as soon as possible. Measles vaccines given within 72 hours after exposure may prevent or reduce the severity of disease.
Children as young as 6 months old can receive the MMR vaccine if they are at risk during an outbreak. If your child isn’t fully vaccinated with two doses of the MMR vaccine—or three doses, if your child received the first dose before their first birthday—talk to your pediatrician.
Unvaccinated people who have been exposed to the virus should stay home from work, school, day care, and other activities for 21 days to avoid spreading the disease.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
The Drug & Supplement Combo That Reverses Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So far, its effects have been dramatic (in a good way) in mice; human trials are now underway.
How does it work?
It builds from previous work, in which a Japanese research team created an “anti-aging vaccine”, that responded to a problem more specific than aging as a whole, namely atherosclerosis.
They found that a certain* protein was upregulated (i.e., it was made at a greater rate resulting in greater quantities) in patients (mouse and human alike) with atherosclerosis. So, they immunized the mice against that protein, and long story short, everything improved for them, from their atherosclerosis to general markers of aging—including growing back fur that had been lost due to age-related balding (just like in humans). They also lived longer, as is to be expected of a mouse who is now biologically younger.
*To avoid being mysterious: it was glycoprotein nonmetastatic melanoma protein B, known to its friends as GPNMB.
You may be wondering: how can one be immunized against a protein? If so, do bear in mind, a virus is also a protein. In this case, they developed an RNA vaccine, that works in a similar way to the COVID vaccines we all know and love (albeit with a different target).
You can read about this in abundant detail here: Senolytic vaccination improves normal and pathological age-related phenotypes and increases lifespan in progeroid mice
Hot on the heels of that, new approaches were found, including…
The combination
We’ll not keep you waiting; the combination is dasatinib plus quercetin, or else fisetin alone.
It’s about killing senescent (aging) “zombie cells” while sparing healthy cells, which that drug (dasatinib) and those supplements (quercetin and fisetin) do.
The researchers noted:
❝Senescent cells are resistant to apoptosis, which is governed through the upregulation of senescent cell anti-apoptotic pathways (SCAPs). Compounds were subsequently identified that disrupted the SCAPs, inducing death of senescent cells while leaving healthy cells unaffected. Forty-six potential senolytic agents were discovered through this process. To advance translational efforts, the majority of research has focused on agents with known safety profiles and limited off-target effects (Kirkland and Tchkonia, 2020).
The best characterized senolytic agents are dasatinib, a tyrosine kinase inhibitor approved for use in humans for cancer treatment, and quercetin, a naturally occurring plant flavonoid. The agents have a synergistic effect, making their combination more potent for senescent cell clearance (Zhu et al., 2015). As senescent cells do not divide and accumulate over a period of weeks, they can be administered using an intermittent approach, which further serves to reduce the risk of side effects (Kirkland and Tchkonia, 2020).
In preclinical trials, the combination of dasatinib and quercetin (D + Q) have been found to alleviate numerous chronic medical conditions including vascular stiffness, osteoporosis, frailty, and hepatic stenosis❞
Source: A geroscience motivated approach to treat Alzheimer’s disease: Senolytics move to clinical trials
As to how they expanded on this research:
❝In our study, oral D + Q were intermittently administered to tau transgenic mice with late-stage pathology (approximated to a 70-year-old human with advanced AD) (Musi et al., 2018). The treatment effectively reduced cellular senescence and associated senescence-associated secretory phenotype incidence. The 35 % reduction in neurofibrillary tangles was accompanied by enhanced neuron density, decreased ventricular enlargement, diminished tau accumulation, and restoration of aberrant cerebral blood flow. A subsequent preclinical study validated the findings, reporting that intermittently administered D + Q cleared senescent cells in the central nervous system, reduced amyloid-β plaques, attenuated neuroinflammation, and enhanced cognition❞
Source: Ibid.
And now taking it to humans:
❝The first clinical trial of D + Q for early-stage Alzheimer’s Disease (AD) has completed enrollment (Gonzales et al., 2021). The primary aim of the open-label pilot study was to examine the central nervous system penetrance of D and Q in a small sample of older adults with early-stage AD (NCT04063124). In addition, two placebo-controlled trials of D + Q for neurodegenerative disease are underway (NCT04685590 and NCT04785300).
One of the trials in development is a multi-site, double-blind, randomized, placebo-controlled study of senolytic therapy in older adults with amnestic mild cognitive impairment (MCI) or early-stage dementia (Clinical Dementia Rating Scale (CDR) Global 0.5–1) due to AD (elevated CSF total tau/Aβ42 ratio).
The treatment regimen will consist of 12-weeks of intermittently administered oral D + Q.❞
Source: Ibid.
The study is actually completed now, but its results are not yet published (again, at time of writing). Which means: they have the data, and now they’re writing the paper.
We look forward to providing an update about that, when the paper is published!
In the meantime…
Dasatinib is a drug usually prescribed to people with certain kinds of leukemia, and suffice it to say, it’s prescription-only. And unlike drugs that are often prescribed off-label (such as metformin for weight loss), getting your doctor to prescribe you an anticancer drug is unlikely unless you have the cancer in question.
You may be wondering: how is an anticancer drug helpful against aging? And the answer is that cancer and aging are very interrelated, and both have to do with “these old cells just won’t die, and are using the resources needed for young healthy cells”. So in both cases, killing those “zombie cells” while sparing healthy ones, is what’s needed. However, your doctor will probably not buy that as a reason to prescribe you a drug that is technically chemotherapy.
Quercetin, on the other hand, is a readily-available supplement, as is fisetin, and both have glowing (in a good way) safety profiles.
Want to know more?
You can read more about each of quercetin and fisetin (including how to get them), here:
Enjoy!
Share This Post
-
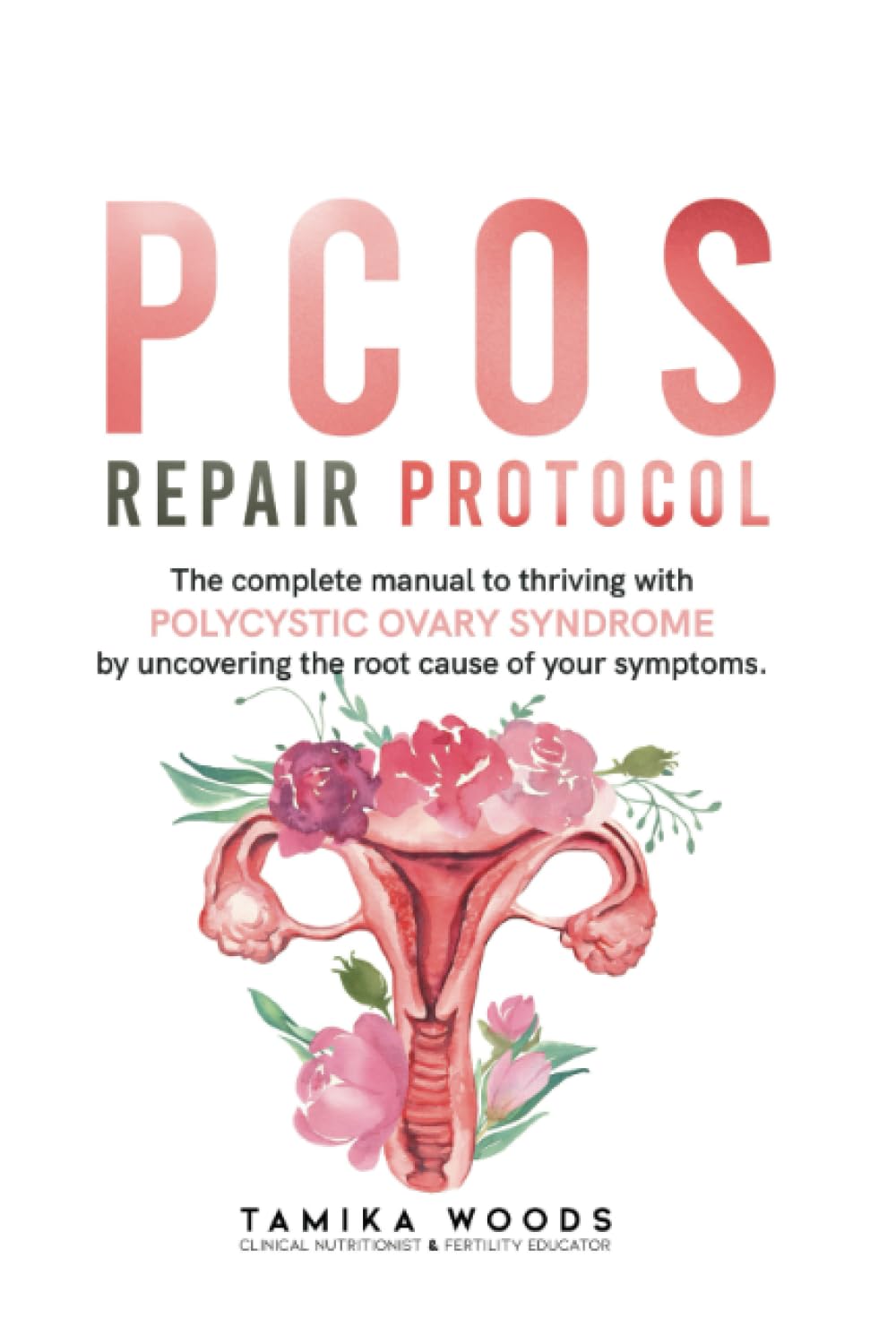
PCOS Repair Protocol – by Tamika Woods
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PCOS (Polycystic Ovary Syndrome) affects about 1 in 5 women, and the general position of the medical establishment is “Oh dear, how sad; never mind”.
…which leaves a lot of people suffering with symptoms with little to no help.
This book looks to address that, and while it doesn’t claim to cure PCOS, it offers a system for managing (including: reducing) the symptoms. The author, a clinical nutritionist by academic background, tackles this in large part via being mindful about what one eats, in the context of the gut and endocrine system specifically.
It’s not just “have a gut healthy diet and eat foods with these nutrients”, though (although yes: also that). Rather, the author walks us through in-depth quizzes and lab testing advice, to advise the reader on how to understand the root cause of your PCOS symptoms, and then address each of those with an individualized management plan.
The style is on the low-end of pop-science, notwithstanding the clinically-informed content. For those who like a very chatty informal approach, you’ll find this one perfect. For those who don’t, well, you won’t find this one perfect, but you will most likely find it informative all the same.
Bottom line: if you or someone you care about (do you know 5 women?) has PCOS, the information in here could make a difference.
Click here to check out PCOS Repair Protocol, and suffer less!
Share This Post
Related Posts
-
One More Resource Against Osteoporosis!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Your Bones Were Made For Moving Too!
We know that to look after bone health, resistance training is generally what’s indicated. Indeed, we mentioned it yesterday, and we’ve talked about it before:
Resistance Is Useful! (Especially As We Get Older)
We also know that if you have osteoporosis already, some exercises are a better or worse idea than others:
Osteoporosis & Exercises: Which To Do (And Which To Avoid)
However! New research suggests that also getting in your recommended 150 minutes per week of moderate exercise slows bone density loss.
The study by Dr. Tiina Savikangas et al. looked at 299 people in their 70s (just over half being women) and found that, over the course of a year, bone mineral density loss was inversely correlated with moderate exercise as recorded by an accelerometer (as found in most fitness-tracking wearables and smartphones).
In other words: those who got more minutes of exercise, kept more bone mineral density.
As well as monitoring bone mineral density, the study also looked at cross-sectional area, but that remained stable throughout.
As for how much is needed:
❝Even short bursts of activity can be significant for the skeleton, so we also looked at movement in terms of the number and intensity of individual impacts. For example, walking and running cause impacts of different intensities.
We found that impacts that were comparable to at least brisk walking were associated with better preservation of bone mineral density.❞
Read more: Impacts during everyday physical activity can slow bone loss ← pop-science source, interviewing the lead researcher
On which note, we’ve a small bone to pick…
As a small correction, the pop-science source says that the subjects’ ages ranged from 70 to 85 years; the paper, meanwhile, clearly shows that the age-range was 74.4±3.9 years (shown in the “Results” table), rounded to 74.4 ± 4 years, in the abstract. So, certainly no participant was older than 78 years and four months.
Why this matters: the age range itself may be critical or it might not, but what is important is that this highlights how we shouldn’t just believe figures cited in pop-science articles, and it’s always good to click through to the source!
This paper is a particularly fascinating read if you have time, because—unlike a lot of studies—they really took great care to note what exactly can and cannot be inferred from the data, and how and why.
Especially noteworthy was the diligence with which they either controlled for, or recognized that they could not control for, far more variables than most studies even bother to mention.
This kind of transparency is critical for good science, and we’d love to see more of it!
Want to apply this to your life?
Tracking minutes-of-movement is one of the things that fitness trackers are best at, so connect your favourite app (one of these days we’ll do a fitness tracker comparison article) and get moving!
And as for the other things that fitness trackers do? As it turns out, they do have their strengths and weaknesses, which are good to bear in mind:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Luxurious Longevity Risotto
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pearl barley is not only tasty and fiber-rich, but also, it contains propionic acid, which lowers cholesterol. The fiber content also lowers cholesterol too, of course, by the usual mechanism. The dish’s health benefits don’t end there, though; check out the science section at the end of the recipe!
You will need
- 2 cups pearl barley
- 3 cups sliced chestnut mushrooms
- 2 onions, finely chopped
- 6 large leaves collard greens, shredded
- ½ bulb garlic, finely chopped
- 8 spring onions, sliced
- 1½ quarts low-sodium vegetable stock
- 2 tbsp nutritional yeast
- 1 tbsp chia seeds
- 1 tbsp black pepper, coarse ground
- 1 tsp MSG or 2 tsp low-sodium salt
- 1 tsp rosemary
- 1 tsp thyme
- Extra virgin olive oil, for cooking
- Optional garnish: fresh basil leaves
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a large sauté pan; add the onions and garlic and cook for 5 minutes; add the mushrooms and cook for another 5 minutes.
2) Add the pearl barley and a cup of the vegetable stock. Cook, stirring, until the liquid is nearly all absorbed, and add more stock every few minutes, as per any other risotto. You may or may not use all the stock you had ready. Pearl barley takes longer to cook than rice, so be patient—it’ll be worth the wait!
Alternative: an alternative is to use a slow cooker, adding a quart of the stock at once and coming back about 4 hours later—thus, it’ll take a lot longer, but will require minimal/no supervision.
3) When the pearl barley has softened, become pearl-like, and the dish is taking on a creamy texture, stir in the rest of the ingredients. Once the greens have softened, the dish is done, and it’s time to serve. Add the garnish if using one:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Magic Of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- The Many Health Benefits Of Garlic
- Chia: The Tiniest Seeds With The Most Value
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Unwell Women – by Dr. Elinor Cleghorn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For a demographic that makes up a little over half of the world’s population, women are paradoxically marginalized in healthcare. And in other ways too, but this book is about health.
Dr. Cleghorn had to fight for seven (!) years to get her own lupus condition recognized as such, and continues to have to fight for it to be taken seriously on an ongoing basis. And yet, 95% of the book is not about her and her experiences, but rather, the bigger picture.
The book is divided into sections, by period in history. From Hippocrates to the modern day, Dr. Cleghorn gives us a well-researched, incredibly well-referenced overview of the marginalization of women’s health. Far from being a dry history book in the early parts though, it’s fascinating and engaging throughout.
The modern day sections are part shining a light into dark areas, part practical information-and-advice “did you know this happens, and you can do this about it”, and part emphatic call-to-action to demand better.
Bottom line: this book is in this reviewer’s “top 5 books read this year”, and we highly recommend it to you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: