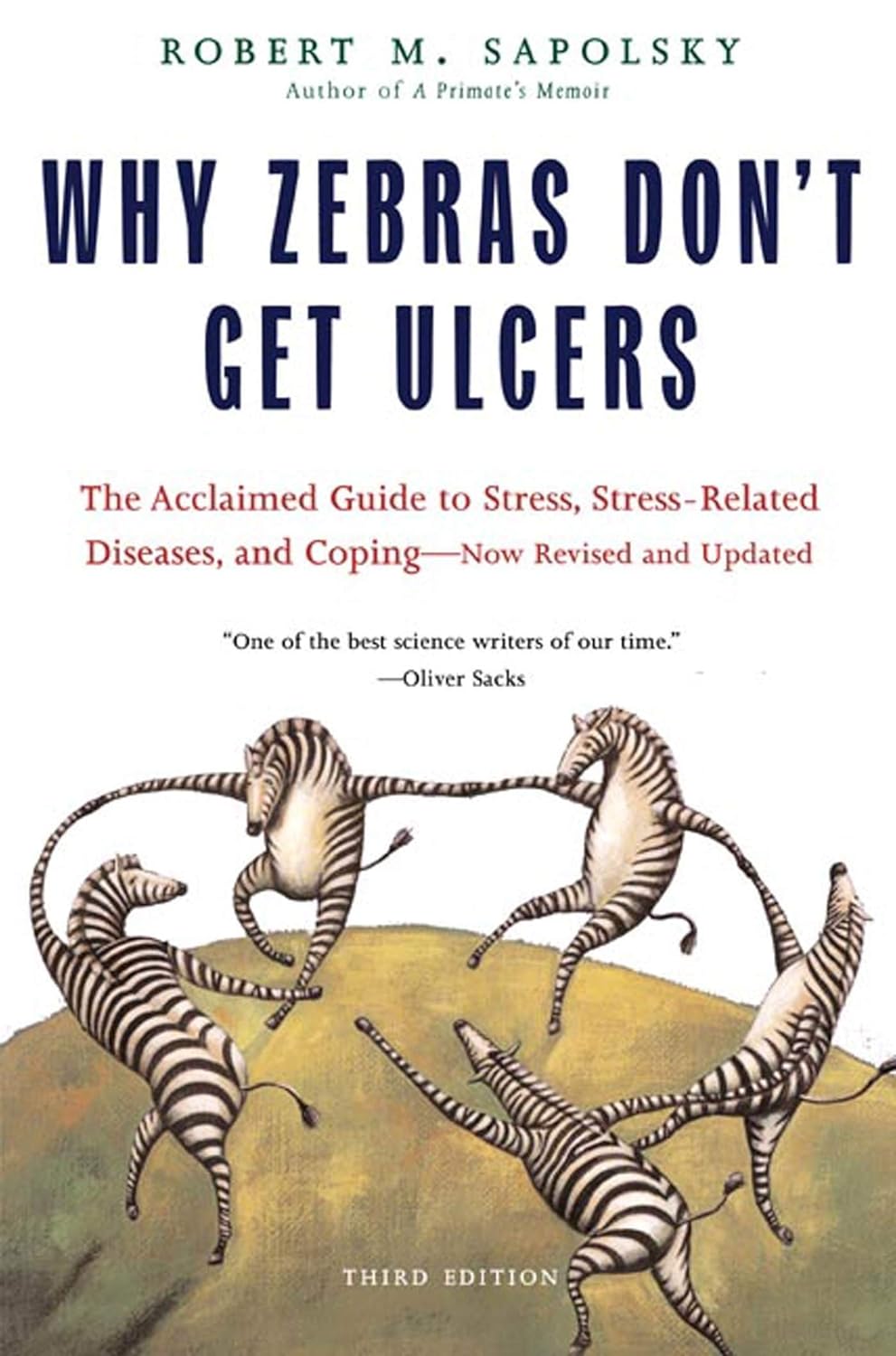
Why Zebras Don’t Get Ulcers – by Dr. Robert M. Sapolsky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book does kick off with a section that didn’t age well—he talks of the stress induced globally by the Spanish Flu pandemic of 1918, and how that kind of thing just doesn’t happen any more. Today, we have much less existentially dangerous stressors!
However, the fact we went and had another pandemic really only adds weight to the general arguments of the book, rather than detracting.
We are consistently beset by “the slings and arrows of outrageous fortune” as Shakespeare would put it, and there’s a reason (or twenty) why many people go grocery-shopping with the cortisol levels of someone being hunted for sport.
So, why don’t zebras get ulcers, as they actually are hunted for food?
They don’t have rent to pay or a mortgage, they don’t have taxes, or traffic, or a broken washing machine, or a project due in the morning. Their problems come one at a time. They have a useful stress response to a stressful situation (say, being chased by lions), and when the danger is over, they go back to grazing. They have time to recover.
For us, we are (usually) not being chased by lions. But we have everything else, constantly, around the clock. So, how to fix that?
Dr. Sapolsky comprehensively describes our physiological responses to stress in quite different terms than many. By reframing stress responses as part of the homeostatic system—trying to get the body back into balance—we find a solution, or rather: ways to help our bodies recover.
The style is “pop-science” and is very accessible for the lay reader while still clearly coming from a top-level academic who is neck-deep in neuroendocrinological research. Best of both worlds!
Bottom line: if you try to take very day at a time, but sometimes several days gang up on you at once, and you’d like to learn more about what happens inside you as a result and how to fix that, this book is for you!
Click here to check out “Why Zebras Don’t Get Ulcers” and give yourself a break!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An unbroken night’s sleep is a myth. Here’s what good sleep looks like
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What do you imagine a good night’s sleep to be?
Often when people come into our sleep clinic seeking treatment, they share ideas about healthy sleep.
Many think when their head hits the pillow, they should fall into a deep and restorative sleep, and emerge after about eight hours feeling refreshed. They’re in good company – many Australians hold the same belief.
In reality, healthy sleep is cyclic across the night, as you move in and out of the different stages of sleep, often waking up several times. Some people remember one or more of these awakenings, others do not. Let’s consider what a healthy night’s sleep looks like.
Bricolage/Shutterstock Sleep cycles are a roller-coaster
As an adult, our sleep moves through different cycles and brief awakenings during the night. Sleep cycles last roughly 90 minutes each.
We typically start the night with lighter sleep, before moving into deeper sleep stages, and rising again into rapid eye movement (REM) sleep – the stage of sleep often linked to vivid dreaming.
If sleeping well, we get most of our deep sleep in the first half of the night, with REM sleep more common in the second half of the night.
Deepest sleep usually happens during the first half of the night. Verin/Shutterstock Adults usually move through five or six sleep cycles in a night, and it is entirely normal to wake up briefly at the end of each one. That means we might be waking up five times during the night. This can increase with older age and still be healthy. If you’re not remembering these awakenings that’s OK – they can be quite brief.
What does getting a ‘good’ sleep actually mean?
You’ll often hear that adults need between seven and nine hours of sleep per night. But good sleep is about more than the number of hours – it’s also about the quality.
For most people, sleeping well means being able to fall asleep soon after getting into bed (within around 30 minutes), sleeping without waking up for long periods, and waking feeling rested and ready for the day.
You shouldn’t be feeling excessively sleepy during the day, especially if you’re regularly getting at least seven hours of refreshing sleep a night (this is a rough rule of thumb).
But are you noticing you’re feeling physically tired, needing to nap regularly and still not feeling refreshed? It may be worthwhile touching base with your general practitioner, as there a range of possible reasons.
Common issues
Sleep disorders are common. Up to 25% of adults have insomnia, a sleep disorder where it may be hard to fall or stay asleep, or you may wake earlier in the morning than you’d like.
Rates of common sleep disorders such as insomnia and sleep apnoea – where your breathing can partially or completely stop many times during the night – also increase with age, affecting 20% of early adults and 40% of people in middle age. There are effective treatments, so asking for help is important.
Beyond sleep disorders, our sleep can also be disrupted by chronic health conditions – such as pain – and by certain medications.
There can also be other reasons we’re not sleeping well. Some of us are woken by children, pets or traffic noise during the night. These “forced awakenings” mean we may find it harder to get up in the morning, take longer to leave bed and feel less satisfied with our sleep. For some people, night awakenings may have no clear cause.
A good way to tell if these awakenings are a problem for you is by thinking about how they affect you. When they cause feelings of frustration or worry, or are impacting how we feel and function during the day, it might be a sign to seek some help.
If waking up in the night is interfering with your normal day-to-day activities, it may indicate a problem. BearFotos/Shutterstock We also may struggle to get up in the morning. This could be for a range of reasons, including not sleeping long enough, going to bed or waking up at irregular times – or even your own internal clock, which can influence the time your body prefers to sleep.
If you’re regularly struggling to get up for work or family needs, it can be an indication you may need to seek help. Some of these factors can be explored with a sleep psychologist if they are causing concern.
Can my smart watch help?
It is important to remember sleep-tracking devices can vary in accuracy for looking at the different sleep stages. While they can give a rough estimate, they are not a perfect measure.
In-laboratory polysomnography, or PSG, is the best standard measure to examine your sleep stages. A PSG examines breathing, oxygen saturation, brain waves and heart rate during sleep.
Rather than closely examining nightly data (including sleep stages) from a sleep tracker, it may be more helpful to look at the patterns of your sleep (bed and wake times) over time.
Understanding your sleep patterns may help identify and adjust behaviours that negatively impact your sleep, such as your bedtime routine and sleeping environment.
And if you find viewing your sleep data is making you feel worried about your sleep, this may not be useful for you. Most importantly, if you are concerned it is important to discuss it with your GP who can refer you to the appropriate specialist sleep health provider.
Amy Reynolds, Associate Professor in Clinical Sleep Health, Flinders University; Claire Dunbar, Research Associate, Sleep Health, Flinders University; Gorica Micic, Postdoctoral Research Fellow, Clinical Psychologist, Flinders University; Hannah Scott, Research Fellow in Sleep Health, Flinders University, and Nicole Lovato, Associate Professor, Adelaide Institute for Sleep Health, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Lifestyle vs Multiple Sclerosis & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Saray Stancic. She’s another from the ranks of “doctors who got a serious illness and it completely changed how they view the treatment of serious illness”.
In her case, Stancic was diagnosed with multiple sclerosis, and wasn’t impressed with the results from the treatments offered, so (after 8 years of pain, suffering, and many medications, only for her condition to worsen) she set about doing better with an evidence-based lifestyle medicine approach.
After 7 years of her new approach, she would go on to successfully run a marathon and live symptom-free.
All this to say: her approach isn’t a magic quick fix, but it is a serious method for serious results, and after all, while it’d be nice to be magically in perfect health tomorrow, what’s important is being in good health for life, right?
If you’re interested in her impressive story, check out:
Doctor With Multiple Sclerosis On The Collapse Of US Healthcare
If you want to know what she did, then read on…
Six key lifestyle changes
Dr. Stancic credits her recovery to focus on the following evidence-based approaches:
The plant-centered plate
This is critical, and is the one she places most emphasis on. Most chronic diseases are exacerbated, if not outright caused, by chronic inflammation, and one cannot fix that without an anti-inflammatory diet.
An anti-inflammatory diet doesn’t have to be 100% plant-based, but broadly speaking, plants are almost always anti-inflammatory to a greater or lesser degree, while animal products are often pro-inflammatory—especially red meat and unfermented dairy.
For more details, see:
Anti-Inflammatory Diet 101 (What to Eat to Fight Inflammation)
Movement every day
While “exercise is good for you” is in principle not a shocker, remember that her starting point was being in terrible condition with badly flared-up MS.
Important to understand here is that excessive exercise can weaken the immune system and sometimes cause flare-ups of various chronic diseases.
Moving thoroughly and moving often, however, is best. So walking yes, absolutely, but also don’t neglect the rest of your body, do some gentle bodyweight squats (if you can; if you can’t, work up to them), stretch your arms as well as your legs, take all your joints through a full range of motion.
See also:
The Doctor Who Wants Us To Exercise Less, & Move More
Mindful stress management
Stress in life is unavoidable, but how we manage it is up to us. Bad things will continue to happen, great and small, but we can take a deep breath, remember that those things aren’t the boss of us, and deal with it calmly and conscientiously.
Mindfulness-Based Stress Reduction is of course the evidence-based “gold standard” for this, but whatever (not substance-based) method works for you, works for you!
About MBSR:
No-Frills, Evidence-Based Mindfulness
Good sleeping habits
Getting good sleep can be hard for anyone, let alone if you have chronic pain. However, Dr. Stancic advocates for doing whatever we can to get good sleep—which means not just duration (the famous “7–9 hours”), but also quality.
Learn more:
The 6 Dimensions Of Sleep (And Why They Matter)
Substance intake awareness
This one’s not so much of a “don’t do drugs, kids” as the heading makes it look. Dr. Stancic assumes we already know, for example, that smoking is bad for us in a long list of ways, and alcohol isn’t much better.
However, she also advises us that in our eagerness to do that plant-based diet, we would do better to go for whole foods plant-based, rather than the latest processed meat substitutes, for example.
And supplements? She bids us exercise caution, and to make sure to get good quality, as poor quality supplements can be worse than taking nothing (looking at you, cheap turmeric supplements that contain heavy metals).
And of course, that nutrients gained from diet will almost always be better than nutrients gained from supplements, as our body can usually use them better.
And see also, some commonly-made supplements mistakes:
Do You Know Which Supplements You Shouldn’t Take Together? (10 Pairs!)
Human connection
Lastly, we humans are a social species by evolution; as individuals, we may enjoy relatively more or less social contact, but having access to such is important not just for our mental health, but our physical health too—we will tend to deteriorate much more quickly when we have to deal with everything alone, all other things being equal.
It doesn’t mean you need a busy social life if that’s not in your nature, but it does mean it’s incredibly beneficial to have at least a small number of people that you trust and whose company you enjoy, at least relatively accessible to you (i.e., their life need not revolve around you, but they are the kind of people who will generally happily spend time with you and provide support when needed if they can).
As for how:
How To Beat Loneliness & Isolation
Want to know more from Dr. Stancic?
We recently reviewed this very good book of hers, which goes over each of these six things in much more detail than we have room for here:
What’s Missing from Medicine – by Dr. Saray Stancic
Enjoy!
Share This Post
-
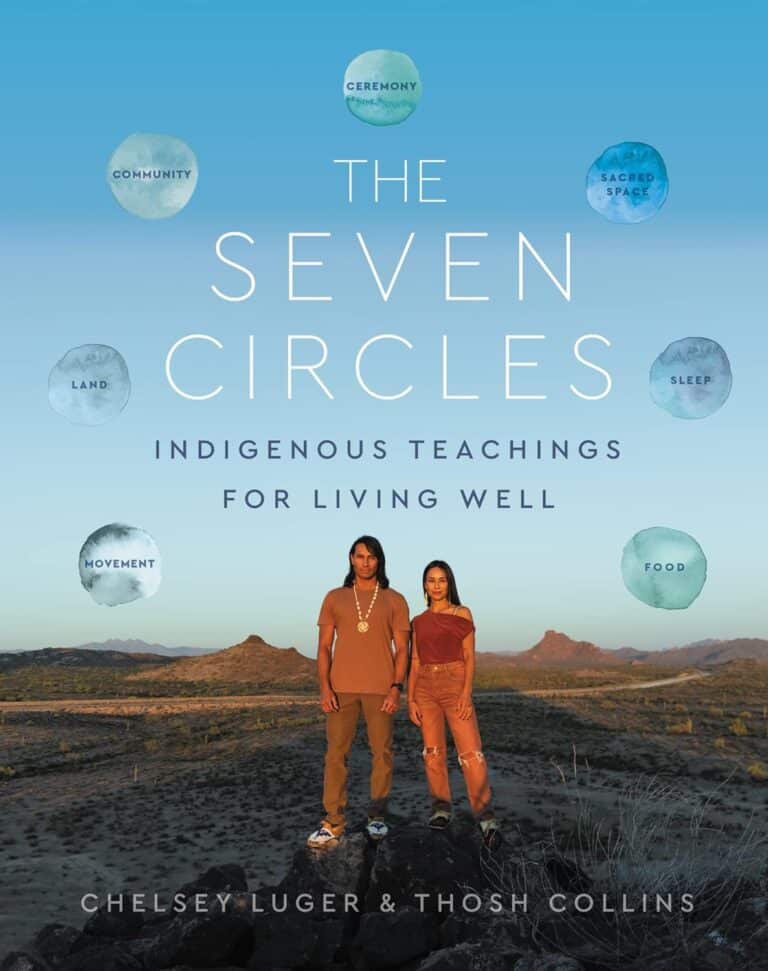
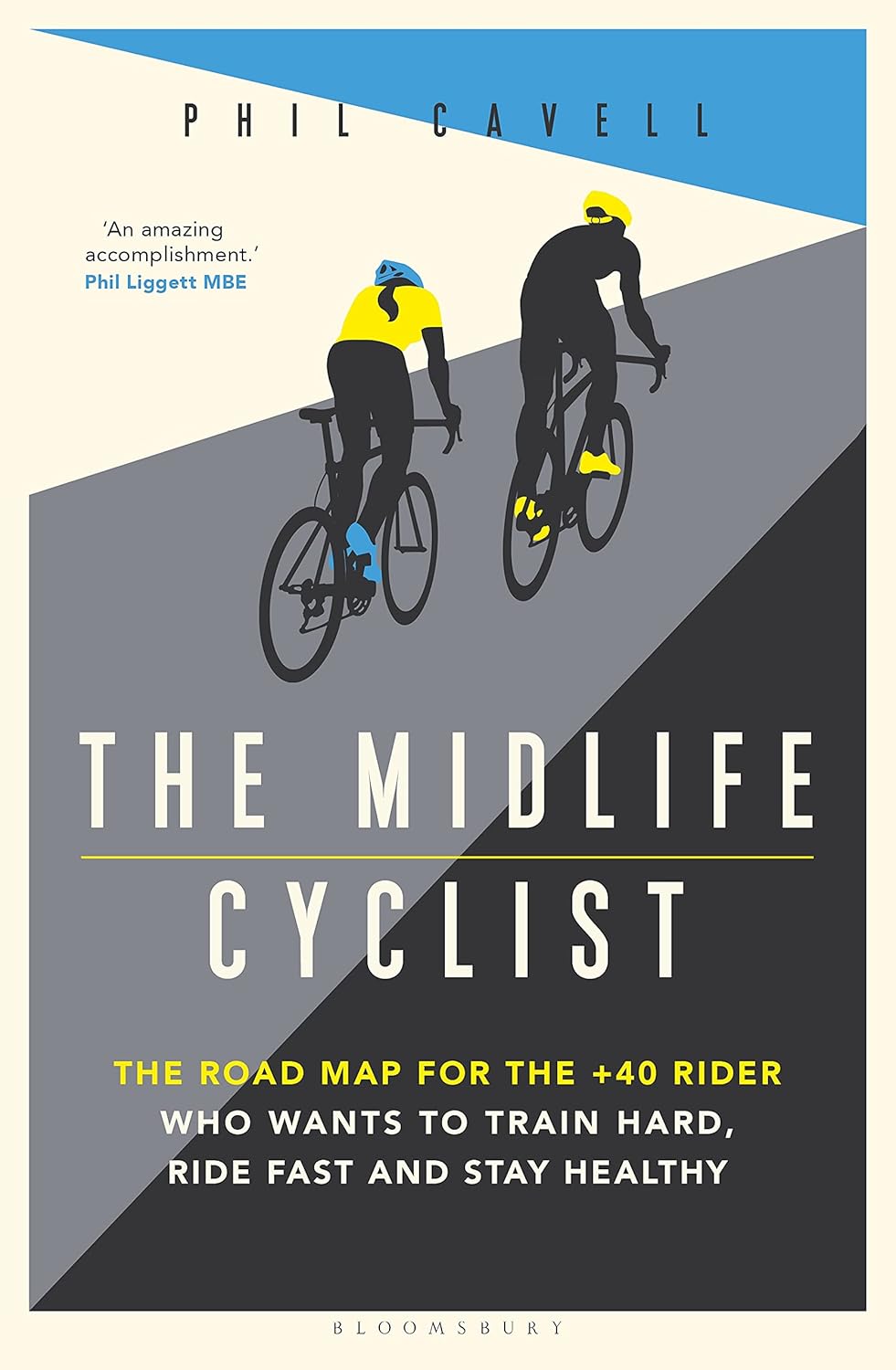
The Midlife Cyclist – by Phil Cavell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether stationary cycling in your living room, or competing in the Tour de France, there’s a lot more to cycling than “push the pedals”—if you want to get good benefits and avoid injury, in any case.
This book explores the benefits of different kinds of cycling, the biomechanics of various body positions, and the physiology of different kinds of performance, and the impact these things have on everything from your joints to your heart to your telomeres.
The style is very much conversational, with science included, and a readiness to acknowledge in cases where the author is guessing or going with a hunch, rather than something being well-evidenced. This kind of honesty is always good to see, and it doesn’t detract from where the science is available and clear.
One downside for some readers will be that while Cavell does endeavour to cover sex differences in various aspects of how they relate to the anatomy and physiology (mostly: the physiology) of cycling, the book is written from a male perspective and the author clearly understands that side of things better. For other readers, of course, this will be a plus.
Bottom line: if you enjoy cycling, or you’re thinking of taking it up but it seems a bit daunting because what if you do it wrong and need a knee replacement in a few years or what if you hurt your spine or something, then this is the book to set your mind at ease, and put you on the right track.
Click here to check out The Midlife Cyclist, and enjoy the cycle of life!
Share This Post
Related Posts
-
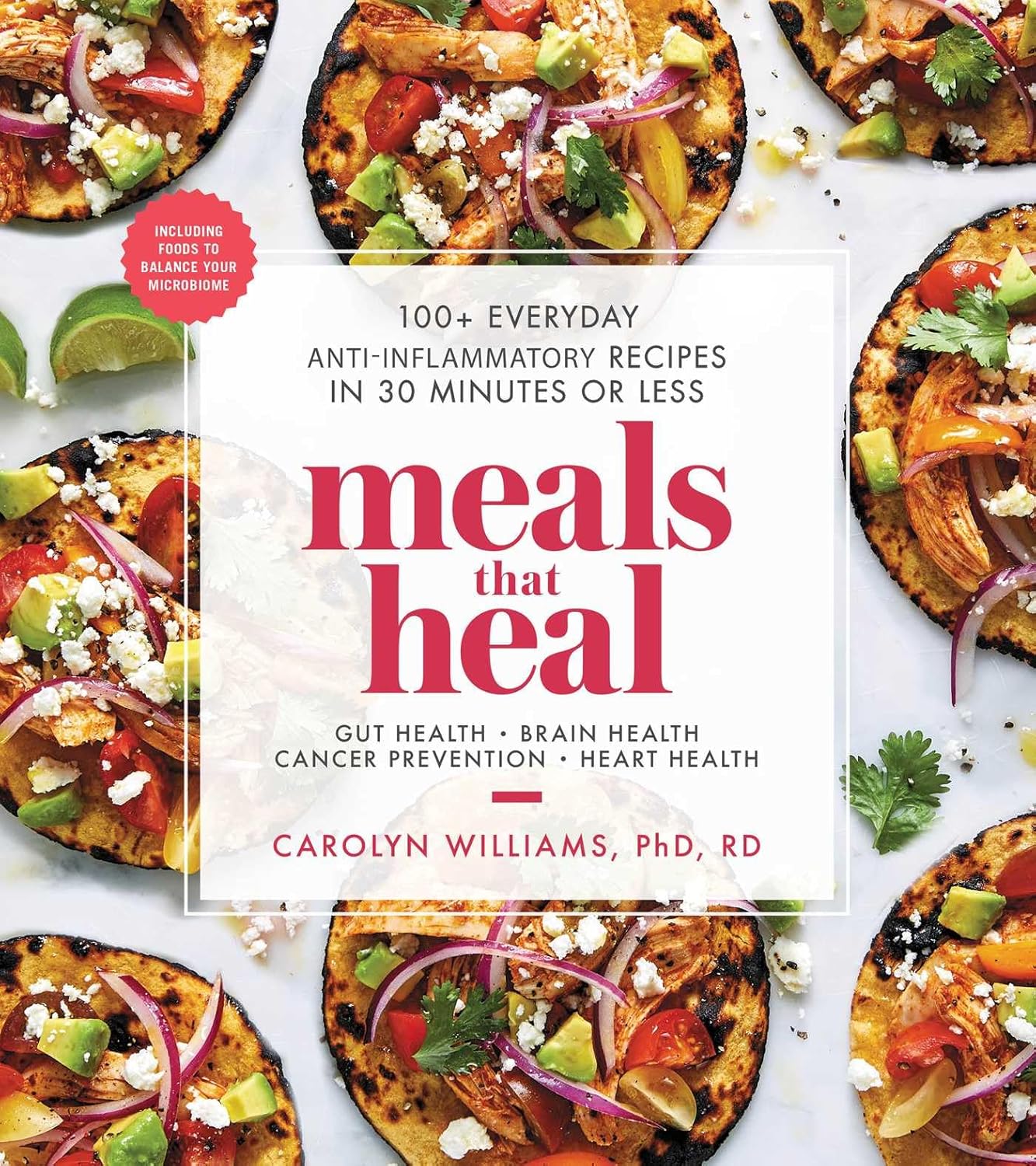
Meals That Heal – by Dr. Carolyn Williams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Inflammation is implicated as a contributory or casual factor in almost all chronic diseases (and still exacerbates the ones in which it’s not directly implicated causally), so if there’s one area of health to focus on with one’s diet, then reducing inflammation is a top candidate.
This book sets about doing exactly that.
You may be wondering whether, per the book’s subtitle, they can really all be done in 30 minutes or under. The answer is: no, not unless you have a team of sous-chefs to do all the prep work for you, and line up everything mise-en-place style for when you start the clock. If you do have that team of sous-chefs working for you, then you can probably do most of them in under 30 minutes. If you don’t have that team, then budget about an hour in total, sometimes less, sometimes more, depending on the recipe.
The recipes themselves are mostly Mediterranean-inspired, though you might want to do a few swaps where the author has oddly recommended using seed oils instead of olive oil, or plant milk in place of where she has used dairy milk in a couple of “recipes” for smoothies. You might also want to be a little more generous with the seasonings, if you’re anything like this reviewer.
Bottom line: if you’re looking for an anti-inflammatory starter cookbook, you could do worse than this. You could probably do better, too, such as starting with The Inflammation Spectrum – by Dr. Will Cole.
Alternatively, click here if you want to check out Meals That Heal, and dive straight in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s the difference between autism and Asperger’s disorder?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Swedish climate activist Greta Thunberg describes herself as having Asperger’s while others on the autism spectrum, such as Australian comedian Hannah Gatsby, describe themselves as “autistic”. But what’s the difference?
Today, the previous diagnoses of “Asperger’s disorder” and “autistic disorder” both fall within the diagnosis of autism spectrum disorder, or ASD.
Autism describes a “neurotype” – a person’s thinking and information-processing style. Autism is one of the forms of diversity in human thinking, which comes with strengths and challenges.
When these challenges become overwhelming and impact how a person learns, plays, works or socialises, a diagnosis of autism spectrum disorder is made.
Where do the definitions come from?
The Diagnostic and Statistical Manual of Mental Disorders (DSM) outlines the criteria clinicians use to diagnose mental illnesses and behavioural disorders.
Between 1994 and 2013, autistic disorder and Asperger’s disorder were the two primary diagnoses related to autism in the fourth edition of the manual, the DSM-4.
In 2013, the DSM-5 collapsed both diagnoses into one autism spectrum disorder.
How did we used to think about autism?
The two thinkers behind the DSM-4 diagnostic categories were Baltimore psychiatrist Leo Kanner and Viennese paediatrician Hans Asperger. They described the challenges faced by people who were later diagnosed with autistic disorder and Asperger’s disorder.
Kanner and Asperger observed patterns of behaviour that differed to typical thinkers in the domains of communication, social interaction and flexibility of behaviour and thinking. The variance was associated with challenges in adaptation and distress.
Kanner and Asperger described different thinking patterns in children with autism.
Roman Nerud/ShutterstockBetween the 1940s and 1994, the majority of those diagnosed with autism also had an intellectual disability. Clinicians became focused on the accompanying intellectual disability as a necessary part of autism.
The introduction of Asperger’s disorder shifted this focus and acknowledged the diversity in autism. In the DSM-4 it superficially looked like autistic disorder and Asperger’s disorder were different things, with the Asperger’s criteria stating there could be no intellectual disability or delay in the development of speech.
Today, as a legacy of the recognition of the autism itself, the majority of people diagnosed with autism spectrum disorder – the new term from the DSM-5 – don’t a have an accompanying intellectual disability.
What changed with ‘autism spectrum disorder’?
The move to autism spectrum disorder brought the previously diagnosed autistic disorder and Asperger’s disorder under the one new diagnostic umbrella term.
It made clear that other diagnostic groups – such as intellectual disability – can co-exist with autism, but are separate things.
The other major change was acknowledging communication and social skills are intimately linked and not separable. Rather than separating “impaired communication” and “impaired social skills”, the diagnostic criteria changed to “impaired social communication”.
The introduction of the spectrum in the diagnostic term further clarified that people have varied capabilities in the flexibility of their thinking, behaviour and social communication – and this can change in response to the context the person is in.
Why do some people prefer the old terminology?
Some people feel the clinical label of Asperger’s allowed a much more refined understanding of autism. This included recognising the achievements and great societal contributions of people with known or presumed autism.
The contraction “Aspie” played an enormous part in the shift to positive identity formation. In the time up to the release of the DSM-5, Tony Attwood and Carol Gray, two well known thinkers in the area of autism, highlighted the strengths associated with “being Aspie” as something to be proud of. But they also raised awareness of the challenges.
What about identity-based language?
A more recent shift in language has been the reclamation of what was once viewed as a slur – “autistic”. This was a shift from person-first language to identity-based language, from “person with autism spectrum disorder” to “autistic”.
The neurodiversity rights movement describes its aim to push back against a breach of human rights resulting from the wish to cure, or fundamentally change, people with autism.
Autism is one of the forms of diversity in human thinking, which comes with strengths and challenges.
Alex and Maria photo/ShutterstockThe movement uses a “social model of disability”. This views disability as arising from societies’ response to individuals and the failure to adjust to enable full participation. The inherent challenges in autism are seen as only a problem if not accommodated through reasonable adjustments.
However the social model contrasts itself against a very outdated medical or clinical model.
Current clinical thinking and practice focuses on targeted supports to reduce distress, promote thriving and enable optimum individual participation in school, work, community and social activities. It doesn’t aim to cure or fundamentally change people with autism.
A diagnosis of autism spectrum disorder signals there are challenges beyond what will be solved by adjustments alone; individual supports are also needed. So it’s important to combine the best of the social model and contemporary clinical model.
Andrew Cashin, Professor of Nursing, School of Health and Human Sciences, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
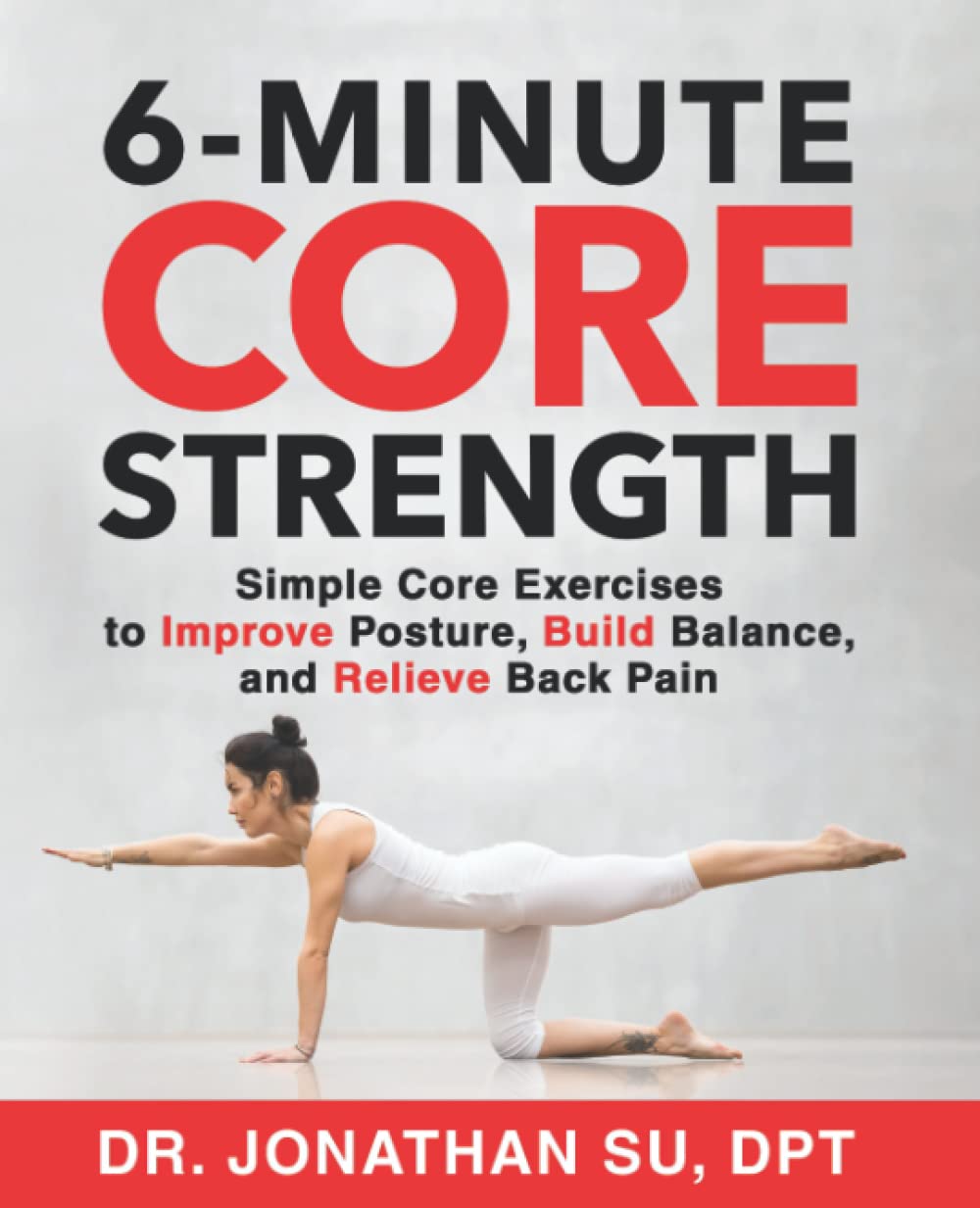
6-Minute Core Strength – by Dr. Jonathan Su
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t normally do author biographies here, but in this case it’s worth noting that Dr. Su is a physiotherapist, military rehab expert, and an IAYT yoga therapist. So, these things together certainly do lend weight to his advice.
About the “6-minute” thing: this is in the style of the famous “7-minute workout” and “5 Minutes’ Physical Fitness” etc, and refers to how long each exercise session should take. The baseline is one such session per day, though of course doing more than one set of 6 minutes each time is a bonus if you wish to do so.
The exercises are focused on core strength, but they also include hip and shoulder exercises, since these are after all attached to the core, and hip and shoulder mobility counts for a lot.
A particular strength of the book is in troubleshooting mistakes of the kind that aren’t necessarily visible from photos; in this case, Dr. Su explains what you need to go for in a certain exercise, and how to know if you are doing it correctly. This alone is worth the cost of the book, in this reviewer’s opinion.
Bottom line: if you want core strength and want it simple yet comprehensive, this book can guide you.
Click here to check out 6-Minute Core Strength, and strengthen yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: