Why is cancer called cancer? We need to go back to Greco-Roman times for the answer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the earliest descriptions of someone with cancer comes from the fourth century BC. Satyrus, tyrant of the city of Heracleia on the Black Sea, developed a cancer between his groin and scrotum. As the cancer spread, Satyrus had ever greater pains. He was unable to sleep and had convulsions.
Advanced cancers in that part of the body were regarded as inoperable, and there were no drugs strong enough to alleviate the agony. So doctors could do nothing. Eventually, the cancer took Satyrus’ life at the age of 65.
Cancer was already well known in this period. A text written in the late fifth or early fourth century BC, called Diseases of Women, described how breast cancer develops:
hard growths form […] out of them hidden cancers develop […] pains shoot up from the patients’ breasts to their throats, and around their shoulder blades […] such patients become thin through their whole body […] breathing decreases, the sense of smell is lost […]
Other medical works of this period describe different sorts of cancers. A woman from the Greek city of Abdera died from a cancer of the chest; a man with throat cancer survived after his doctor burned away the tumour.
Where does the word ‘cancer’ come from?

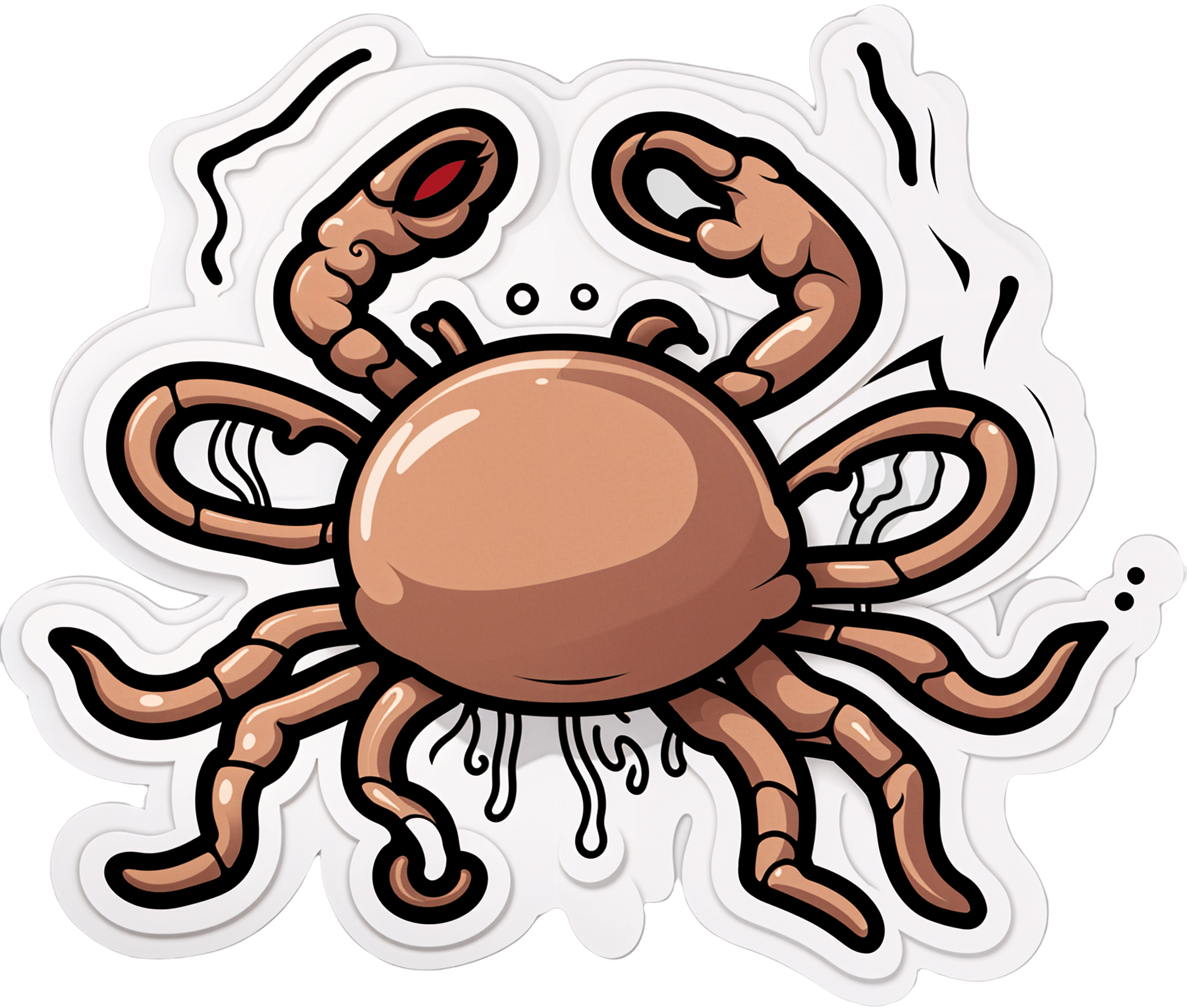
The word cancer comes from the same era. In the late fifth and early fourth century BC, doctors were using the word karkinos – the ancient Greek word for crab – to describe malignant tumours. Later, when Latin-speaking doctors described the same disease, they used the Latin word for crab: cancer. So, the name stuck.
Even in ancient times, people wondered why doctors named the disease after an animal. One explanation was the crab is an aggressive animal, just as cancer can be an aggressive disease; another explanation was the crab can grip one part of a person’s body with its claws and be difficult to remove, just as cancer can be difficult to remove once it has developed. Others thought it was because of the appearance of the tumour.
The physician Galen (129-216 AD) described breast cancer in his work A Method of Medicine to Glaucon, and compared the form of the tumour to the form of a crab:
We have often seen in the breasts a tumour exactly like a crab. Just as that animal has feet on either side of its body, so too in this disease the veins of the unnatural swelling are stretched out on either side, creating a form similar to a crab.
Not everyone agreed what caused cancer
In the Greco-Roman period, there were different opinions about the cause of cancer.
According to a widespread ancient medical theory, the body has four humours: blood, yellow bile, phlegm and black bile. These four humours need to be kept in a state of balance, otherwise a person becomes sick. If a person suffered from an excess of black bile, it was thought this would eventually lead to cancer.
The physician Erasistratus, who lived from around 315 to 240 BC, disagreed. However, so far as we know, he did not offer an alternative explanation.
How was cancer treated?
Cancer was treated in a range of different ways. It was thought that cancers in their early stages could be cured using medications.
These included drugs derived from plants (such as cucumber, narcissus bulb, castor bean, bitter vetch, cabbage); animals (such as the ash of a crab); and metals (such as arsenic).
Galen claimed that by using this sort of medication, and repeatedly purging his patients with emetics or enemas, he was sometimes successful at making emerging cancers disappear. He said the same treatment sometimes prevented more advanced cancers from continuing to grow. However, he also said surgery is necessary if these medications do not work.
Surgery was usually avoided as patients tended to die from blood loss. The most successful operations were on cancers of the tip of the breast. Leonidas, a physician who lived in the second and third century AD, described his method, which involved cauterising (burning):
I usually operate in cases where the tumours do not extend into the chest […] When the patient has been placed on her back, I incise the healthy area of the breast above the tumour and then cauterize the incision until scabs form and the bleeding is stanched. Then I incise again, marking out the area as I cut deeply into the breast, and again I cauterize. I do this [incising and cauterizing] quite often […] This way the bleeding is not dangerous. After the excision is complete I again cauterize the entire area until it is dessicated.
Cancer was generally regarded as an incurable disease, and so it was feared. Some people with cancer, such as the poet Silius Italicus (26-102 AD), died by suicide to end the torment.
Patients would also pray to the gods for hope of a cure. An example of this is Innocentia, an aristocratic lady who lived in Carthage (in modern-day Tunisia) in the fifth century AD. She told her doctor divine intervention had cured her breast cancer, though her doctor did not believe her.

From the past into the future
We began with Satyrus, a tyrant in the fourth century BC. In the 2,400 years or so since then, much has changed in our knowledge of what causes cancer, how to prevent it and how to treat it. We also know there are more than 200 different types of cancer. Some people’s cancers are so successfully managed, they go on to live long lives.
But there is still no general “cure for cancer”, a disease that about one in five people develop in their lifetime. In 2022 alone, there were about 20 million new cancer cases and 9.7 million cancer deaths globally. We clearly have a long way to go.
Konstantine Panegyres, McKenzie Postdoctoral Fellow, Historical and Philosophical Studies, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Junk Food Turns Public Villain as Power Shifts in Washington
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The new Trump administration could be coming for your snacks.
For years, the federal government has steered clear of regulating junk food, fast food, and ultra-processed food.
Now attitudes are changing. Some members of President-elect Donald Trump’s inner circle are gearing up to battle “Big Food,” or the companies that make most of the food and beverages consumed in the United States. Nominees for top health agencies are taking aim at ultra-processed foods that account for an estimated 70% of the nation’s food supply. Based on recent statements, a variety of potential politically charged policy options to regulate ultra-processed food may land on the Trump team menu, including warning labels, changes to agribusiness subsidies, and limits on which products consumers can buy with government food aid.
The push to reform the American diet is being driven largely by conservatives who have taken up the cause that has long been a darling of the left. Trump supporters such as Robert F. Kennedy Jr., whose controversial nomination to lead the Department of Health and Human Services still faces Senate confirmation, are embracing a concept that champions natural foods and alternative medicine. It’s a movement they’ve dubbed “MAHA,” or Make America Healthy Again. Their interest has created momentum because their goals have fairly broad bipartisan support even amid a bitterly divided Congress in which lawmakers from both sides of the aisle focused on the issue last year.
It’s likely to be a pitched battle because the food industry wields immense political influence and has successfully thwarted previous efforts to regulate its products or marketing. The category of “food processing and sales companies,” which includes Tyson Foods and Nestle SA, tallied $26.7 million in spending on lobbying in 2024, according to OpenSecrets. That’s up from almost $10 million in 1998.
“They have been absolutely instrumental and highly, highly successful at delaying any regulatory effectiveness in America,” said Laura Schmidt, a health policy professor at the University of California-San Francisco. “It really does feel like there needs to be a moment of reckoning here where people start asking the question, ‘Why do we have to live like this?’”
“Ultra-processed food” is a widely used term that means different things to different people and is used to describe items ranging from sodas to many frozen meals. These products often contain added fats, starches, and sugars, among other things. Researchers say consumption of ultra-processed foods is linked — in varying levels of intensity — to chronic conditions like diabetes, cancer, mental health problems, and early death.
Nutrition and health leaders are optimistic that a reckoning is already underway. Kennedy has pledged to remove processed foods from school lunches, restrict certain food additives such as dyes in cereal, and shift federal agricultural subsidies away from commodity crops widely used in ultra-processed foods.
The intensifying focus in Washington has triggered a new level of interest on the legal front as lawyers explore cases to take on major foodmakers for selling products they say result in chronic disease.
Bryce Martinez, now 18, filed a lawsuit in December against almost a dozen foodmakers such as Kraft Heinz, The Coca-Cola Co., and Nestle USA. He developed diabetes and non-alcoholic fatty liver disease by age 16, and is seeking to hold them accountable for his illnesses. According to the suit, filed in the Philadelphia Court of Common Pleas, the companies knew or should have known ultra-processed foods were harmful and addictive.
The lawsuit noted that Martinez grew up eating heavily advertised, brand-name foods that are staples of the American diet — sugary soft drinks, Cheerios and Lucky Charms, Skittles and Snickers, frozen and packaged dinners, just to name a few.
Nestle, Coca-Cola, and Kraft Heinz didn’t return emails seeking comment for this article. The Consumer Brands Association, a trade association for makers of consumer packaged goods, disputed the allegations.
“Attempting to classify foods as unhealthy simply because they are processed, or demonizing food by ignoring its full nutrient content, misleads consumers and exacerbates health disparities,” said Sarah Gallo, senior vice president of product policy, in a statement.
Other law firms are on the hunt for children or adults who believe they were harmed by consuming ultra-processed foods, increasing the likelihood of lawsuits.
One Indiana personal injury firm says on its website that “we are actively investigating ultra processed food (UPF) cases.” Trial attorneys in Texas also are looking into possible legal action against the federal regulators they say have failed to police ultra-processed foods.
“If you or your child have suffered health problems that your doctor has linked directly to the consumption of ultra-processed foods, we want to hear your story,” they say on their website.
Meanwhile, the FDA on Jan. 14 announced it is proposing to require a front-of-package label to appear on most packaged foods to make information about a food’s saturated fat, sodium, and added sugar content easily visible to consumers.
And on Capitol Hill, Sens. Bernie Sanders (I-Vt.), Ron Johnson (R-Wis.), and Cory Booker (D-N.J.) are sounding the alarm over ultra-processed food. Sanders introduced legislation in 2024 that could lead to a federal ban on junk food advertising to children, a national education campaign, and labels on ultra-processed foods that say the products aren’t recommended for children. Booker cosigned the legislation along with Sens. Peter Welch (D-Vt.) and John Hickenlooper (D-Colo.).
The Senate Committee on Health, Education, Labor and Pensions held a December hearing examining links between ultra-processed food and chronic disease during which FDA Commissioner Robert Califf called for more funding for research.
Food companies have tapped into “the same neural circuits that are involved in opioid addiction,” Califf said at the hearing.
Sanders, who presided over the hearing, said there’s “growing evidence” that “these foods are deliberately designed to be addictive,” and he asserted that ultra-processed foods have driven epidemics of diabetes and obesity, and hundreds of billions of dollars in medical expenses.
Research on food and addiction “has accumulated to the point where it’s reached a critical mass,” said Kelly Brownell, an emeritus professor at Stanford who is one of the editors of a scholarly handbook on the subject.
Attacks from three sides — lawyers, Congress, and the incoming Trump administration, all seemingly interested in taking up the fight — could lead to enough pressure to challenge Big Food and possibly spur better health outcomes in the U.S., which has the lowest life expectancy among high-income countries.
“Maybe getting rid of highly processed foods in some things could actually flip the switch pretty quickly in changing the percentage of the American public that are obese,” said Robert Redfield, a virologist who led the Centers for Disease Control and Prevention during the previous Trump administration, in remarks at a December event hosted by the Heritage Foundation, a conservative think tank.
Claims that Big Food knowingly manufactured and sold addictive and harmful products resemble the claims leveled against Big Tobacco before the landmark $206 billion settlement was reached in 1998.
“These companies allegedly use the tobacco industry’s playbook to target children, especially Black and Hispanic children, with integrated marketing tie-ins with cartoons, toys, and games, along with social media advertising,” Rene Rocha, one of the lawyers at Morgan & Morgan representing Martinez, told KFF Health News.
The 148-page Martinez lawsuit against foodmakers draws from documents made public in litigation against tobacco companies that owned some of the biggest brands in the food industry.
Similar allegations were made against opioid manufacturers, distributors, and retailers before they agreed to pay tens of billions of dollars in a 2021 settlement with states.
The FDA ultimately put restrictions on the labeling and marketing of tobacco, and the opioid epidemic led to legislation that increased access to lifesaving medications to treat addiction.
But the Trump administration’s zeal in taking on Big Food may face unique challenges.
The ability of the FDA to impose regulation is hampered in part by funding. While the agency’s drug division collects industry user fees, its division of food relies on a more limited budget determined by Congress.
Change can take time because the agency moves at what some critics call a glacial pace. Last year, the FDA revoked a regulation allowing brominated vegetable oil in food products. The agency determined in 1970 that the additive was not generally recognized as safe.
Efforts to curtail the marketing of ultra-processed food could spur lawsuits alleging that any restrictions violate commercial speech protected by the First Amendment. And Kennedy — if he is confirmed as HHS secretary — may struggle to get support from a Republican-led Congress that champions less federal regulation and a president-elect who during his previous term served fast food in the White House.
“The question is, will RFK be able to make a difference?” said David L. Katz, a doctor who founded True Health Initiative, a nonprofit group that combats public health misinformation. “No prior administration has done much in this space, and RFK is linked to a particularly anti-regulatory administration.”
Meanwhile, the U.S. population is recognized as among the most obese in the world and has the highest rate of people with multiple chronic conditions among high-income countries.
“There is a big grassroots effort out there because of how sick we are,” said Jerold Mande, who served as deputy undersecretary for food safety at the Department of Agriculture from 2009 to 2011. “A big part of it is people shouldn’t be this sick this young in their lives. You’re lucky if you get to 18 without a chronic disease. It’s remarkable.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
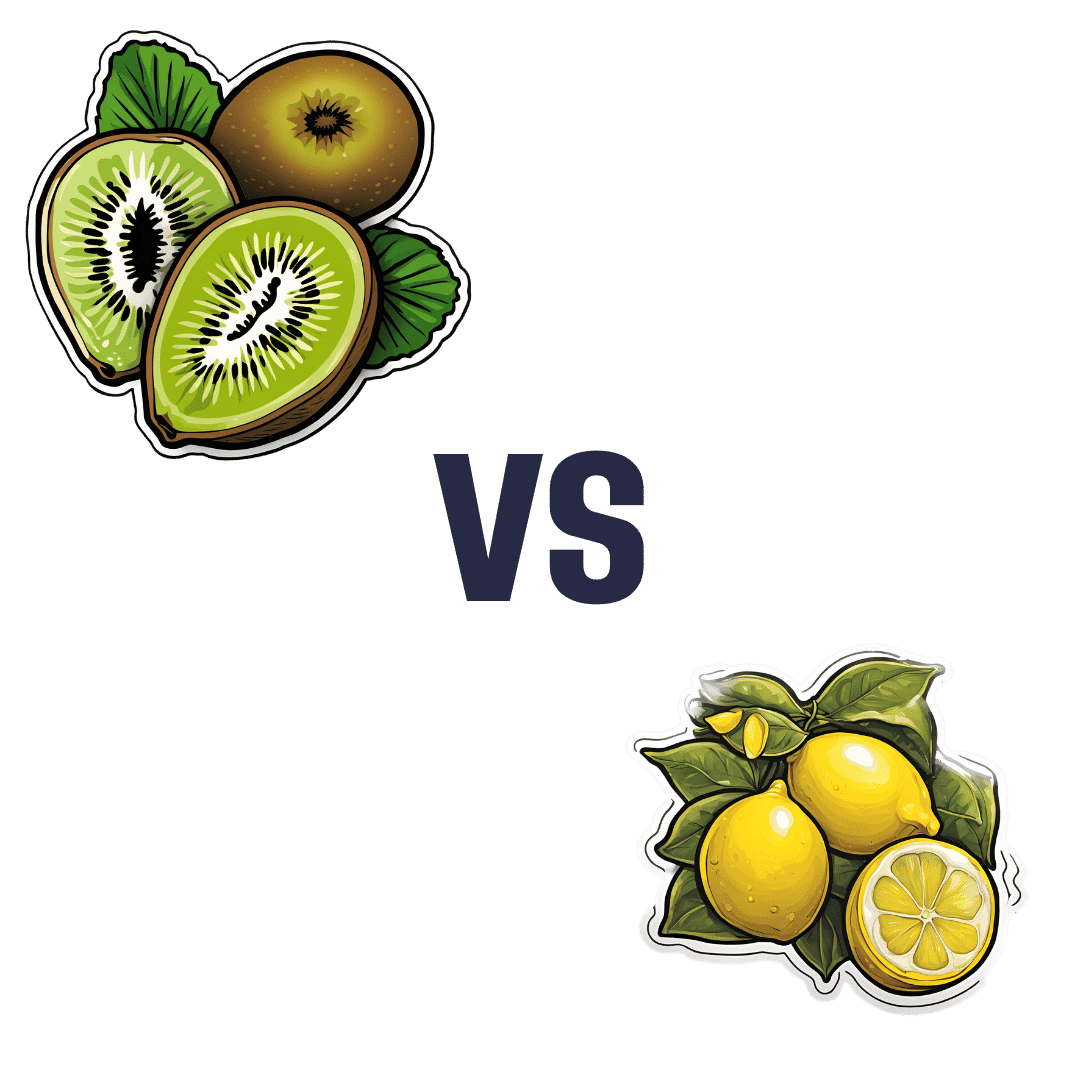
Kiwi vs Lemon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to lemon, we picked the kiwi.
Why?
A fairly straightforward one today!
In terms of macros, kiwi has more protein, carbs, and fiber, the ratio of the latter two also giving it the lower glycemic index. An easy win for kiwi here.
In the category of vitamins, kiwi has more of vitamins A, B2, B3, B9, C, E, K, and choline, while lemon has more of vitamins B1 and B6. Yes, that’s right, lemon didn’t even win on the vitamin C that it’s famous for. In any case, a clear 8:2 win for kiwi.
Looking at minerals, kiwi has more calcium, copper, magnesium, manganese, phosphorus, potassium, and zinc, while lemon has more iron and selenium. So, looking at this 7:2 win for kiwi, you might want to reconsider that “glass of lemon water to replenish minerals” trend!
None of this is to knock lemons, by the way; lemons are still a very respectable fruit, nutritionally. Probably very few people are out there eating lemons the way one might eat kiwi…
(writer’s note: I say “very few”, as once upon a time when my son was small, I remember coming into the kitchen to find he had helped himself to lemon wedges and was just eating them, so it can happen. But I also one time when he was just as small, found him drinking hot sauce directly from the bottle, so hey, he clearly already enjoyed strong flavors. Lest I seem a very inattentive mother, I’ll say in my defense that our kitchen has no real toddler-height hazards when the oven is cold, and those items were from the bottom of the fridge, so easy to access if I leave the room for a moment to grab something)
…but what we do want to say here is: if you don’t care for lemons so much, you’re not missing out. If the lemon water isn’t calling to you, you can skip it guilt-free.
In any case, do enjoy either or both, but kiwi’s the clear winner here!
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← kiwi is top of the list! It has some cool properties, as you’ll see, killing cancer cells while sparing healthy ones.
Take care!
Share This Post
-
What’s Missing from Medicine – by Dr. Saray Stancic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Another from the ranks of “doctors who got a serious illness and it completely changed how they view the treatment of serious illness”, Dr. Stancic was diagnosed with multiple sclerosis, and wasn’t impressed with the treatments presented.
Taking an evidence-based lifestyle medicine approach, she was able to not only manage her illness sufficiently to resume her normal activities, but even when so far as to run a marathon, and today boasts a symptom-free, active life.
The subtitular six lifestyle changes are not too shocking, and include a plants-centric diet, good exercise, good sleep, stress management, avoidance of substance abuses, and a fostering of social connections, but the value here is in what she has to say about each, especially the ones that aren’t so self-explanatory and/or can even cause harm if done incorrectly (such as exercise, for example).
The style is on the academic end of pop-science, of the kind that has frequent data tables, lots of statistics, and an extensive bibliography, but is still very readable.
Bottom line: if you are faced with a chronic disease, or even just an increased risk of some chronic disease, or simply like to not take chances, then this is a high-value book for you.
Click here to check out What’s Missing From Medicine, and enjoy chronic good health!
Share This Post
Related Posts
-
“Skinny Fat” Explained (& How To Fix It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Skinny fat” is a term you may have seen floating around social media. It describes people who have a low body weight but a high body fat percentage, often resulting in flabby appearance despite being within a weight range considered healthy. Many try dieting and exercising, only to find that neither work.
This video explains what’s going wrong, and how to fix it:
Diet & exercise won’t work if it’s not right
This problem occurs because common weight-loss approaches, such as restrictive dieting and excessive cardio, fail to improve body composition:
- Restrictive dieting reduces both fat and lean mass, keeping the body fat percentage unchanged
- Cardio burns some calories but the underlying metabolic issue hasn’t meaningfully changed, so any loss will be temporary (and most of any immediate loss will be water weight, anyway)
The key to overcoming skinny fat is resistance training. Lifting weights or doing bodyweight exercises helps build muscle, which not only lowers body fat percentage (by simple mathematics; add more muscle and the percentages of other things must go down even if the total amount is the same) and improves overall definition, which is something most people consider nice. However, the real value here is that it actually addresses the underlying metabolic issue—because muscle costs calories to maintain, one’s basal metabolic rate will now be faster, even when you’re sleeping.
This then becomes… Not quite a self-sustaining system, because you do have to still eat well and continue to do resistance training, but your body will be doing most of the work for you, and you’ll find it’s a lot easier to maintain a healthy body composition than to get one in the first place, for exactly the metabolic reason we described.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Visceral Belly Fat & How To Lose It ← this is a different, but adjacent issue (and very important for avoiding metabolic disease risks)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kombucha vs Kimchi – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kombucha to kimchi, we picked the kombucha.
Why?
While both are very respectable gut-healthy fermented products,
• the kombucha contains fermented tea, a little apple cider vinegar, and a little fiber
• the kimchi contains (after the vegetables) 810 mg sodium in that little tin, and despite the vegetables, no fiber.You may reasonably be surprised that they managed to take something that is made of mostly vegetables and ended up with no fiber without juicing it, but they did. Fermented vegetables are great for the healthy bacteria benefits (and are tasty too!), but the osmotic pressure due to the salt destroys the cell walls and thus the fiber.
Thus, we chose the kombucha that does the same job without delivering all that salt.
However! If you are comparing kombucha and kimchi out in the wilds of your local supermarket, do still check individual labels. It’s not uncommon, for example, for stores to sell pre-made kombucha that’s loaded with sugar.
About sugar and kombucha…
Sugar is required to make kombucha, to feed the yeast and helpful bacteria. However, there should be none of that sugar left (or only the tiniest trace amount) in the final product, because the yeast (and friends) consumed and metabolized it.
What some store brands do, however, is add in sugar afterwards, as they believe it improves the taste. This writer cannot imagine how, but that is their rationale in any case. Needless to say, it is not a healthy addition, and specifically, it’s bad for your gut, which (healthwise) is the whole point of drinking kombucha in the first place.
Want some? Here is an example product on Amazon, but feel free to shop around as there are many flavors available!
Read more about gut health: Gut Health 101
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Skin Care Down There (Incl. Butt Acne, Hyperpigmentation, & More)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Sam Ellis, dermatologist, gives us the low-down:
Where the sun don’t shine
Common complaints and remedies that Dr. Ellis covers in this video include:
- Butt acne/folliculitis: most butt breakouts are actually folliculitis, not traditional acne. Folliculitis is caused by friction, sitting for long periods, or wearing tight clothes. Solutions include antimicrobial washes like benzoyl peroxide and changing sitting habits (i.e. to sit less)
- Keratosis pilaris: rough bumps around hair follicles can appear on the butt, often confused with acne.
- Boils and abscesses: painful, large lumps; these need medical attention for drainage.
- Hidradenitis suppurativa: recurrent painful cysts and boils in skin creases, often in the groin and buttocks. These require medical intervention and treatment.
- Ingrown hairs: are common in people who shave or wax. Treat with warm compresses and gentle exfoliants.
- Hyperpigmentation: is often caused by hormonal changes, friction, or other irritation. Laser hair removal and gentle chemical exfoliants can help.
In the event that the sun does, in fact, shine on your genitals (for example you sunbathe nude and have little or no pubic hair), then sun protection is essential to prevent further darkening (and also, incidentally, reduce the risk of cancer).
For more on all of this, plus a general introduction to skincare in the bikini zone (i.e. if everything’s fine there right now and you’d like to keep it that way), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Evidence-Based Skincare That Beats Product-Specific Hype
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: