What’s the difference between heat exhaustion and heat stroke? One’s a medical emergency
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When British TV doctor Michael Mosley died last year in Greece after walking in extreme heat, local police said “heat exhaustion” was a contributing factor.
Since than a coroner could not find a definitive cause of death but said this was most likely due to an un-identified medical reason or heat stroke.
Heat exhaustion and heat stroke are two illnesses that relate to heat.
So what’s the difference?

A spectrum of conditions
Heat-related illnesses range from mild to severe. They’re caused by exposure to excessive heat, whether from hot conditions, physical exertion, or both. The most common ones include:
- heat oedema: swelling of the hands, feet and ankles
- heat cramps: painful, involuntary muscle spasms usually after exercise
- heat syncope: fainting due to overheating
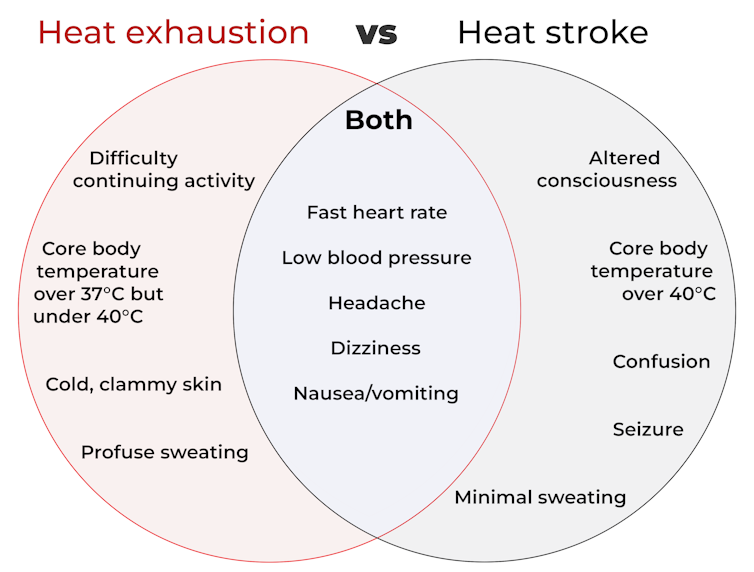
- heat exhaustion: when the body loses water due to excessive sweating, leading to a rise in core body temperature (but still under 40°C). Symptoms include lethargy, weakness and dizziness, but there’s no change to consciousness or mental clarity
- heat stroke: a medical emergency when the core body temperature is over 40°C. This can lead to serious problems related to the nervous system, such as confusion, seizures and unconsciousness including coma, leading to death.
As you can see from the diagram below, some symptoms of heat stroke and heat exhaustion overlap. This makes it hard to recognise the difference, even for medical professionals.
How does this happen?
The human body is an incredibly efficient and adaptable machine, equipped with several in-built mechanisms to keep our core temperature at an optimal 37°C.
But in healthy people, regulation of body temperature begins to break down when it’s hotter than about 31°C with 100% humidity (think Darwin or Cairns) or about 38°C with 60% humidity (typical of other parts of Australia in summer).
This is because humid air makes it harder for sweat to evaporate and take heat with it. Without that cooling effect, the body starts to overheat.
Once the core temperature rises above 37°C, heat exhaustion can set in, which can cause intense thirst, weakness, nausea and dizziness.
If the body heat continues to build and the core body temperature rises above 40°C, a much more severe heat stroke could begin. At this point, it’s a life-threatening emergency requiring immediate medical attention.
At this temperature, our proteins start to denature (like an egg on a hotplate) and blood flow to the intestines stops. This makes the gut very leaky, allowing harmful substances such as endotoxins (toxic substances in some bacteria) and pathogens (disease causing microbes) to leak into the bloodstream.
The liver can’t detoxify these fast enough, leading to the whole body becoming inflamed, organs failing, and in the worst-case scenario, death.
Who’s most at risk?
People doing strenuous exercise, especially if they’re not in great shape, are among those at risk of heat exhaustion or heat stroke. Others at risk include those exposed to high temperatures and humidity, particularly when wearing heavy clothing or protective gear.
Outdoor workers such as farmers, firefighters and construction workers are at higher risk too. Certain health conditions, such as diabetes, heart disease, or lung conditions (such as COPD or chronic obstructive pulmonary disease), and people taking blood pressure medications, can also be more vulnerable.
Adults over 65, infants and young children are especially sensitive to heat as they are less able to physically cope with fluctuations in heat and humidity.

How are these conditions managed?
The risk of serious illness or death from heat-related conditions is very low if treatment starts early.
For heat exhaustion, have the individual lie down in a cool, shady area, loosen or remove excess clothing, and cool them by fanning, moistening their skin, or immersing their hands and feet in cold water.
As people with heat exhaustion almost always are dehydrated and have low electrolytes (certain minerals in the blood), they will usually need to drink fluids.
However, emergency hospital care is essential for heat stroke. In hospital, health professionals will focus on stabilising the patient’s:
- airway (ensure no obstructions, for instance, vomit)
- breathing (look for signs of respiratory distress or oxygen deprivation)
- circulation (check pulse, blood pressure and signs of shock).
Meanwhile, they will use rapid-cooling techniques including immersing the whole body in cold water, or applying wet ice packs covering the whole body.
Take home points
Heat-related illnesses, such as heat stroke and heat exhaustion, are serious health conditions that can lead to severe illness, or even death.
With climate change, heat-related illness will become more common and more severe. So recognising the early signs and responding promptly are crucial to prevent serious complications.
Matthew Barton, Senior lecturer, School of Nursing and Midwifery, Griffith University and Michael Todorovic, Associate Professor of Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is Unnoticed Environmental Mold Harming Your Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Environmental mold can be a lot more than just the famously toxic black mold that sometimes makes the headlines, and many kinds you might not notice, but it can colonizes your sinuses and gut just the same:
Breaking the mold
Around 25% of homes in North America are estimated to have mold, though the actual number is likely to be higher, affecting both older and new homes. For that matter, mold can grow in unexpected areas, like inside air conditioning units, even in dry regions.
If mold just sat where it is minding its own business, it might not be so bad, but instead they release their spores, which are de facto airborne mycotoxins, which can colonize places like the sinuses or gut, causing significant health issues.
Not everyone in the same household is affected the same way by mold due to genetic differences and varying pre-existing health conditions. But as a general rule of thumb, mold inflames the brain, nerves, gut, and skin, and can negatively impact the vagal nerve, which is linked to the gut-brain connection. Mycotoxins also damage mitochondria, leading to symptoms like fatigue, brain fog, and cognitive issues. To complicate matters further, mold illness can mimic other conditions like anxiety, chronic fatigue, fibromyalgia, IBS, and more, making it difficult to diagnose.
Testing is possible, though they all have limitations, e.g:
- Home testing: testing the home for mold spores and mycotoxins is crucial for effective treatment; professional mold remediation companies are a good idea (to do a thorough job of cleaning, without also breathing in half the mold while cleaning it).
- Mold allergy testing: mold allergy testing (IgE testing or skin tests) is often used, but it doesn’t diagnose mold-related illnesses linked to severe symptoms like fatigue or neurodegeneration.
- Serum antibody testing: tests for immune reactions (IgG) to mycotoxins may not always show positive results if the immune system is weakened by long-term exposure.
- Urine mycotoxin testing: urine tests can detect mycotoxins in the body, though are likely to be more expensive, being probably not covered by public health in Canada or insurance in the US.
- Organic acid testing: this urine test can indicate mold colonization in areas like the sinuses or gut. Again, cost/availability may vary, though.
For more information on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
What is PNF stretching, and will it improve my flexibility?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether improving your flexibility was one of your new year’s resolutions, or you’ve been inspired watching certain tennis stars warming up at the Australian Open, maybe 2025 has you keen to focus on regular stretching.
However, a quick Google search might leave you overwhelmed by all the different stretching techniques. There’s static stretching and dynamic stretching, which can be regarded as the main types of stretching.
But there are also some other potentially lesser known types of stretching, such as PNF stretching. So if you’ve come across PNF stretching and it piques your interest, what do you need to know?
Undrey/Shutterstock What is PNF stretching?
PNF stretching stands for proprioceptive neuromuscular facilitation. It was developed in the 1940s in the United States by neurologist Herman Kabat and physical therapists Margaret Knott and Dorothy Voss.
PNF stretching was initially designed to help patients with neurological conditions that affect the movement of muscles, such as polio and multiple sclerosis.
By the 1970s, its popularity had seen PNF stretching expand beyond the clinic and into the sporting arena where it was used by athletes and fitness enthusiasts during their warm-up and to improve their flexibility.
Although the specifics have evolved over time, PNF essentially combines static stretching (where a muscle is held in a lengthened position for a short period of time) with isometric muscle contractions (where the muscle produces force without changing length).
PNF stretching is typically performed with the help of a partner.
There are 2 main types
The two most common types of PNF stretching are the “contract-relax” and “contract-relax-agonist-contract” methods.
The contract-relax method involves putting a muscle into a stretched position, followed immediately by an isometric contraction of the same muscle. When the person stops contracting, the muscle is then moved into a deeper stretch before the process is repeated.
For example, to improve your hamstring flexibility, you could lie down and get a partner to lift your leg up just to the point where you begin to feel a stretch in the back of your thigh.
Once this sensation eases, attempt to push your leg back towards the ground as your partner resists the movement. After this, your partner should now be able to lift your leg up slightly higher than before until you feel the same stretching sensation.
This technique was based on the premise that the contracted muscle would fall “electrically silent” following the isometric contraction and therefore not offer its usual level of resistance to further stretching (called “autogenic inhibition”). The contract-relax method attempts to exploit this brief window to create a deeper stretch than would otherwise be possible without the prior muscle contraction.
The contract-relax-agonist-contract method is similar. But after the isometric contraction of the stretched muscle, you perform an additional contraction of the muscle group opposing the muscle being stretched (referred to as the “agonist” muscle), before the muscle is moved into a static stretch once more.
Again, if you’re trying to improve hamstring flexibility, immediately after trying to push your leg towards the ground you would attempt to lift it back towards the ceiling (this bit without partner resistance). You would do this by contracting the muscles on the front of the thigh (the quadriceps, the agonist muscle in this case).
Likewise, after this, your partner should be able to lift your leg up slightly higher than before.
The contract-relax-agonist-contract method is said to take advantage of a phenomenon known as “reciprocal inhibition.” This is where contracting the muscle group opposite that of the muscle being stretched leads to a short period of reduced activation of the stretched muscle, allowing the muscle to stretch further than normal.
What does the evidence say?
Research has shown PNF stretching is associated with improved flexibility.
While it has been suggested that both PNF methods improve flexibility via changes in nervous system function, research suggests they may simply improve our ability to tolerate stretching.
It’s worth noting most of the research on PNF stretching and flexibility has focused on healthy populations. This makes it difficult to provide evidence-based recommendations for people with clinical conditions.
And it may not be the most effective method if you’re looking to improve your flexibility in the long term. A 2018 review found static stretching was better for improving flexibility compared to PNF stretching. But other research has found it could offer greater immediate benefits for flexibility than static stretching.
At present, similar to other types of stretching, research linking PNF stretching to injury prevention and improved athletic performance is relatively inconclusive.
PNF stretching may actually lead to small temporary deficits in performance of strength, power, and speed-based activities if performed immediately beforehand. So it’s probably best done after exercise or as a part of a standalone flexibility session.
Static stretching may be a more effective way to improve flexibility over the long-term. GaudiLab/Shutterstock How much should you do?
It appears that a single contract-relax or contract-relax-agonist-contract repetition per muscle, performed twice per week, is enough to improve flexibility.
The contraction itself doesn’t need to be hard and forceful – only about 20% of your maximal effort should suffice. The contraction should be held for at least three seconds, while the static stretching component should be maintained until the stretching sensation eases.
So PNF stretching is potentially a more time-efficient way to improve flexibility, compared to, for example, static stretching. In a recent study we found four minutes of static stretching per muscle during a single session is optimal for an immediate improvement in flexibility.
Is PNF stretching the right choice for me?
Providing you have a partner who can help you, PNF stretching could be a good option. It might also provide a faster way to become more flexible for those who are time poor.
However, if you’re about to perform any activities that require strength, power, or speed, it may be wise to limit PNF stretching to afterwards to avoid any potential deficits in performance.
Lewis Ingram, Lecturer in Physiotherapy, University of South Australia and Hunter Bennett, Lecturer in Exercise Science, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Maximize Your Misery! (7 Great Methods)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s imagine that instead of being healthily fulfilled in life, you wanted to spend your days as miserable as possible. What should you do?
Here are a few pointers:
Stay still
Avoid physical activity and/or outdoor exposure, to avoid any mood-lifting neurochemicals. In fact, remain indoors as much as possible, preferably in the same room.
If you want to absolutely maximize your misery, make your bedroom the sole space for all activities that it’s possible to do there.
Disrupt your sleep
Keep an irregular sleep schedule by varying your bedtime and wake-up times frequently. Sleep in as much as possible, and make up for it by staying up late to ensure ongoing exhaustion.
Maximize screentime
Use digital entertainment as much as possible to distract you from meaningful activities and rest—as a bonus, this will also help you to avoid self-reflection.
Begin and end your day with a device in hand.
Fuel negative emotions
If you’re going to focus on something, focus on problems you cannot control, to stoke the fires of anger and angst.
A good way of doing this is by staying informed about distressing events, while avoiding meaningful actions to address them. Contribute only in token gestures, and then lament the lack of change.
Follow your impulses
Act on short-term desires without considering long-term consequences, while avoiding behaviors that you know might improve your mood or wellbeing.
Trust that doing the same things that have not previously resulted in happiness, will continue to reliably deliver unhappiness.
Set goals to miss
It’s important that your goals should be vague, and overly ambitious in their scope and/or deliverability. Ideally you should also disregard any preparatory work that a person would normally do before embarking on such a project.
Bonus tip: you can further sabotage any chances of progress, by waiting for motivation to strike before you take any action.
Pursue happiness
Focus on chasing happiness itself, instead of improving your situation or skills. Treat happiness as an end goal, instead of a by-product of worthwhile activities.
Want to learn more?
If you’d like to know many more ways to be miserable, we featured these 7 from this book of 40, which we haven’t reviewed yet, but probably will one of these days:
How to Be Miserable: 40 Strategies You Already Use – by Dr. Randy Paterson
Alternatively…
If for some strange reason you’d rather not do those things, you might consider a previous article of ours:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Enjoy!
Share This Post
Related Posts
-
How Stress Affects Your Body
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Sharon Bergquist gives us a tour:
Stress, from the inside out
Stress is a natural physical and emotional response to challenges or being overwhelmed. It can be beneficial in short-term situations (e.g. escape from a tiger) but is harmful when prolonged or frequent (e.g. escape the rat-race).
Immediate physiological response: cortisol, adrenaline (epinephrine), and norepinephrine are released by the adrenal glands.
The effects this has (non-exhaustive list; we’re just citing what’s in the video here):
- Cortisol impairs blood vessel function, promoting atherosclerosis.
- Adrenaline increases heart rate and blood pressure, leading to hypertension.
- Stress disrupts the brain-gut connection, causing:
- Digestive issues like irritable bowel syndrome and heartburn.
- Changes in gut bacteria composition, potentially affecting overall health.
- Cortisol increases appetite and cravings for energy-dense “comfort foods”.
- This in turn promotes visceral fat storage, which raises the risk of heart disease and insulin resistance.
- Immune-specific effects:
- Stress hormones initially aid in healing and immune defense.
- Chronic stress weakens immune function (by over-working it constantly), increasing susceptibility to infections and slowing recovery.
- Other systemic effects:
- Chronic stress shortens telomeres, which protect chromosomes. Shortened telomeres accelerate cellular aging.
- Chronic stress can also cause acne, hair loss, sexual dysfunction, headaches, muscle tension, fatigue, irritability, and difficulty concentrating.
So, how to manage this? The video says that viewing stressful situations as controllable challenges, rather than insurmountable threats, leads to better short-term performance and long-term health.
Which would be wonderful, except that usually things are stressful precisely because they are not entirely within the field of our control, and the usual advice is to tend to what we can control, and accept what we can’t.
However… That paradigm still leaves out the very big set of “this might be somewhat within our control or it might not; we really don’t know yet; we can probably impact it but what if we don’t do enough, or take the wrong approach and do the wrong thing? And also we have 17 competing stressors, which ones should we prioritize tending to first, and…” and so on.
To that end, we suggest checking out the “Want to learn more?” link we drop below the video today, as it is about managing stress realistically, in a world that, if we’re honest about it, can sometimes be frankly unmanageable.
Meanwhile, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Heart Health vs Systemic Stress ← this is good in and of itself, and also links to other stress-related resources of ours
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Psychoactive Drugs Are Having a Moment. The FDA Will Soon Weigh In.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lori Tipton is among the growing number of people who say that MDMA, also known as ecstasy, saved their lives.
Raised in New Orleans by a mother with untreated bipolar disorder who later killed herself and two others, Tipton said she endured layers of trauma that eventually forced her to seek treatment for crippling anxiety and hypervigilance. For 10 years nothing helped, and she began to wonder if she was “unfixable.”
Then she answered an ad for a clinical trial for MDMA-assisted therapy to treat post-traumatic stress disorder. Tipton said the results were immediate, and she is convinced the drug could help a lot of people. But even as regulators weigh approval of the first MDMA-based treatment, she’s worried that it won’t reach those who need it most.
“The main thing that I’m always concerned about is just accessibility,” the 43-year-old nonprofit project manager said. “I don’t want to see this become just another expensive add-on therapy for people who can afford it when people are dying every day by their own hand because of PTSD.”
MDMA is part of a new wave of psychoactive drugs that show great potential for treating conditions such as severe depression and PTSD. Investors are piling into the nascent field, and a host of medications based on MDMA, LSD, psychedelic mushrooms, ketamine, the South American plant mixture ayahuasca, and the African plant ibogaine are now under development, and in some cases vying for approval by the Food and Drug Administration.
Proponents hope the efforts could yield the first major new therapies for mental illness since the introduction of modern antidepressants in the 1980s. But not all researchers are convinced that their benefits have been validated, or properly weighed against the risks. And they can be difficult to assess using traditional clinical trials.
The first MDMA-assisted assisted therapy appeared to be on track for FDA approval this August, but a recent report from an independent review committee challenged the integrity of the trial data from the drug’s maker, Lykos Therapeutics, a startup founded by a psychedelic research and advocacy group. The FDA will convene a panel of independent investigators on June 4 to determine whether to recommend the drug’s approval.
Proponents of the new therapies also worry that the FDA will impose treatment protocols, such as requiring multiple trained clinicians to monitor a patient for extended periods, that will render them far too expensive for most people.
Tipton’s MDMA-assisted therapy included three eight-hour medication sessions overseen by two therapists, each followed by an overnight stay at the facility and an integration session the following day.
“It does seem that some of these molecules can be administered safely,” said David Olson, director of the University of California-Davis Institute for Psychedelics and Neurotherapeutics. “I think the question is can they be administered safely at the scale needed to really make major improvements in mental health care.”
Breakthrough Therapies?
Psychedelics and other psychoactive substances, among the medicines with the oldest recorded use, have long been recognized for their potential therapeutic benefits. Modern research on them started in the mid-20th century, but clinical trial results didn’t live up to the claims of advocates, and they eventually got a bad name both from their use as party drugs and from rogue CIA experiments that involved dosing unsuspecting individuals.
The 1970 Controlled Substances Act made most psychoactive drugs illegal before any treatments were brought to market, and MDMA was classified as a Schedule 1 substance in 1985, which effectively ended any research. It wasn’t until 2000 that scientists at Johns Hopkins University were granted regulatory approval to study psilocybin anew.
Ketamine was in a different category, having been approved as an anesthetic in 1970. In the early 2000s, researchers discovered its antidepressant effects, and a ketamine-based therapy, Spravato, received FDA approval in 2019. Doctors can also prescribe generic ketamine off-label, and hundreds of clinics have sprung up across the nation. A clinical trial is underway to evaluate ketamine’s effectiveness in treating suicidal depression when used with other psychiatric medications.
Ketamine’s apparent effectiveness sparked renewed interest in the therapeutic potential of other psychoactive substances.
They fall into distinct categories: MDMA is an entactogen, also known as an empathogen, which induces a sense of connectedness and emotional communion, while LSD, psylocibin, and ibogaine are psychedelics, which create altered perceptual states. Ketamine is a dissociative anesthetic, though it can produce hallucinations at the right dose.
Despite the drugs’ differences, Olson said they all create neuroplasticity and allow the brain to heal damaged neural circuits, which imaging shows can be shriveled up in patients with addiction, depression, and PTSD.
“All of these brain conditions are really disorders of neural circuits,” Olson said. “We’re basically looking for medicines that can regrow these neurons.”
Psychedelics are particularly good at doing this, he said, and hold promise for treating diseases including Alzheimer’s.
A number of psychoactive drugs have now received the FDA’s “breakthrough therapy” designation, which expedites development and review of drugs with the potential to treat serious conditions.
But standard clinical trials, in which one group of patients is given the drug and a control group is given a placebo, have proven problematic, for the simple reason that people have no trouble determining whether they’ve gotten the real thing.
The final clinical trial for Lykos’ MDMA treatment showed that 71% of participants no longer met the criteria for PTSD after 18 weeks of taking the drug versus 48% in the control group.
A March report by the Institute for Clinical and Economic Review, an independent research group, questioned the company’s clinical trial results and challenged the objectivity of MDMA advocates who participated in the study as both patients and therapists. The institute also questioned the drug’s cost-effectiveness, which insurers factor into coverage decisions.
Lykos, a public benefit company, was formed in 2014 as an offshoot of the Multidisciplinary Association for Psychedelic Studies, a nonprofit that has invested more than $150 million into psychedelic research and advocacy.
The company said its researchers developed their studies in partnership with the FDA and used independent raters to ensure the reliability and validity of the results.
“We stand behind the design and results of our clinical trials,” a Lykos spokesperson said in an email.
There are other hazards too. Psychoactive substances can put patients in vulnerable states, making them potential victims for financial exploitation or other types of abuse. In Lykos’ second clinical trial, two therapists were found to have spooned, cuddled, blindfolded, and pinned down a female patient who was in distress.
The substances can also cause shallow breathing, heart issues, and hyperthermia.
To mitigate risks, the FDA can put restrictions on how drugs are administered.
“These are incredibly potent molecules and having them available in vending machines is probably a bad idea,” said Hayim Raclaw of Negev Capital, a venture capital fund focused on psychedelic drug development.
But if the protocols are too stringent, access is likely to be limited.
Rachel del Dosso, a trauma therapist in the greater Los Angeles area who offers ketamine-assisted therapy, said she’s been following the research on drugs like MDMA and psilocybin and is excited for their therapeutic potential but has reservations about the practicalities of treatment.
“As a therapist in clinical practice, I’ve been thinking through how could I make that accessible,” she said. “Because it would cost a lot for [patients] to have me with them for the whole thing.”
Del Dosso said a group therapy model, which is sometimes used in ketamine therapy, could help scale the adoption of other psychoactive treatments, too.
Artificial Intelligence and Analogs
Researchers expect plenty of new discoveries in the field. One of the companies Negev has invested in, Mindstate Design Labs, uses artificial intelligence to analyze “trip reports,” or self-reported drug experiences, to identify potentially therapeutic molecules. Mindstate has asked the FDA to green-light a clinical trial of the first molecule identified through this method, 5-MeO-MiPT, also known as moxy.
AlphaFold, an AI program developed by Google’s DeepMind, has identified thousands of potential psychedelic molecules.
There’s also a lot of work going into so-called analog compounds, which have the therapeutic effects of hallucinogens but without the hallucinations. The maker of a psilocybin analog announced in March that the FDA had granted it breakthrough therapy status.
“If you can harness the neuroplasticity-promoting properties of LSD while also creating an antipsychotic version of it, then that can be pretty powerful,” Olson said.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The How Not to Die Cookbook – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Greger’s “How Not To Die”, which is excellent and/but very science-dense.
This book is different, in that the science is referenced and explained throughout, but the focus is the recipes, and how to prepare delicious healthy food in accordance with the principles laid out in How Not To Die.
It also follows “Dr Greger’s Daily Dozen“, that is to say, the 12 specific things he advises we make sure to have every day, and thus helps us to include them in an easy, no-fuss fashion.
The recipes themselves are by Robin Robertson, and/but with plenty of notes by Dr Greger; they clearly collaborated closely in creating them.
The ingredients are all things one can find in any well-stocked supermarket, so unless you live in a food desert, you can make these things easily.
And yes, the foods are delicious too.
Bottom line: if you’re interested in cooking according to perhaps the most science-based dietary system out there, then this book is a top-tier choice.
Click here to check out The How Not To Die Cookbook, and live well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: