What is type 1.5 diabetes? It’s a bit like type 1 and a bit like type 2 – but it’s often misdiagnosed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While you’re likely familiar with type 1 and type 2 diabetes, you’ve probably heard less about type 1.5 diabetes.
Also known as latent autoimmune diabetes in adults (LADA), type 1.5 diabetes has features of both type 1 and type 2 diabetes.
More people became aware of this condition after Lance Bass, best known for his role in the iconic American pop band NSYNC, recently revealed he has it.
So, what is type 1.5 diabetes? And how is it diagnosed and treated?

There are several types of diabetes
Diabetes mellitus is a group of conditions that arise when the levels of glucose (sugar) in our blood are higher than normal. There are actually more than ten types of diabetes, but the most common are type 1 and type 2.
Type 1 diabetes is an autoimmune condition where the body’s immune system attacks and destroys the cells in the pancreas that make the hormone insulin. This leads to very little or no insulin production.
Insulin is important for moving glucose from the blood into our cells to be used for energy, which is why people with type 1 diabetes need insulin medication daily. Type 1 diabetes usually appears in children or young adults.
Type 2 diabetes is not an autoimmune condition. Rather, it happens when the body’s cells become resistant to insulin over time, and the pancreas is no longer able to make enough insulin to overcome this resistance. Unlike type 1 diabetes, people with type 2 diabetes still produce some insulin.
Type 2 is more common in adults but is increasingly seen in children and young people. Management can include behavioural changes such as nutrition and physical activity, as well as oral medications and insulin therapy.

How does type 1.5 diabetes differ from types 1 and 2?
Like type 1 diabetes, type 1.5 occurs when the immune system attacks the pancreas cells that make insulin. But people with type 1.5 often don’t need insulin immediately because their condition develops more slowly. Most people with type 1.5 diabetes will need to use insulin within five years of diagnosis, while those with type 1 typically require it from diagnosis.
Type 1.5 diabetes is usually diagnosed in people over 30, likely due to the slow progressing nature of the condition. This is older than the typical age for type 1 diabetes but younger than the usual diagnosis age for type 2.
Type 1.5 diabetes shares genetic and autoimmune risk factors with type 1 diabetes such as specific gene variants. However, evidence has also shown it may be influenced by lifestyle factors such as obesity and physical inactivity which are more commonly associated with type 2 diabetes.
What are the symptoms, and how is it treated?
The symptoms of type 1.5 diabetes are highly variable between people. Some have no symptoms at all. But generally, people may experience the following symptoms:
- increased thirst
- frequent urination
- fatigue
- blurred vision
- unintentional weight loss.
Typically, type 1.5 diabetes is initially treated with oral medications to keep blood glucose levels in normal range. Depending on their glucose control and the medication they are using, people with type 1.5 diabetes may need to monitor their blood glucose levels regularly throughout the day.
When average blood glucose levels increase beyond normal range even with oral medications, treatment may progress to insulin. However, there are no universally accepted management or treatment strategies for type 1.5 diabetes.

Type 1.5 diabetes is often misdiagnosed
Lance Bass said he was initially diagnosed with type 2 diabetes, but later learned he actually has type 1.5 diabetes. This is not entirely uncommon. Estimates suggest type 1.5 diabetes is misdiagnosed as type 2 diabetes 5–10% of the time.
There are a few possible reasons for this.
First, accurately diagnosing type 1.5 diabetes, and distinguishing it from other types of diabetes, requires special antibody tests (a type of blood test) to detect autoimmune markers. Not all health-care professionals necessarily order these tests routinely, either due to cost concerns or because they may not consider them.
Second, type 1.5 diabetes is commonly found in adults, so doctors might wrongly assume a person has developed type 2 diabetes, which is more common in this age group (whereas type 1 diabetes usually affects children and young adults).
Third, people with type 1.5 diabetes often initially make enough insulin in the body to manage their blood glucose levels without needing to start insulin medication. This can make their condition appear like type 2 diabetes, where people also produce some insulin.
Finally, because type 1.5 diabetes has symptoms that are similar to type 2 diabetes, it may initially be treated as type 2.
We’re still learning about type 1.5
Compared with type 1 and type 2 diabetes, there has been much less research on how common type 1.5 diabetes is, especially in non-European populations. In 2023, it was estimated type 1.5 diabetes represented 8.9% of all diabetes cases, which is similar to type 1. However, we need more research to get accurate numbers.
Overall, there has been a limited awareness of type 1.5 diabetes and unclear diagnostic criteria which have slowed down our understanding of this condition.
A misdiagnosis can be stressful and confusing. For people with type 1.5 diabetes, being misdiagnosed with type 2 diabetes might mean they don’t get the insulin they need in a timely manner. This can lead to worsening health and a greater likelihood of complications down the road.
Getting the right diagnosis helps people receive the most appropriate treatment, save money, and reduce diabetes distress. If you’re experiencing symptoms you think may indicate diabetes, or feel unsure about a diagnosis you’ve already received, monitor your symptoms and chat with your doctor.
Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University and Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
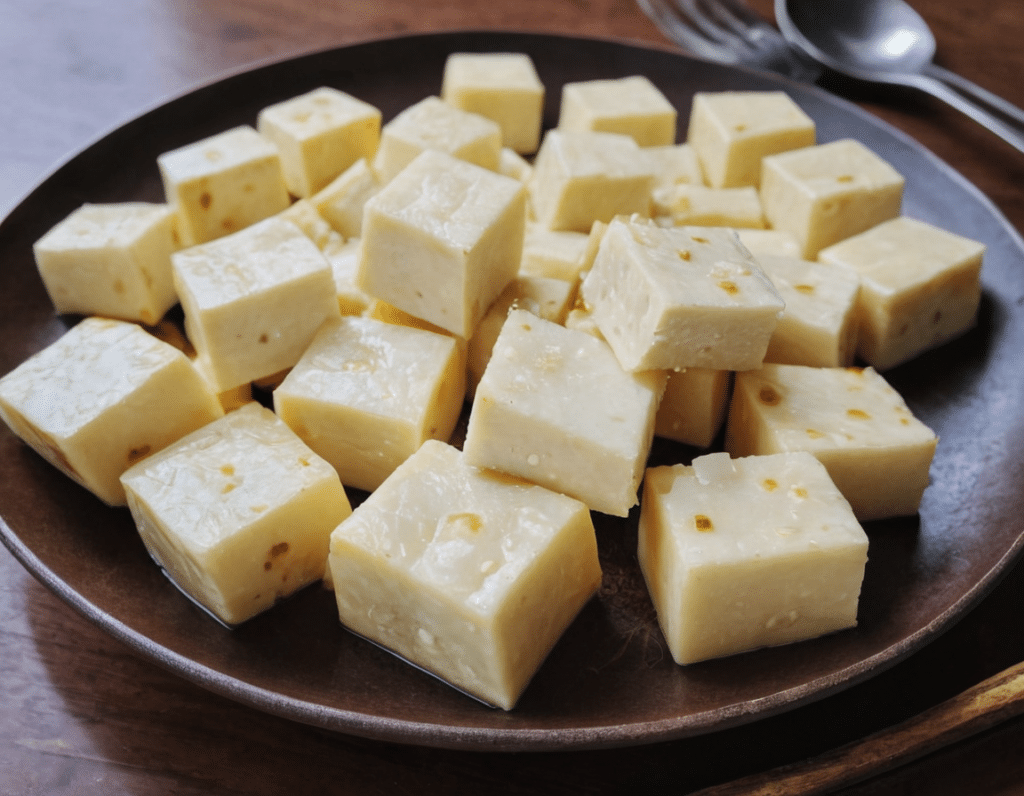
High-Protein Paneer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Paneer (a kind of Desi cheese used in many recipes from that region) is traditionally very high in fat, mostly saturated. Which is delicious, but not exactly the most healthy.
Today we’ll be making a plant-based paneer that does exactly the same jobs (has a similar texture and gentle flavor, takes on the flavors of dishes in the same way, etc) but with a fraction of the fat (of which only a trace amount is saturated, in this plant-based version), and even more protein. We’ll use this paneer in some recipes in the future, but it can be enjoyed by itself already, so let’s get going…
You will need
- ½ cup gram flour (unwhitened chickpea flour)
- Optional: 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Whisk the flour (and salt, if using) with 2 cups water in a big bowl, whisking until the texture is smooth.
2) Transfer to a large saucepan on a low-to-medium heat; you want it hot, but not quite a simmer. Keep whisking until the mixture becomes thick like polenta. This should take 10–15 minutes, so consider having someone else to take shifts if the idea of whisking continually for that long isn’t reasonable to you.
3) Transfer to a non-stick baking tin that will allow you to pour it about ½” deep. If the tin’s too large, you can always use a spatula to push it up against two or three sides, so that it’s the right depth
3) Refrigerate for at least 10 minutes, but longer is better if you have the time.
4) When ready to serve/use, cut it into ½” cubes. These can be served/used now, or kept for about a week in the fridge.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Share This Post
-
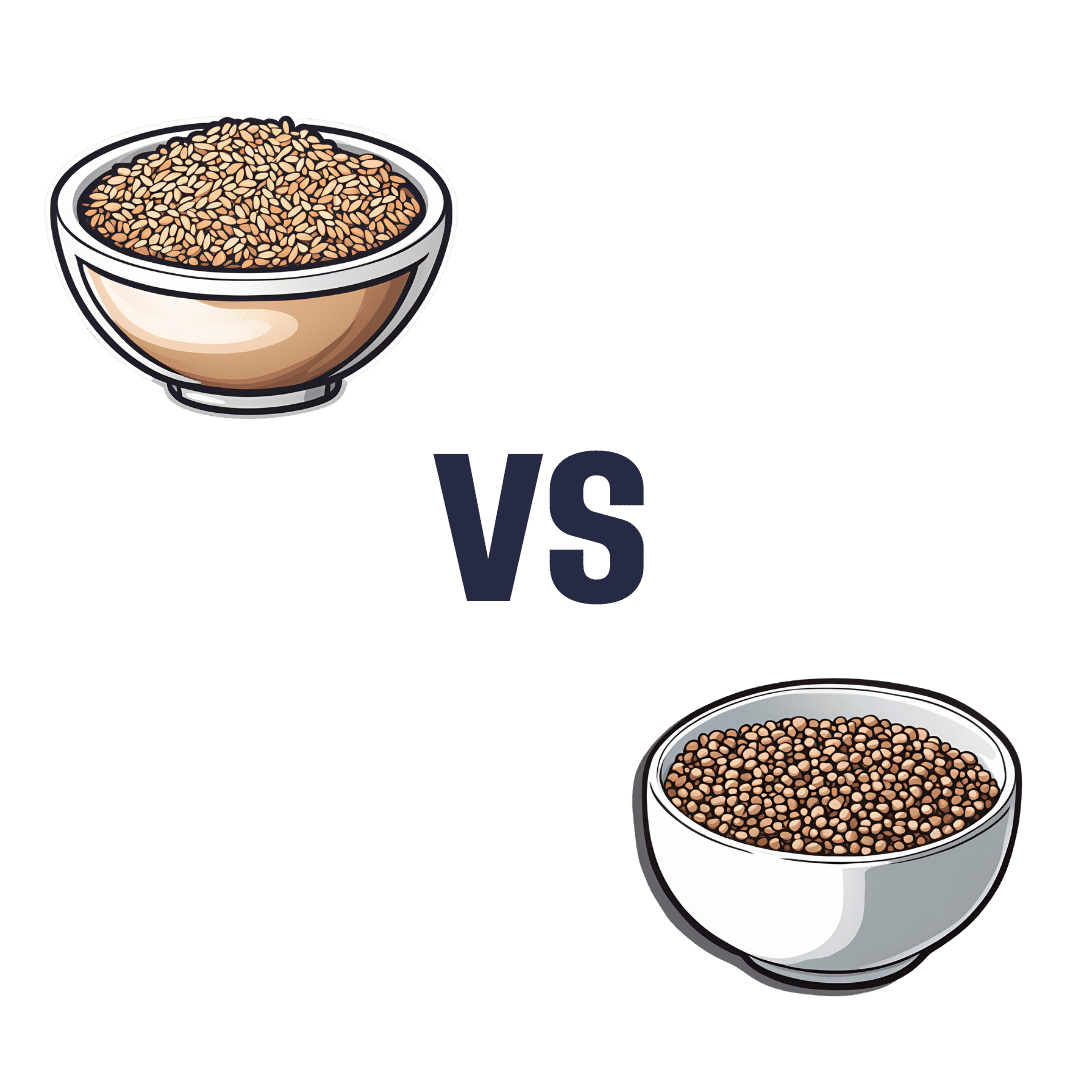
Brown Rice vs Buckwheat – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing brown rice to buckwheat, we picked the buckwheat.
Why?
In terms of macros, brown rice has more carbs, while buckwheat has nearly 2x the fiber, and more protein. An easy choice here: buckwheat for the win.
In the category of vitamins, brown rice has more of vitamins B1, B2, B3, B6, and E, while buckwheat has more of vitamins B9, K, and choline. A win for brown rice this time, although as a point in buckwheat’s favor, while most of the margins of difference are comparable, buckwheat has nearly 10x the vitamin K.
When it comes to minerals, brown rice has more manganese, phosphorus, selenium, and zinc, while buckwheat has more calcium, copper, iron, and magnesium. A win for buckwheat again this time.
A quick note on gluten: both of these are naturally gluten-free, so that’s not an issue here. Buckwheat, despite its name, is not a wheat, nor even closely related to wheat. It’s not even technically a grain; it’s a flowering plant of which we eat the groats. In taxonomic terms, buckwheat is about as related to wheat as a lionfish is to a lion.
Adding up the sections makes for an overall 2:1 win for buckwheat, though even if it weren’t for that, which is someone more likely to hear from a doctor, “you need to eat more fiber”, or “you need to eat more vitamin E”? Thus, even had the categories been tied (let’s imagine it had been tied on minerals, say) that’d have been a tiebreaker in favor of buckwheat. As it is, buckwheat already won by strength of numbers anyway.
Of course, do enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Grains: Bread Of Life, Or Cereal Killer?
Enjoy!
Share This Post
-
Keep Your Wits About You – by Dr. Vonetta Dotson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Dotson sets out to provide the reader with the tools to maintain good brain health at any age, though she does assume the reader to be in midlife or older.
She talks us through the most important kinds of physical activity, mental activity, and social activity, as well as a good grounding in brain-healthy nutrition, and how to beat the often catch-22 situation of poor sleep.
If you are the sort of person who likes refreshers on what you have just read, you’ll enjoy that the final two chapters repeat the information from chapters 2–6. If not, then well, if you skip the final 2 chapters the book will be 25% shorter without loss of content.
The style is enthusiastic; when it comes to her passion for the brain, Dr. Dotson both tells and shows, in abundance. While some authors may take care to break down the information in a way that can be understood from skimming alone, Dr. Dotson assumes that the reader’s interest will match hers, and thus will not mind a lot of lengthy prose with in-line citations. So, provided that’s the way you like to read, it’ll suit you too.
Bottom line: if you are looking for a book on maintaining optimal brain health that covers the basics without adding advice that is out of the norm, then this is a fine option for that!
Click here to check out Keep Your Wits About You, and keep your wits about you!
Share This Post
Related Posts
-
Ready… Set… Flow!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Time to make your new year plans? Or maybe you’ve already made a list, and you’re checking it twice. If so, now’s the time to make sure that your new year’s plans will flow:
“Flow”, as you may be aware, is the psychological state generally defined as “a state in which we feel good about what we’re doing, and just keep doing it, at a peak performance level”; the term was coined by psychologist Mihaly Csikszentmihalyi and has risen to popularity since.
We wrote about it a little before, here:
Morning Routines That Just Flow
The above article details how to start the perfect day, but how to start the perfect year? Firstly, it’s good to get the jump on the new year a little; see:
The Science Of New Year’s Pre-Resolutions
…and we also agree with Dr. Faye Bate, who preaches taking the path of least resistance when it comes to healthy habits:
How To Actually Start A Healthy Lifestyle In The New Year
Because…
Getting into the flow
The most hydrating drink is the one that [contains adequate water and] you will actually drink. The best exercise is the one you’ll do. The best sleep is the sleep you can actually get. And so on.
We see this—or rather its evil counterpoint—a lot in diet culture. People frame their willpower against the temptations of donuts and whatever, and make Faustian bargains whereby they will eat food they find boring in the hopes it will bring them good health. And it won’t. Because, they’ll give up quickly.
Instead, each part of our healthy life has to be engaged with with a sense of flow. Again, that’s: “a state in which we feel good about what we’re doing, and just keep doing it, at a peak performance level”
So we need to find healthy recipes we like (check out our recipe section!), we need to find exercise that we like, we need to find an approach to sleep that the Geneva Convention wouldn’t consider a kind a torture, and so forth. And, ideally, not just “like” in the sense of “this is tolerable” but “like” in the sense of “I am truly passionate about this thing”.
And that’s going to look different for each of us.
Running is a great example of something that some people truly love, whereas others will do almost anything to avoid.
And food? We’ve written before about the usefulness of a “to don’t” list; it’s like a “to do” list, but it’s things we’re not going to even try to do. For example, a person with two addictions is usually advised to quit one at a time, so quitting the other would go on a “to don’t” list for now. The same goes for food; you need to enjoy what you’re eating or you won’t “feel good about what we’re doing, and just keep doing it”, per flow. So, do not deprive yourself; it won’t work anyway; just pick one healthy change to make, and then queue up any other changes for once the first one has started feeling natural to you.
For more on “to don’t” lists and other such tricks, see: How To Keep On Keeping On… Long Term!
Staying in the flow
…is not usually a problem, you would think, because “…and just keep doing it, at peak performance level” but the fact is, sometimes we get kicked out of our flow by something external. We covered some of that in the above-linked “How To Keep On Keeping On” article, such as figuring out showstoppers in advance (for example, “if I get an injury, I will rest until it is healed”) and ideally, back-up plans.
For example, let’s say you have your dietary plan all worked out, then you are invited to someone’s birthday celebration a couple of weeks in, and you don’t want to rain on their parade, so you figure out for yourself in advance how you are going to mitigate any harm to your plans, e.g. “I will simply choose the healthiest option available, and not worry if it doesn’t meet my usual standards” or “I will simply fast” if that’s an appropriate thing for you (for some it might be, for some it might not be).
For more on this, see:
How To Avoid Slipping Into (Bad) Old Habits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Mental Health First-Aid That You’ll Hopefully Never Need
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Take Your Mental Health As Seriously As General Health!
Sometimes, health and productivity means excelling—sometimes, it means avoiding illness and unproductivity. Both are essential, and today we’re going to tackle some ground-up stuff. If you don’t need it right now, great; we suggest to read it for when and if you do. But how likely is it that you will?
- One in four of us are affected by serious mental health issues in any given year.
- One in five of us have suicidal thoughts at some point in our lifetime.
- One in six of us are affected to at least some extent by the most commonly-reported mental health issues, anxiety and depression, in any given week.
…and that’s just what’s reported, of course. These stats are from a UK-based source but can be considered indicative generally. Jokes aside, the UK is not a special case and is not measurably worse for people’s mental health than, say, the US or Canada.
While this is not an inherently cheery topic, we think it’s an important one.
Depression, which we’re going to focus on today, is very very much a killer to both health and productivity, after all.
One of the most commonly-used measures of depression is known by the snappy name of “PHQ9”. It stands for “Patient Health Questionnaire Nine”, and you can take it anonymously online for free (without signing up for anything; it’s right there on the page already):
Take The PHQ9 Test Here! (under 2 minutes, immediate results)
There’s a chance you took that test and your score was, well, depressing. There’s also a chance you’re doing just peachy, or maybe somewhere in between. PHQ9 scores can fluctuate over time (because they focus on the past two weeks, and also rely on self-reports in the moment), so you might want to bookmark it to test again periodically. It can be interesting to track over time.
In the event that you’re struggling (or: in case one day you find yourself struggling, or want to be able to support a loved one who is struggling), some top tips that are useful:
Accept that it’s a medical condition like any other
Which means some important things:
- You/they are not lazy or otherwise being a bad person by being depressed
- You/they will probably get better at some point, especially if help is available
- You/they cannot, however, “just snap out of it”; illness doesn’t work that way
- Medication might help (it also might not)
Do what you can, how you can, when you can
Everyone knows the advice to exercise as a remedy for depression, and indeed, exercise helps many. Unfortunately, it’s not always that easy.
Did you ever see the 80s kids’ movie “The Neverending Story”? There’s a scene in which the young hero Atreyu must traverse the “Swamp of Sadness”, and while he has a magical talisman that protects him, his beloved horse Artax is not so lucky; he slows down, and eventually stops still, sinking slowly into the swamp. Atreyu pulls at him and begs him to keep going, but—despite being many times bigger and stronger than Atreyu, the horse just sinks into the swamp, literally drowning in despair.
See the scene: The Neverending Story movie clip – Artax and the Swamp of Sadness (1984)
Wow, they really don’t make kids’ movies like they used to, do they?
But, depression is very much like that, and advice “exercise to feel less depressed!” falls short of actually being helpful, when one is too depressed to do it.
If you’re in the position of supporting someone who’s depressed, the best tool in your toolbox will be not “here’s why you should do this” (they don’t care; not because they’re an uncaring person by nature, but because they are physiologically impeded from caring about themself at this time), but rather:
“please do this with me”
The reason this has a better chance of working is because the depressed person will in all likelihood be unable to care enough to raise and/or maintain an objection, and while they can’t remember why they should care about themself, they’re more likely to remember that they should care about you, and so will go with your want/need more easily than with their own. It’s not a magic bullet, but it’s worth a shot.
What if I’m the depressed person, though?
Honestly, the same, if there’s someone around you that you do care about; do what you can to look after you, for them, if that means you can find some extra motivation.
But I’m all alone… what now?
Firstly, you don’t have to be alone. There are free services that you can access, for example:
- US: https://nami.org/help
- Canada: https://www.wellnesstogether.ca/en-CA
- UK: https://www.samaritans.org/
…which varyingly offer advice, free phone services, webchats, and the like.
But also, there are ways you can look after yourself a little bit; do the things you’d advise someone else to do, even if you’re sure they won’t work:
- Take a little walk around the block
- Put the lights on when you’re not sleeping
- For that matter, get out of bed when you’re not sleeping. Literally lie on the floor if necessary, but change your location.
- Change your bedding, or at least your clothes
- If changing the bedding is too much, change just the pillowcase
- If changing your clothes is too much, change just one item of clothing
- Drink some water; it won’t magically cure you, but you’ll be in slightly better order
- On the topic of water, splash some on your face, if showering/bathing is too much right now
- Do something creative (that’s not self-harm). You may scoff at the notion of “art therapy” helping, but this is a way to get at least some of the lights on in areas of your brain that are a little dark right now. Worst case scenario is it’ll be a distraction from your problems, so give it a try.
- Find a connection to community—whatever that means to you—even if you don’t feel you can join it right now. Discover that there are people out there who would welcome you if you were able to go join them. Maybe one day you will!
- Hiding from the world? That’s probably not healthy, but while you’re hiding, take the time to read those books (write those books, if you’re so inclined), learn that new language, take up chess, take up baking, whatever. If you can find something that means anything to you, go with that for now, ride that wave. Motivation’s hard to come by during depression and you might let many things slide; you might as well get something out of this period if you can.
If you’re not depressed right now but you know you’re predisposed to such / can slip that way?
Write yourself instructions now. Copy the above list if you like.
Most of all: have a “things to do when I don’t feel like doing anything” list.
If you only take one piece of advice from today’s newsletter, let that one be it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Getting Your Messy Life In Order
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Getting Your Messy Life In Order
We’ve touched on this before by recommending the book, but today we’re going to give an overview of the absolute most core essentials of the “Getting Things Done” method. If you’re unfamiliar, this will be enough to get you going. If you’re already familiar, this may be a handy reminder!
First, you’ll need:
- A big table
- A block of small memo paper squares—post-it note sized, but no need to be sticky.
- A block of A4 printer paper
- A big trash bag
Gathering everything
Gather up not just all your to-dos, but: all sources of to-dos, too, and anything else that otherwise needs “sorting”.
Put them all in one physical place—a dining room table may have enough room. You’ll need a lot of room because you’re going to empty our drawers of papers, unopened (or opened and set aside) mail. Little notes you made for yourself, things stuck on the fridge or memo boards. Think across all areas of your life, and anything you’re “supposed” to do, write it down on a piece of paper. No matter what area of your life, no matter how big or small.
Whether it’s “learn Chinese” or “take the trash out”, write it down, one item per piece of paper (hence the block of little memo squares).
Sorting everything
Everything you’ve gathered needs one of three things to happen:
- You need to take some action (put it in a “to do” pile)
- You may need it later sometime (put it in a “to file” pile)
- You don’t need it (put it in the big trash bag for disposal)
What happens next will soothe you
- Dispose of the things you put for disposal
- File the things for filing in a single alphabetical filing system. If you don’t have one, you’ll need to get one, so write that down and add it to the “to do” pile.
- You will now process your “to dos”
Processing the “to dos”
The pile you have left is now your “inbox”. It’s probably huge; later it’ll be smaller, maybe just a letter-tray on your desk.
Many of your “to dos” are actually not single action items, they’re projects. If something requires more than one step, it’s a project.
Take each item one-by-one. Do this in any order; you’re going to do this as quickly as possible! Now, ask yourself: is this a single-action item that I could do next, without having to do something else first?
- If yes: put it in a pile marked “next action”
- If no: put it in a pile marked “projects”.
Take a sheet of A4 paper and fold it in half. Write “Next Action” on it, and put your pile of next actions inside it.
Take a sheet of A4 paper per project and write the name of the project on it, for example “Learn Chinese”, or “Do taxes”. Put any actions relating to that project inside it.
Likely you don’t know yet what the first action will be, or else it’d be in your “Next Action” pile, so add an item to each project that says “Brainstorm project”.
Processing the “Next Action” pile
Again you want to do this as quickly as possible, in any order.
For each item, ask yourself “Do I care about this?” If the answer is no, ditch that item, and throw it out. That’s ok. Things change and maybe we no longer want or need to do something. No point in hanging onto it.
For each remaining item, ask yourself “can this be done in under 2 minutes?”.
- If yes, do it, now. Throw away the piece of paper for it when you’re done.
- If no, ask yourself:”could I usefully delegate this to someone else?” If the answer is yes, do so.
If you can’t delegate it, ask yourself: “When will be a good time to do this?” and schedule time for it. A specific, written-down, clock time on a specific calendar date. Input that into whatever you use for scheduling things. If you don’t already use something, just use the calendar app on whatever device you use most.
The mnemonic for the above process is “Do/Defer/Delegate/Ditch”
Processing projects:
If you don’t know where to start with a project, then figuring out where to start is your “Next Action” for that project. Brainstorm it, write down everything you’ll need to do, and anything that needs doing first.
The end result of this is:
- You will always, at any given time, have a complete (and accessible) view of everything you are “supposed” to do.
- You will always, at any given time, know what action you need to take next for a given project.
- You will always, when you designate “work time”, be able to get straight into a very efficient process of getting through your to-dos.
Keeping on top of things
- Whenever stuff “to do something with/about” comes to you, put it in your physical “inbox” place—as mentioned, a letter-tray on a desk should suffice.
- At the start of each working day, quickly process things as described above. This should be a small daily task.
- Once a week, do a weekly review to make sure you didn’t lose sight of something.
- Monthly, quarterly, and annual reviews can be a good practice too.
How to do those reviews? Topic for another day, perhaps.
Or:
Check out the website / Check out GTD apps / Check out the book
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: