What is AuDHD? 5 important things to know when someone has both autism and ADHD
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may have seen some new ways to describe when someone is autistic and also has attention-deficit hyperactivity disorder (ADHD). The terms “AuDHD” or sometimes “AutiADHD” are being used on social media, with people describing what they experience or have seen as clinicians.
It might seem surprising these two conditions can co-occur, as some traits appear to be almost opposite. For example, autistic folks usually have fixed routines and prefer things to stay the same, whereas people with ADHD usually get bored with routines and like spontaneity and novelty.
But these two conditions frequently overlap and the combination of diagnoses can result in some unique needs. Here are five important things to know about AuDHD.

1. Having both wasn’t possible a decade ago
Only in the past decade have autism and ADHD been able to be diagnosed together. Until 2013, the Diagnostic and Statistical Manual of Mental Disorders (DSM) – the reference used by health workers around the world for definitions of psychological diagnoses – did not allow for ADHD to be diagnosed in an autistic person.
The manual’s fifth edition was the first to allow for both diagnoses in the same person. So, folks diagnosed and treated prior to 2013, as well as much of the research, usually did not consider AuDHD. Instead, children and adults may have been “assigned” to whichever condition seemed most prominent or to be having the greater impact on everyday life.
2. AuDHD is more common than you might think
Around 1% to 4% of the population are autistic.
They can find it difficult to navigate social situations and relationships, prefer consistent routines, find changes overwhelming and repetition soothing. They may have particular sensory sensitivities.
ADHD occurs in around 5–8% of children and adolescents and 2–6% of adults. Characteristics can include difficulties with focusing attention in a flexible way, resulting in procrastination, distraction and disorganisation. People with ADHD can have high levels of activity and impulsivity.
Studies suggest around 40% of those with ADHD also meet diagnostic criteria for autism and vice versa. The co-occurrence of having features or traits of one condition (but not meeting the full diagnostic criteria) when you have the other, is even more common and may be closer to around 80%. So a substantial proportion of those with autism or ADHD who don’t meet full criteria for the other condition, will likely have some traits.
3. Opposing traits can be distressing
Autistic people generally prefer order, while ADHDers often struggle to keep things organised. Autistic people usually prefer to do one thing at a time; people with ADHD are often multitasking and have many things on the go. When someone has both conditions, the conflicting traits can result in an internal struggle.
For example, it can be upsetting when you need your things organised in a particular way but ADHD traits result in difficulty consistently doing this. There can be periods of being organised (when autistic traits lead) followed by periods of disorganisation (when ADHD traits dominate) and feelings of distress at not being able to maintain organisation.
There can be eventual boredom with the same routines or activities, but upset and anxiety when attempting to transition to something new.
Autistic special interests (which are often all-consuming, longstanding and prioritised over social contact), may not last as long in AuDHD, or be more like those seen in ADHD (an intense deep dive into a new interest that can quickly burn out).
Autism can result in quickly being overstimulated by sensory input from the environment such as noises, lighting and smells. ADHD is linked with an understimulated brain, where intense pressure, novelty and excitement can be needed to function optimally.
For some people the conflicting traits may result in a balance where people can find a middle ground (for example, their house appears tidy but the cupboards are a little bit messy).
There isn’t much research yet into the lived experience of this “trait conflict” in AuDHD, but there are clinical observations.
4. Mental health and other difficulties are more frequent
Our research on mental health in children with autism, ADHD or AuDHD shows children with AuDHD have higher levels of mental health difficulites than autism or ADHD alone.
This is a consistent finding with studies showing higher mental health difficulties such as depression and anxiety in AuDHD. There are also more difficulties with day-to-day functioning in AuDHD than either condition alone.
So there is an additive effect in AuDHD of having the executive foundation difficulties found in both autism and ADHD. These difficulties relate to how we plan and organise, pay attention and control impulses. When we struggle with these it can greatly impact daily life.
5. Getting the right treatment is important
ADHD medication treatments are evidence-based and effective. Studies suggest medication treatment for ADHD in autistic people similarly helps improve ADHD symptoms. But ADHD medications won’t reduce autistic traits and other support may be needed.
Non-pharmacological treatments such as psychological or occupational therapy are less researched in AuDHD but likely to be helpful. Evidence-based treatments include psychoeducation and psychological therapy. This might include understanding one’s strengths, how traits can impact the person, and learning what support and adjustments are needed to help them function at their best. Parents and carers also need support.
The combination and order of support will likely depend on the person’s current functioning and particular needs. https://www.youtube.com/embed/pMx1DnSn-eg?wmode=transparent&start=0 ‘Up until recently … if you had one, you couldn’t have the other.’
Do you relate?
Studies suggest people may still not be identified with both conditions when they co-occur. A person in that situation might feel misunderstood or that they can’t fully relate to others with a singular autism and ADHD diagnosis and something else is going on for them.
It is important if you have autism or ADHD that the other is considered, so the right support can be provided.
If only one piece of the puzzle is known, the person will likely have unexplained difficulties despite treatment. If you have autism or ADHD and are unsure if you might have AuDHD consider discussing this with your health professional.
Tamara May, Psychologist and Research Associate in the Department of Paediatrics, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rebounding Into The Best Of Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Trampoline” is a brand-name that’s been popularized as a generic name, and “rebounding”, the name used in this video, is the same thing as “trampolining”. With that in mind, let us bounce swiftly onwards:
Surprising benefits
It’s easy to think “isn’t that cheating?” to the point that such “cheating” could be useless, since surely the device is doing most of the work?
The thing is, while indeed it’s doing a lot of the work for you, your muscles are still doing a lot—mostly stabilization work, which is of course a critical thing for our muscles to be able to do. While it’s rare that we need to do a somersault in everyday life, it’s common that we have to keep ourselves from falling over, after all.
It also represents a kind of gentle resistance exercise, and as such, improves bone density—something first discovered during NASA research for astronauts. Other related benefits pertain to the body’s ability to deal with acceleration and deceleration; it also benefits the lymphatic system, which unlike the blood’s circulatory system, has no pump of its own. Rebounding does also benefit the cardiovascular system, though, as now the heart gets confused (in the healthy way, a little like it gets confused with high-intensity interval training).
Those are the main evidence-based benefits; anecdotally (but credibly, since these things can be said of most exercise) it’s also claimed that it benefits posture, improves sleep and mood, promotes weight loss and better digestion, reduces bloating, improves skin (the latter being due to improved circulation), and alleviates arthritis (most moderate exercise improves immune response, and thus reduces chronic inflammation, so again, this is reasonable, even if anecdotal).
For more details on all of these and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Exercise Less, Move More
- How To Do HIIT (Without Wrecking Your Body)
- Resistance Is Useful! (Especially As We Get Older)
- HIIT, But Make It HIRT
- The Lymphatic System Against Cancer & More
Take care!
Share This Post
-
Does Eating Shellfish Contribute To Gout?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
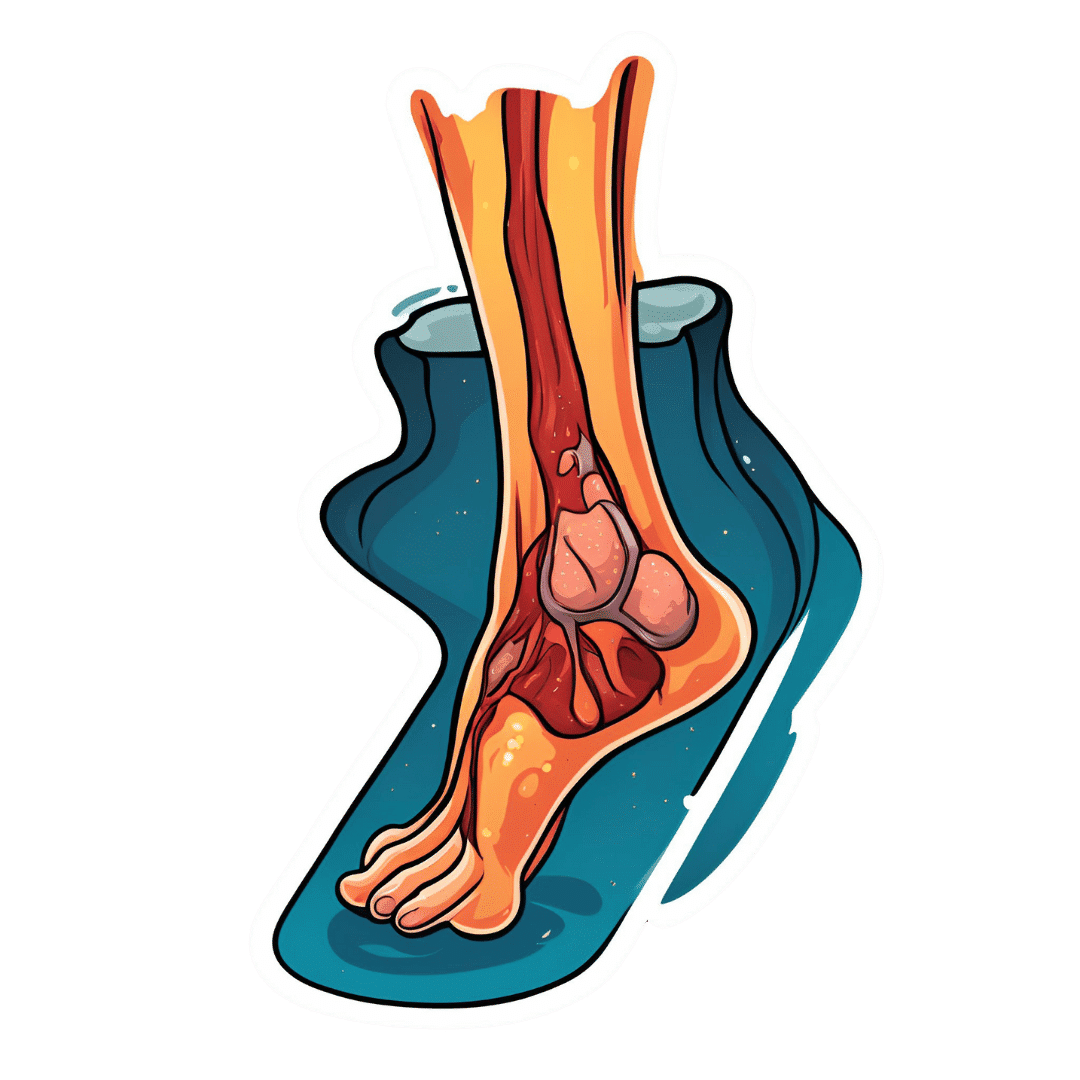
❝I have a question about seafood as healthy, doesn’t eating shellfish contribute to gout?❞
It can do! Gout (a kind of inflammatory arthritis characterized by the depositing of uric acid crystals in joints) has many risk factors, and diet is one component, albeit certainly the most talked-about one.
First, you may be wondering: isn’t all arthritis inflammatory? Since arthritis is by definition the inflammation of joints, this is a reasonable question, but when it comes to classifying the kinds, “inflammatory” arthritis is caused by inflammation, while “non-inflammatory” arthritis (a slightly confusing name) merely has inflammation as one of its symptoms (and is caused by physical wear-and-tear). For more information, see:
- Tips For Avoiding/Managing Rheumatoid Arthritis ←inflammatory
- Tips For Avoiding/Managing Osteoarthritis ← “non-inflammatory”
As for gout specifically, top risk factors include:
- Increasing age: risk increases with age
- Being male: women do get gout, but much less often
- Hypertension: all-cause hypertension is the biggest reasonably controllable factor
There’s not a lot we can do about age (but of course, looking after our general health will tend to slow biological aging, and after all, diseases only care about the state of our body, not what the date on the calendar is).
As for sex, this risk factor is hormones, and specifically has to do with estrogen and testosterone’s very different effects on the immune system (bearing in mind that chronic inflammation is a disorder of the immune system). However, few if any men would take up feminizing hormone therapy just to lower their gout risk!
That leaves hypertension, which happily is something that we can all (barring extreme personal circumstances) do quite a bit about. Here’s a good starting point:
Hypertension: Factors Far More Relevant Than Salt
…and for further pointers:
How To Lower Your Blood Pressure (Cardiologists Explain)
As for diet specifically (and yes, shellfish):
The largest study into this (and thus, one of the top ones cited in a lot of other literature) looked at 47,150 men with no history of gout at the baseline.
So, with the caveat that their findings could have been different for women, they found:
- Eating meat in general increased gout risk
- Narrowing down specific meats: beef, pork, and lamb were the worst offenders
- Eating seafood in general increased gout risk
- Narrowing down specific seafoods: all seafoods increased gout risk within a similar range
- As a specific quirk of seafoods: the risk was increased if the man had a BMI under 25
- Eating dairy in general was not associated with an increased risk of gout
- Narrowing down specific dairy foods: low-fat dairy products such as yogurt were associated with a decreased risk of gout
- Eating purine-rich vegetables in general was not associated with an increased risk of gout
- Narrowing down to specific purine-rich vegetables: no purine-rich vegetable was associated with an increase in the risk of gout
Dairy products were included in the study, as dairy products in general and non-fermented dairy products in particular are often associated with increased inflammation. However, the association was simply not found to exist when it came to gout risk.
Purine-rich vegetables were included in the study, as animal products highest in purines have typically been found to have the worst effect on gout. However, the association was simply not found to exist when it came to plants with purines.
You can read the full study here:
Purine-Rich Foods, Dairy and Protein Intake, and the Risk of Gout in Men
So, the short answer to your question of “doesn’t eating shellfish contribute to the risk of gout” is:
Yes, it can, but occasional consumption probably won’t result in gout unless you have other risk factors going against you.
If you’re a slim male 80-year-old alcoholic smoker with hypertension, then definitely do consider skipping the lobster, but honestly, there may be bigger issues to tackle there.
And similarly, obviously skip it if you have a shellfish allergy, and if you’re vegan or vegetarian or abstain from shellfish for religious reasons, then you can certainly live very healthily without ever having any.
See also: Do We Need Animal Products, To Be Healthy?
For most people most of the time, a moderate consumption of seafood, including shellfish if you so desire, is considered healthy.
As ever, do speak with your own doctor to know for sure, as your individual case may vary.
For reference, this question was surely prompted by the article:
Lobster vs Crab – Which is Healthier?
Take care!
Share This Post
-
Most adults will gain half a kilo this year – and every year. Here’s how to stop ‘weight creep’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As we enter a new year armed with resolutions to improve our lives, there’s a good chance we’ll also be carrying something less helpful: extra kilos. At least half a kilogram, to be precise.
“Weight creep” doesn’t have to be inevitable. Here’s what’s behind this sneaky annual occurrence and some practical steps to prevent it.
Allgo/Unsplash Small gains add up
Adults tend to gain weight progressively as they age and typically gain an average of 0.5 to 1kg every year.
While this doesn’t seem like much each year, it amounts to 5kg over a decade. The slow-but-steady nature of weight creep is why many of us won’t notice the extra weight gained until we’re in our fifties.
Why do we gain weight?
Subtle, gradual lifestyle shifts as we progress through life and age-related biological changes cause us to gain weight. Our:
- activity levels decline. Longer work hours and family commitments can see us become more sedentary and have less time for exercise, which means we burn fewer calories
- diets worsen. With frenetic work and family schedules, we sometimes turn to pre-packaged and fast foods. These processed and discretionary foods are loaded with hidden sugars, salts and unhealthy fats. A better financial position later in life can also result in more dining out, which is associated with a higher total energy intake
- sleep decreases. Busy lives and screen use can mean we don’t get enough sleep. This disturbs our body’s energy balance, increasing our feelings of hunger, triggering cravings and decreasing our energy
Insufficient sleep can increase our appetite. Craig Adderley/Pexels - stress increases. Financial, relationship and work-related stress increases our body’s production of cortisol, triggering food cravings and promoting fat storage
- metabolism slows. Around the age of 40, our muscle mass naturally declines, and our body fat starts increasing. Muscle mass helps determine our metabolic rate, so when our muscle mass decreases, our bodies start to burn fewer calories at rest.
We also tend to gain a small amount of weight during festive periods – times filled with calorie-rich foods and drinks, when exercise and sleep are often overlooked. One study of Australian adults found participants gained 0.5 kilograms on average over the Christmas/New Year period and an average of 0.25 kilograms around Easter.
Why we need to prevent weight creep
It’s important to prevent weight creep for two key reasons:
1. Weight creep resets our body’s set point
Set-point theory suggests we each have a predetermined weight or set point. Our body works to keep our weight around this set point, adjusting our biological systems to regulate how much we eat, how we store fat and expend energy.
When we gain weight, our set point resets to the new, higher weight. Our body adapts to protect this new weight, making it challenging to lose the weight we’ve gained.
But it’s also possible to lower your set point if you lose weight gradually and with an interval weight loss approach. Specifically, losing weight in small manageable chunks you can sustain – periods of weight loss, followed by periods of weight maintenance, and so on, until you achieve your goal weight.
Holidays can also come with weight gain. Zan Lazarevic/Unsplash 2. Weight creep can lead to obesity and health issues
Undetected and unmanaged weight creep can result in obesity which can increase our risk of heart disease, strokes, type 2 diabetes, osteoporosis and several types of cancers (including breast, colorectal, oesophageal, kidney, gallbladder, uterine, pancreatic and liver).
A large study examined the link between weight gain from early to middle adulthood and health outcomes later in life, following people for around 15 years. It found those who gained 2.5 to 10kg over this period had an increased incidence of type 2 diabetes, heart disease, strokes, obesity-related cancer and death compared to participants who had maintained a stable weight.
Fortunately, there are steps we can take to build lasting habits that will make weight creep a thing of the past.
7 practical steps to prevent weight creep
1. Eat from big to small
Aim to consume most of your food earlier in the day and taper your meal sizes to ensure dinner is the smallest meal you eat.
A low-calorie or small breakfast leads to increased feelings of hunger, specifically appetite for sweets, across the course of the day.
We burn the calories from a meal 2.5 times more efficiently in the morning than in the evening. So emphasising breakfast over dinner is also good for weight management.
Aim to consume bigger breakfasts and smaller dinners. Michael Burrows/Pexels 2. Use chopsticks, a teaspoon or an oyster fork
Sit at the table for dinner and use different utensils to encourage eating more slowly.
This gives your brain time to recognise and adapt to signals from your stomach telling you you’re full.
3. Eat the full rainbow
Fill your plate with vegetables and fruits of different colours first to support eating a high-fibre, nutrient-dense diet that will keep you feeling full and satisfied.
Meals also need to be balanced and include a source of protein, wholegrain carbohydrates and healthy fat to meet our dietary needs – for example, eggs on wholegrain toast with avocado.
4. Reach for nature first
Retrain your brain to rely on nature’s treats – fresh vegetables, fruit, honey, nuts and seeds. In their natural state, these foods release the same pleasure response in the brain as ultra-processed and fast foods, helping you avoid unnecessary calories, sugar, salt and unhealthy fats.
5. Choose to move
Look for ways to incorporate incidental activity into your daily routine – such as taking the stairs instead of the lift – and boost your exercise by challenging yourself to try a new activity.
Just be sure to include variety, as doing the same activities every day often results in boredom and avoidance.
Try new activities or sports to keep your interest up. Cottonbro Studio/Pexels 6. Prioritise sleep
Set yourself a goal of getting a minimum of seven hours of uninterrupted sleep each night, and help yourself achieve it by avoiding screens for an hour or two before bed.
7. Weigh yourself regularly
Getting into the habit of weighing yourself weekly is a guaranteed way to help avoid the kilos creeping up on us. Aim to weigh yourself on the same day, at the same time and in the same environment each week and use the best quality scales you can afford.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Clinical Trials Director, Department of Endocrinology, RPA Hospital, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
What Macronutrient Balance Is Right For You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I want to learn more about macros. Can you cover that topic?❞
That’s a little broader than we usually go for, given the amount of space we have, but let’s give it a go!
Macronutrients, or “macros”, are the nutrients that we typically measure in grams rather than milligrams or micrograms, and are:
- Carbohydrates
- …and what kinds, of which usually the focus is on how much is sugars as opposed to more complex carbs that take longer to break down. See also: Should You Go Light Or Heavy On Carbs?
- …and of the sugars, the interested may further categorize them into sucrose, fructose, etc. See also: Which Sugars Are Healthier, And Which Are Just The Same?
- Proteins
- …of which, the amino acid make-up is generally considered a matter of micronutrients. See also: Protein: How Much Do We Need, Really?
- Fats
- …and what kinds, i.e. monounsaturated vs polyunsaturated vs saturated. See also: Saturated Fat: What’s The Truth?
- …and then the interested may further categorize them for their fatty acids / triglycerides profile, etc. See also: What Omega-3 Fatty Acids Really Do For Us
- Fiber
- …which often gets ignored by people counting macros, as “stuff that doesn’t do anything”, despite it in fact being very important for health. See also: Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Water
- …which again tends to get disregarded but is very arguably a critical macronutrient. See also: Busting The Myth of “Eight Glasses Of Water A Day”
In terms of how much we need of each, you can read more in the above-linked articles, but:
- General scientific consensus is we need plenty of fiber (30 or 40g per day is good) and water (highly dependent on climate and activity), and there’s a clear minimum requisite for protein (usually put at around 1g of protein per day per 1kg of body weight).
- There is vigorous debate in the general health community about what the best ratio of carbs to fat is.
The reality is that humans are quite an adaptable species, and while we absolutely do need at least some of both (carbohydrates and fats), we can play around with the ratios quite a bit, provided we don’t get too extreme about it.
While some influence is social and often centered around weight loss (see for example keto which seeks to minimize carbs, and volumetrics, which seeks maximise volume-to-calorie ratio, which de facto tends to minimize fats), some of what drives us to lean one way or the other will be genetics, too—dependent on what our ancestors ate more or less of.
Writer’s example: my ancestors could not grow much grain (or crops in general) where they were, so they got more energy from such foods as whale and seal fat (with protein coming more from reindeer). Now, biology is not destiny, and I personally enjoy a vegan diet, but my genes are probably why I am driven to get most of my daily calories from fat (of which, a lot of fatty nuts (don’t tell almonds, but I prefer walnuts and cashews) and healthy oils such as olive oil, avocado oil, and coconut oil).
However! About that adaptability. Provided we make changes slowly, we can usually adjust our diet to whatever we want it to be, including whether we get our energy more from carbs or fats. The reason we need to make changes slowly is because our gut needs time to adjust. For example, if your vegan writer here were to eat her ancestrally-favored foods now, I’d be very ill, because my gut microbiome has no idea what to do with animal products anymore, no matter what genes I have. In contrast, if an enthusiastic enjoyer of a meat-heavy diet were to switch to my fiber-rich diet overnight, they’d be very ill.
So: follow your natural inclinations, make any desired changes slowly, and if in doubt, it’s hard to go wrong with enjoying carbs and fats in moderation.
Learn more: Intuitive Eating Might Not Be What You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Carbohydrates
-
Rewire Your OCD Brain – by Dr. Catherine Pittman & Dr. William Youngs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
OCD is just as misrepresented in popular media as many other disorders, and in this case, it’s typically not “being a neat freak” or needing to alphabetize things, so much as having uncontrollable obsessive intrusive thoughts, and often in response to those, unwanted compulsions. This can come from unchecked spiralling anxiety, and/or PTSD, for example.
What Drs. Pittman & Young offer is an applicable set of solutions, to literally rewire the brain (insofar as synapses can be considered neural wires). Leveraging neuroplasticity to work with us rather than against us, the authors talk us through picking apart the crossed wires, and putting them back in more helpful ways.
This is not, by the way, a book of CBT, though it does touch on that too.
Mostly, the book explains—clearly and simply and sometimes with illustrations—what is going wrong for us neurologically, and how to neurologically change that.
Bottom line: whether you have OCD or suffer from anxiety or just need help dealing with obsessive thoughts, this book can help a lot in, as the title suggests, rewiring that.
Click here to check out Rewire Your OCD Brain, and banish obsessive thoughts!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eating disorders don’t just affect teen girls. The risk may go up around pregnancy and menopause too
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eating disorders impact more than 1.1 million people in Australia, representing 4.5% of the population. These disorders include binge eating disorder, bulimia nervosa, and anorexia nervosa.
Meanwhile, more than 4.1 million people (18.9%) are affected by body dissatisfaction, a major risk factor for some types of eating disorders.
But what image comes to mind first when you think of someone with an eating disorder or body image concerns? Is it a teenage girl? If so, you’re definitely not alone. This is often the image we see in popular media.
Eating disorders and body image concerns are most common in teenage girls, but their prevalence in adults, particularly in women, aged in their 30s, 40s and 50s, is actually close behind.
So what might be going on with girls and women in these particular age groups to create this heightened risk?
Drazen Zigic/Shutterstock The 3 ‘P’s
We can consider women’s risk periods for body image issues and eating disorders as the three “P”s: puberty (teenagers), pregnancy (30s) and perimenopause and menopause (40s, 50s).
A recent report from The Butterfly Foundation showed the three highest prevalence groups for body image concerns are teenage girls aged 15–17 (39.9%), women aged 55–64 (35.7%) and women aged 35–44 (32.6%).
We acknowledge there’s a wide age range for when girls and women will go through these phases of life. For example, a small proportion of women will experience premature menopause before 40, and not all women will become pregnant.
Variations in the way eating disorder symptoms are measured across different studies can make it difficult to draw direct comparisons, but here’s a snapshot of what the evidence tells us.
Puberty
In a review of studies looking at children aged six to adolescents aged 18, 30% of girls in this age group reported disordered eating, compared to 17% of boys. Rates of disordered eating were higher as children got older.
Pregnancy
During pregnancy, eating disorder prevalence is estimated at 7.5%. Almost 70% of women are dissatisfied with their body weight and figure in the post-partum period.
Pregnancy can represent a major change in identity and self-perception. Pormezz/Shutterstock Perimenopause
It’s estimated more than 73% of midlife women aged 42–52 are unsatisfied with their body weight. However, only a portion of these women would have been going through the menopause transition at the time of this study.
The prevalence of eating disorders is around 3.5% in women over 40 and 1–2% in men at the same stage.
So what’s going on?
Although we’re not sure of the exact mechanisms underlying eating disorder and body dissatisfaction risk during the three “P”s, it’s likely a combination of factors are at play.
These life stages involve significant reproductive hormonal changes (for example, fluctuations in oestrogen and progesterone) which can lead to increases in appetite or binge eating and changes in body composition. These changes can result in concerns about body weight and shape.
These stages can also represent a major change in identity and self-perception. A girl going through puberty may be concerned about turning into an “adult woman” and changes in attitudes of those around her, such as unwanted sexual attention.
Pregnancy obviously comes with significant body size and shape changes. Pregnant women may also feel their body is no longer their own.
While social pressures to be thin can stop during pregnancy, social expectations arguably return after birth, demanding women “bounce back” to their pre-pregnancy shape and size quickly.
Women going through menopause commonly express concerns about a loss of identity. In combination with changes in body composition and a perception their appearance is departing from youthful beauty ideals, this can intensify body dissatisfaction and increase the risk of eating disorders.
These periods of life can each also be incredibly stressful, both physically and psychologically.
For example, a girl going through puberty may be facing more adult responsibilities and stress at school. A pregnant woman could be taking care of a family while balancing work and other demands. A woman going through menopause could potentially be taking care of multiple generations (teenage children, ageing parents) while navigating the complexities of mid-life.
Research has shown interpersonal problems and stressors can increase the risk of eating disorders.
Body image concerns and eating disorders are not limited to teenage girls. transly/Unsplash, CC BY We need to do better
Unfortunately most of the policy and research attention currently seems to be focused on preventing and treating eating disorders in adolescents rather than adults. There also appears to be a lack of understanding among health professionals about these issues in older women.
In research I (Gemma) led with women who had experienced an eating disorder during menopause, participants expressed frustration with the lack of services that catered to people facing an eating disorder during this life stage. Participants also commonly said health professionals lacked education and training about eating disorders during menopause.
We need to increase awareness among health professionals and the general public about the fact eating disorders and body image concerns can affect women of any age – not just teenage girls. This will hopefully empower more women to seek help without stigma, and enable better support and treatment.
Jaycee Fuller from Bond University contributed to this article.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14. For concerns around eating disorders or body image visit the Butterfly Foundation website or call the national helpline on 1800 33 4673.
Gemma Sharp, Professor, NHMRC Emerging Leadership Fellow & Senior Clinical Psychologist, The University of Queensland; Amy Burton, Lecturer in Clinical Psychology, University of Technology Sydney, and Megan Lee, Assistant Professor, Psychology, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: