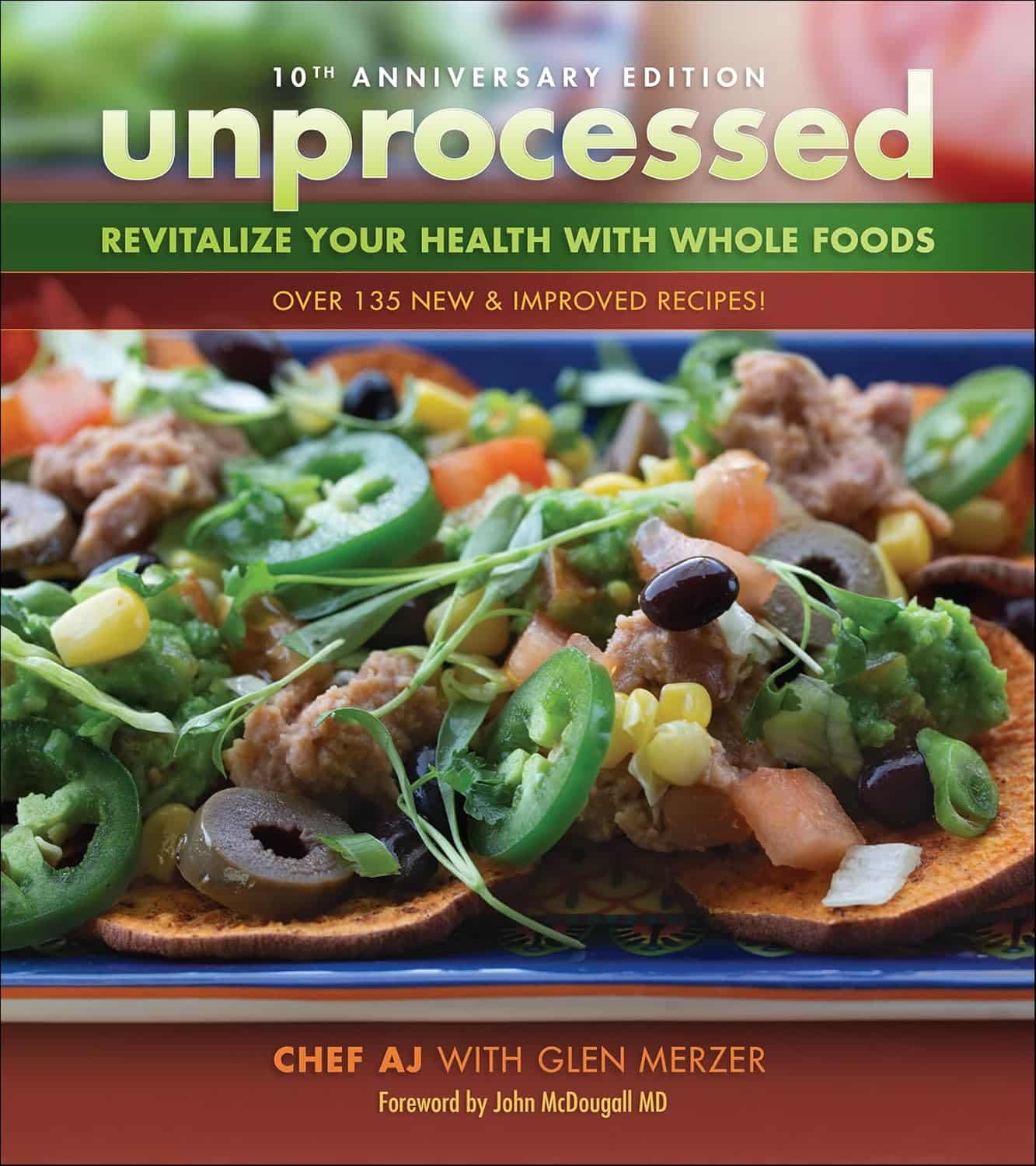
Unprocessed 10th Anniversary Edition – by Abbie Jay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The main premise of this book is cooking…
- With nutritious whole foods
- Without salt, oil, sugar (“SOS”)
It additionally does it without animal products and without gluten, and (per “nutritious whole foods”), and, as the title suggests, avoiding anything that’s more than very minimally processed. Remember, for example, that if something is fermented, then that fermentation is a process, so the food has been processed—just, minimally.
This is a revised edition, and it’s been adjusted to, for example, strip some of the previous “no salt” low-sodium options (such as tamari with 233mg/tsp sodium, compared to salt’s 2,300mg/tsp sodium).
You may be wondering: what’s left? Tasty, well-seasoned, plant-based food, that leans towards the “comfort food” culinary niche.
Enough to sate the author, after her own battles with anorexia and obesity (in that order) and finally, after various hospital trips, getting her diet where it needed to be for the healthy lifestyle that she lives now, while still getting to eat such dishes as “Chef AJ’s Disappearing Lasagna” and peanut butter fudge truffles and 151 more.
Bottom line: if you want whole-food plant-based comfort-food cooking that’s healthy in general and especially heart-healthy, this book has plenty of that.
Click here to check out Unprocessed: 10th Anniversary Edition, and… Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Sleep Solution – by Dr. Chris Winter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book’s blurb contains a bold claim:
❝If you want to fix your sleep problems, Internet tips and tricks aren’t going to do it for you. You need to really understand what’s going on with your sleep—both what your problems are and how to solve them.❞
So, how well does it deliver, on the strength of being a whole book rather than an Internet article?
Well, for sure we wouldn’t have the room to include all the information that Dr. Winter does, in one of our main feature articles here (we’d need to spread it out over several weeks, at least).
He examines very thoroughly what is going on with sleep, sleep disturbance, and sleep deprivation. What’s going on with the different phases of sleep (far more than your phone’s sleep app will), and how imbalances in these can cause problems.
While the usual sleep hygiene tips do get a mention, he broadly assumes we know that part already. Instead, he focuses on aligning as many components as possible of our rich and interesting circadian rhythm. Yes, even if that means clawing our way out of insomnia and/or a bad sleep schedule (or lack of coherent sleep schedule) first. He gives plenty of practical advice on how to do that.
Bottom line: if you’d like to more deeply understand sleep, what is or isn’t wrong with yours, and how you can fix it, this book is a great resource.
Click here to check out The Sleep Solution, and enjoy the benefits of better rest!
Share This Post
-
Food for Life – by Dr. Tim Spector
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is, as the author puts it, “an eater’s guide to food and nutrition”. Rather than telling us what to eat or not eat, he provides an overview of what the latest science has to say about various foods, and leaves us to make our own informed decisions.
He also stands firmly by the “personalized nutrition” idea that he introduced in his previous book which we reviewed the other day, and gives advice on what tests we might like to perform.
The writing style is accessible, without shying away from reference to hard science. Dr. Spector provides lots of information about key chemicals, genes, gut bacteria, and more—as well as simply providing a very enjoyable read along the way.
Bottom line: if you’d like a much better idea of what food is (and isn’t) doing what, this book is an invaluable resource.
Click here to check out Food for Life, and make the best decisions for you!
Share This Post
-
Edamame vs Soybeans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing edamame to soybeans, we picked the soybeans.
Why?
You may be thinking: aren’t edamame soybeans? And yes, yes they are. But just like our many instances of pitting Brassica oleracea vs Brassica oleracea (one species, many cultivars e.g. broccoli, cauliflower, kale, cabbage, Brussels sprouts, etc), there are still differences. In this case, edamame and soybeans aren’t even different cultivars, what are conventionally called edamame are just the young beans of the plant, while what are conventionally called soybeans are the mature beans of the plant.
The main nutritional difference is: as they get older, they lose vitamins and gain minerals. More on that later. But first, “main difference” isn’t “only difference”, so…
In terms of macros, edamame have more carbs, while soybeans have a little more fiber and a lot more protein. An easy win for the mature soybeans.
In the category of vitamins, edamame have more of vitamins A, B1, B3, B5, B9, C, E, K, and choline, while soybeans have more of vitamins B2 and B6. A clear win for edamame, this time.
When it comes to minerals, the nutritional tables are turned, and edamame have more manganese and zinc, while soybeans have more calcium, copper, iron, magnesium, phosphorus, potassium, and selenium. An easy win for soybeans.
Adding up the sections makes for a two-to-one victory for soybeans, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
Related Posts
-
Savoy Cabbage vs Pak Choi – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing savoy cabbage to pak choi, we picked the savoy.
Why?
Looking at the macros first, the savoy has a little more protein, just under 3x the carbs, and just over 3x the fiber. A modest yet respectable win for savoy.
In terms of vitamins, savoy has more of vitamins B1, B5, B9, E, K, and choline, while pak choi has more of vitamins A, B2, B3, and C. Thus, a 6:4 win for savoy.
When it comes to minerals, savoy has more copper, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pak choi has more calcium, iron, and potassium. So this time, a 7:3 win for savoy.
On the other hand, pak choi scores higher on the polyphenols side, especially in the categories of kaempferol and quercetin.
Still, adding up the sections, we conclude this one’s an overall win for savoy cabbage. Of course, enjoy either or both, though!
Want to learn more?
You might like to read:
Fight Inflammation & Protect Your Brain, With Quercetin
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We’re the ‘allergy capital of the world’. But we don’t know why food allergies are so common in Australian children
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australia has often been called the “allergy capital of the world”.
An estimated one in ten Australian children develop a food allergy in their first 12 months of life. Research has previously suggested food allergies are more common in infants in Australia than infants living in Europe, the United States or Asia.
So why are food allergies so common in Australia? We don’t know exactly – but local researchers are making progress in understanding childhood allergies all the time.
Miljan Zivkovic/Shutterstock What causes food allergies?
There are many different types of reactions to foods. When we refer to food allergies in this article, we’re talking about something called IgE-mediated food allergy. This type of allergy is caused by an immune response to a particular food.
Reactions can occur within minutes of eating the food and may include swelling of the face, lips or eyes, “hives” or welts on the skin, and vomiting. Signs of a severe allergic reaction (anaphylaxis) include difficulty breathing, swelling of the tongue, swelling in the throat, wheeze or persistent cough, difficulty talking or a hoarse voice, and persistent dizziness or collapse.
Recent results from Australia’s large, long-running food allergy study, HealthNuts, show one in ten one-year-olds have a food allergy, while around six in 100 children have a food allergy at age ten.
A food allergy can present with skin reactions. comzeal images/Shutterstock In Australia, the most common allergy-causing foods include eggs, peanuts, cow’s milk, shellfish (for example, prawn and lobster), fish, tree nuts (for example, walnuts and cashews), soybeans and wheat.
Allergies to foods like eggs, peanuts and cow’s milk often present for the first time in infancy, while allergies to fish and shellfish may be more common later in life. While most children will outgrow their allergies to eggs and milk, allergy to peanuts is more likely to be lifelong.
Findings from HealthNuts showed around three in ten children grew out of their peanut allergy by age six, compared to nine in ten children with an allergy to egg.
Are food allergies becoming more common?
Food allergies seem to have become more common in many countries around the world over recent decades. The exact timing of this increase is not clear, because in most countries food allergies were not well measured 40 or 50 years ago.
We don’t know exactly why food allergies are so common in Australia, or why we’re seeing a rise around the world, despite extensive research.
But possible reasons for rising allergies around the world include changes in the diets of mothers and infants and increasing sanitisation, leading to fewer infections as well as less exposure to “good” bacteria. In Australia, factors such as increasing vitamin D deficiency among infants and high levels of migration to the country could play a role.
In several Australian studies, children born in Australia to parents who were born in Asia have higher rates of food allergies compared to non-Asian children. On the other hand, children who were born in Asia and later migrated to Australia appear to have a lower risk of nut allergies.
Meanwhile, studies have shown that having pet dogs and siblings as a young child may reduce the risk of food allergies. This might be because having pet dogs and siblings increases contact with a range of bacteria and other organisms.
This evidence suggests that both genetics and environment play a role in the development of food allergies.
We also know that infants with eczema are more likely to develop a food allergy, and trials are underway to see whether this link can be broken.
Can I do anything to prevent food allergies in my kids?
One of the questions we are asked most often by parents is “can we do anything to prevent food allergies?”.
We now know introducing peanuts and eggs from around six months of age makes it less likely that an infant will develop an allergy to these foods. The Australasian Society of Clinical Immunology and Allergy introduced guidelines recommending giving common allergy-causing foods including peanut and egg in the first year of life in 2016.
Our research has shown this advice had excellent uptake and may have slowed the rise in food allergies in Australia. There was no increase in peanut allergies between 2007–11 to 2018–19.
Introducing other common allergy-causing foods in the first year of life may also be helpful, although the evidence for this is not as strong compared with peanuts and eggs.
Giving kids peanuts early can reduce the risk of a peanut allergy. Madame-Moustache/Shutterstock What next?
Unfortunately, some infants will develop food allergies even when the relevant foods are introduced in the first year of life. Managing food allergies can be a significant burden for children and families.
Several Australian trials are currently underway testing new strategies to prevent food allergies. A large trial, soon to be completed, is testing whether vitamin D supplements in infants reduce the risk of food allergies.
Another trial is testing whether the amount of eggs and peanuts a mother eats during pregnancy and breastfeeding has an influence on whether or not her baby will develop food allergies.
For most people with food allergies, avoidance of their known allergens remains the standard of care. Oral immunotherapy, which involves gradually increasing amounts of food allergen given under medical supervision, is beginning to be offered in some facilities around Australia. However, current oral immunotherapy methods have potential side effects (including allergic reactions), can involve high time commitment and cost, and don’t cure food allergies.
There is hope on the horizon for new food allergy treatments. Multiple clinical trials are underway around Australia aiming to develop safer and more effective treatments for people with food allergies.
Jennifer Koplin, Group Leader, Childhood Allergy & Epidemiology, The University of Queensland and Desalegn Markos Shifti, Postdoctoral Research Fellow, Child Health Research Centre, Faculty of Medicine, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How an Idaho vaccine advocacy org plans its annual goals
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The start of a new year means many nonprofits and community health workers are busy setting goals and reflecting on what’s worked and what hasn’t. For those engaged in vaccine outreach, it also means reflecting on the tools and tactics that help them communicate better with their communities about why vaccines matter.
Across the country, childhood vaccination rates have declined since the COVID-19 pandemic, resulting in a resurgence of preventable diseases like pertussis.
Also known as whooping cough, pertussis has surged in states like Idaho, said Karen Jachimowski Sharpnack, executive director of the Idaho Immunization Coalition, in a conversation with PGN about the organization’s 2025 priorities.
Sharpnack shared how spikes in infectious respiratory illnesses can create opportunities to listen better and understand the nuances of the communities they serve.
Here’s more of what Sharpnack said.
[Editor’s note: The contents of this interview have been edited for length and clarity.]
PGN: Whooping cough cases are up in your state. Can you share an example of how your organization is responding?
Karen Jachimowski Sharpnack: If you look at Treasure Valley and Northern Idaho, the majority of those cases have been reported, and it’s like five times as much as we had the previous year.
So, two things that the Coalition is doing in response: First, we put out radio public service announcements throughout those particular areas about what whooping cough is, how contagious it is, and what you should do if you think your child or anyone you know has it.
Second, we are contacting every school superintendent, principal, school nurse, with a letter from us at the Coalition [to warn about] the whooping cough outbreaks in schools right now. Here’s what the symptoms are, here’s what you can do, and then here’s how you can protect yourself and your families.
It doesn’t mean the health district wouldn’t do it, or the Department of Health and Welfare can’t do it. But from our standpoint, at least we are bringing an awareness to the schools that this is happening.
PGN: How does your organization decide when outreach is needed? How do you take a pulse of your communities’ vaccine attitudes?
K.J.S.: We consistently hold listening sessions. We do them in English and Spanish if we need to, and we go around—and I’m talking about the southern part of the state—and bring people together.
We’ve done adults, we’ve done teenagers, we’ve done college students, we’ve done seniors, we’ve done all age groups.
So, we’ll bring eight or 10 people together, and we’ll spend a couple of hours with them. We feed them and we also pay them to be there. We say, ‘We want to hear from you about what you’re hearing about vaccines, what your views are if you’re vaccinated.’ Anytime, by the way, they can get up and leave and still get paid.
We want to hear what they’re hearing on the ground. And these sessions are extremely informational. For one, we learn about the misinformation that goes out there, like immediately. And two, we’re able to then focus [on how to respond]. If we’re hearing this, what kind of media campaign do we need to get together?
PGN: How do these listening sessions inform your work?
K.J.S.: So, a couple times a year we also pay a professional poller to do a poll. And when we get those results we check them against our listening sessions. We want to see: Are we on target? Are we ahead?
We just finished putting a one-pager together for legislators, so we’re ready to go with the new [legislative] session. We do this poll every year in August-September to know how Idahoans are feeling about vaccines. We get the results in October, because we’re getting ready for the next year.
We actually poll 19-to-64-year-olds, really honing in on questions like, ‘Do you believe vaccines are safe and effective?’ ‘Do you believe that school vaccination rules should still be in place?’
And what’s pretty cool is that two-thirds of Idahoans still believe vaccines are safe and effective, want to keep school rules in place, and believe that the infrastructure systems that we have in place for our vaccine registry should remain the same. Those are important to hear, so this is really good information that we can pull out and do something with.
PGN: Like what?
K.J.S.: Here’s the bottom line. It takes money to do this work, so you have to be able to say what you are going to do with the results.
Doing a poll costs anywhere from $15,000 to $35,000. This is an expensive investment, but we know that the polling is so important to us, along with the time that I have my staff go out and do the listening sessions and get feedback.
We take those results to educate, to talk to our legislators, and advocate for vaccines. We actually do these high-level media campaigns around the state. So, we are actually doing something with the polling. We’re not just sharing the results out.
And then we actually ask, what can we do to make a change? What are we hearing that we need to focus on?
That’s why it’s really important, because we are actually pushing this out for 2025. We know where we’re going in 2025 programmatically with marketing, and we know where we’re going with advocacy work.
We’re not guessing. We’re actually listening to people. And then we’re making really concrete decisions on how we’re going to move the organization forward to be able to help our communities.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: