Tribulus Terrestris For Testosterone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
(Clinical) Trials and Tribul-ations
In the category of supplements that have enjoyed use as aphrodisiacs, Tribulus terrestris (also called caltrop, goat’s head, gokshura, or puncture vine) has a long history, having seen wide use in both Traditional Chinese Medicine and in Ayurveda.
It’s been used for other purposes too, and has been considered a “general wellness” plant.
So, what does the science say?
Good news: very conclusive evidence!
Bad news: the conclusion is not favorable…
Scientists are known for their careful use of clinical language, and it’s very rare for a study/review to claim something as proven (scientists leave journalists to do that part), and in this case, when it comes to Tribulus’s usefulness as a testosterone-enhancing libido-boosting supplement…
❝analysis of empirical evidence from a comprehensive review of available literature proved this hypothesis wrong❞
Strong words! You can read it in full here; they do make some concessions along the way (e.g. mentioning unclear or contradictory findings, suggesting that it may have some effect, but by an as-yet unknown mechanism if it does—although some potential effect on nitric oxide levels has been hypothesized, which is reasonable if so, as NO does feature in arousal-signalling), but the general conclusion is “no, this doesn’t have androgen-enhancing properties”:
Pro-sexual and androgen enhancing effects of Tribulus terrestris L.: Fact or Fiction
That’s a review though, what about taking a look at a representative RCT? Here we go:
❝Tribulus terrestris was not more effective than placebo on improving symptoms of erectile dysfunction or serum total testosterone❞
As a performance-enhancer in sport
We’ll be brief here: it doesn’t seem to work and it may not be safe:
Insights into Supplements with Tribulus Terrestris used by Athletes
From sport, into general wellness?
Finally, a study that finds it may be useful for something!
❝Overall, participants supplemented with TT displayed significant improvements in lipid profile. Inflammatory and hematological biomarkers showed moderate beneficial effects with no significant changes on renal biomarkers. No positive effects were observed on the immune system response. Additionally, no TT-induced toxicity was reported.
In conclusion, there was no clear evidence of the beneficial effects of TT supplementation on muscle damage markers and hormonal behavior.❞
About those lipids…
Animal studies have shown that it may not only improve lipid profiles, but also may partially repair the endothelial dysfunction resulting from hyperlipidemia:
Want to try some?
In the unlikely event that today’s research review has inspired you with an urge to try Tribulus terrestris, here’s an example product on Amazon
If on the other hand you’d like to actually increase testosterone levels, then we suggest:
Topping Up Testosterone? ← a previous main feature did earlier this year
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Oral vaccines could provide relief for people who suffer regular UTIs. Here’s how they work
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a recent TikTok video, Australian media personality Abbie Chatfield shared she was starting a vaccine to protect against urinary tract infections (UTIs).
Huge news for the UTI girlies. I am starting a UTI vaccine tonight for the first time.
Chatfield suffers from recurrent UTIs and has turned to the Uromune vaccine, an emerging option for those seeking relief beyond antibiotics.
But Uromune is not a traditional vaccine injected to your arm. So what is it and how does it work?
9nong/Shutterstock First, what are UTIs?
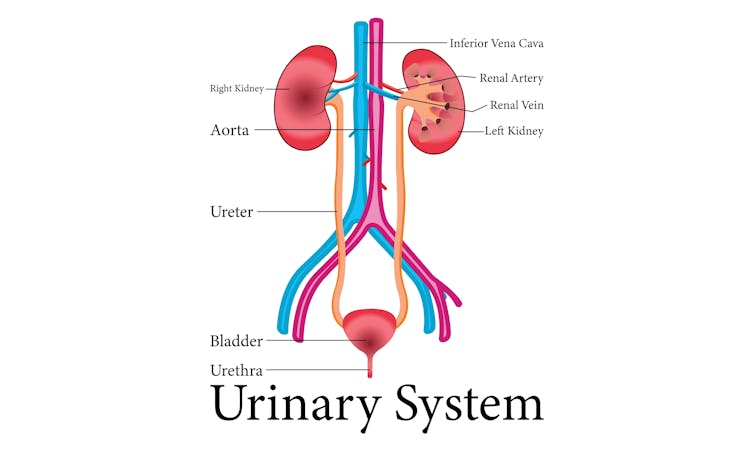
UTIs are caused by bacteria entering the urinary system. This system includes the kidneys, bladder, ureters (thin tubes connecting the kidneys to the bladder), and the urethra (the tube through which urine leaves the body).
The most common culprit is Escherichia coli (E. coli), a type of bacteria normally found in the intestines.
While most types of E. coli are harmless in the gut, it can cause infection if it enters the urinary tract. UTIs are particularly prevalent in women due to their shorter urethras, which make it easier for bacteria to reach the bladder.
Roughly 50% of women will experience at least one UTI in their lifetime, and up to half of those will have a recurrence within six months.
UTIs are caused by bacteria enterning the urinary system. oxo7051/Shutterstock The symptoms of a UTI typically include a burning sensation when you wee, frequent urges to go even when the bladder is empty, cloudy or strong-smelling urine, and pain or discomfort in the lower abdomen or back. If left untreated, a UTI can escalate into a kidney infection, which can require more intensive treatment.
While antibiotics are the go-to treatment for UTIs, the rise of antibiotic resistance and the fact many people experience frequent reinfections has sparked more interest in preventive options, including vaccines.
What is Uromune?
Uromune is a bit different to traditional vaccines that are injected into the muscle. It’s a sublingual spray, which means you spray it under your tongue. Uromune is generally used daily for three months.
It contains inactivated forms of four bacteria that are responsible for most UTIs, including E. coli. By introducing these bacteria in a controlled way, it helps your immune system learn to recognise and fight them off before they cause an infection. It can be classified as an immunotherapy.
A recent study involving 1,104 women found the Uromune vaccine was 91.7% effective at reducing recurrent UTIs after three months, with effectiveness dropping to 57.6% after 12 months.
These results suggest Uromune could provide significant (though time-limited) relief for women dealing with frequent UTIs, however peer-reviewed research remains limited.
Any side effects of Uromune are usually mild and may include dry mouth, slight stomach discomfort, and nausea. These side effects typically go away on their own and very few people stop treatment because of them. In rare cases, some people may experience an allergic reaction.
How can I access it?
In Australia, Uromune has not received full approval from the Therapeutic Goods Administration (TGA), and so it’s not something you can just go and pick up from the pharmacy.
However, Uromune can be accessed via the TGA’s Special Access Scheme or the Authorised Prescriber pathway. This means a GP or specialist can apply for approval to prescribe Uromune for patients with recurrent UTIs. Once the patient has a form from their doctor documenting this approval, they can order the vaccine directly from the manufacturer.
Antibiotics are the go-to treatment for UTIs – but scientists are looking at options to prevent them in the first place. Photoroyalty/Shutterstock Uromune is not covered under the Pharmaceutical Benefits Scheme, meaning patients must cover the full cost out-of-pocket. The cost of a treatment program is around A$320.
Uromune is similarly available through special access programs in places like the United Kingdom and Europe.
Other options in the pipeline
In addition to Uromune, scientists are exploring other promising UTI vaccines.
Uro-Vaxom is an established immunomodulator, a substance that helps regulate or modify the immune system’s response to bacteria. It’s derived from E. coli proteins and has shown success in reducing UTI recurrences in several studies. Uro-Vaxom is typically prescribed as a daily oral capsule taken for 90 days.
FimCH, another vaccine in development, targets something called the adhesin protein that helps E. coli attach to urinary tract cells. FimCH is typically administered through an injection and early clinical trials have shown promising results.
Meanwhile, StroVac, which is already approved in Germany, contains inactivated strains of bacteria such as E. coli and provides protection for up to 12 months, requiring a booster dose after that. This injection works by stimulating the immune system in the bladder, offering temporary protection against recurrent infections.
These vaccines show promise, but challenges like achieving long-term immunity remain. Research is ongoing to improve these options.
No magic bullet, but there’s reason for optimism
While vaccines such as Uromune may not be an accessible or perfect solution for everyone, they offer real hope for people tired of recurring UTIs and endless rounds of antibiotics.
Although the road to long-term relief might still be a bit bumpy, it’s exciting to see innovative treatments like these giving people more options to take control of their health.
Iris Lim, Assistant Professor in Biomedical Science, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Wholesome Threesome Protein Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This soup has two protein– and fiber-rich pseudo-grains, one real wholegrain, and nutrient-dense cashews for yet even more protein, and all of the above are full of many great vitamins and minerals. All in all, a well-balanced and highly-nutritious light meal!
You will need
- ⅓ cup quinoa
- ⅓ cup green lentils
- ⅓ cup wholegrain rice
- 5 cups low-sodium vegetable stock (ideally you made this yourself from offcuts of vegetables, but failing that, low-sodium stock cubes can be bought in most large supermarkets)
- ¼ cup cashews
- 1 tbsp dried thyme
- 1 tbsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
Optional topping:
- ⅓ cup pine nuts
- ⅓ cup finely chopped fresh mint leaves
- 2 tbsp coconut oil
Method
(we suggest you read everything at least once before doing anything)
1) Rinse the quinoa, lentils, and rice.
2) Boil 4 cups of the stock and add the grains and seasonings (MSG/salt, pepper, thyme); simmer for about 25 minutes.
3) Blend the cashews with the other cup of vegetable stock, until smooth. Add the cashew mixture to the soup, stirring it in, and allow to simmer for another 5 minutes.
4) Heat the coconut oil in a skillet and add the pine nuts, stirring until they are golden brown.
5) Serve the soup into bowls, adding the mint and pine nuts to each.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Give Us This Day Our Daily Dozen
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Why You Should Diversify Your Nuts!
Take care!
Share This Post
-
The Drug & Supplement Combo That Reverses Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So far, its effects have been dramatic (in a good way) in mice; human trials are now underway.
How does it work?
It builds from previous work, in which a Japanese research team created an “anti-aging vaccine”, that responded to a problem more specific than aging as a whole, namely atherosclerosis.
They found that a certain* protein was upregulated (i.e., it was made at a greater rate resulting in greater quantities) in patients (mouse and human alike) with atherosclerosis. So, they immunized the mice against that protein, and long story short, everything improved for them, from their atherosclerosis to general markers of aging—including growing back fur that had been lost due to age-related balding (just like in humans). They also lived longer, as is to be expected of a mouse who is now biologically younger.
*To avoid being mysterious: it was glycoprotein nonmetastatic melanoma protein B, known to its friends as GPNMB.
You may be wondering: how can one be immunized against a protein? If so, do bear in mind, a virus is also a protein. In this case, they developed an RNA vaccine, that works in a similar way to the COVID vaccines we all know and love (albeit with a different target).
You can read about this in abundant detail here: Senolytic vaccination improves normal and pathological age-related phenotypes and increases lifespan in progeroid mice
Hot on the heels of that, new approaches were found, including…
The combination
We’ll not keep you waiting; the combination is dasatinib plus quercetin, or else fisetin alone.
It’s about killing senescent (aging) “zombie cells” while sparing healthy cells, which that drug (dasatinib) and those supplements (quercetin and fisetin) do.
The researchers noted:
❝Senescent cells are resistant to apoptosis, which is governed through the upregulation of senescent cell anti-apoptotic pathways (SCAPs). Compounds were subsequently identified that disrupted the SCAPs, inducing death of senescent cells while leaving healthy cells unaffected. Forty-six potential senolytic agents were discovered through this process. To advance translational efforts, the majority of research has focused on agents with known safety profiles and limited off-target effects (Kirkland and Tchkonia, 2020).
The best characterized senolytic agents are dasatinib, a tyrosine kinase inhibitor approved for use in humans for cancer treatment, and quercetin, a naturally occurring plant flavonoid. The agents have a synergistic effect, making their combination more potent for senescent cell clearance (Zhu et al., 2015). As senescent cells do not divide and accumulate over a period of weeks, they can be administered using an intermittent approach, which further serves to reduce the risk of side effects (Kirkland and Tchkonia, 2020).
In preclinical trials, the combination of dasatinib and quercetin (D + Q) have been found to alleviate numerous chronic medical conditions including vascular stiffness, osteoporosis, frailty, and hepatic stenosis❞
Source: A geroscience motivated approach to treat Alzheimer’s disease: Senolytics move to clinical trials
As to how they expanded on this research:
❝In our study, oral D + Q were intermittently administered to tau transgenic mice with late-stage pathology (approximated to a 70-year-old human with advanced AD) (Musi et al., 2018). The treatment effectively reduced cellular senescence and associated senescence-associated secretory phenotype incidence. The 35 % reduction in neurofibrillary tangles was accompanied by enhanced neuron density, decreased ventricular enlargement, diminished tau accumulation, and restoration of aberrant cerebral blood flow. A subsequent preclinical study validated the findings, reporting that intermittently administered D + Q cleared senescent cells in the central nervous system, reduced amyloid-β plaques, attenuated neuroinflammation, and enhanced cognition❞
Source: Ibid.
And now taking it to humans:
❝The first clinical trial of D + Q for early-stage Alzheimer’s Disease (AD) has completed enrollment (Gonzales et al., 2021). The primary aim of the open-label pilot study was to examine the central nervous system penetrance of D and Q in a small sample of older adults with early-stage AD (NCT04063124). In addition, two placebo-controlled trials of D + Q for neurodegenerative disease are underway (NCT04685590 and NCT04785300).
One of the trials in development is a multi-site, double-blind, randomized, placebo-controlled study of senolytic therapy in older adults with amnestic mild cognitive impairment (MCI) or early-stage dementia (Clinical Dementia Rating Scale (CDR) Global 0.5–1) due to AD (elevated CSF total tau/Aβ42 ratio).
The treatment regimen will consist of 12-weeks of intermittently administered oral D + Q.❞
Source: Ibid.
The study is actually completed now, but its results are not yet published (again, at time of writing). Which means: they have the data, and now they’re writing the paper.
We look forward to providing an update about that, when the paper is published!
In the meantime…
Dasatinib is a drug usually prescribed to people with certain kinds of leukemia, and suffice it to say, it’s prescription-only. And unlike drugs that are often prescribed off-label (such as metformin for weight loss), getting your doctor to prescribe you an anticancer drug is unlikely unless you have the cancer in question.
You may be wondering: how is an anticancer drug helpful against aging? And the answer is that cancer and aging are very interrelated, and both have to do with “these old cells just won’t die, and are using the resources needed for young healthy cells”. So in both cases, killing those “zombie cells” while sparing healthy ones, is what’s needed. However, your doctor will probably not buy that as a reason to prescribe you a drug that is technically chemotherapy.
Quercetin, on the other hand, is a readily-available supplement, as is fisetin, and both have glowing (in a good way) safety profiles.
Want to know more?
You can read more about each of quercetin and fisetin (including how to get them), here:
Enjoy!
Share This Post
Related Posts
-
Cross That Bridge – by Samuel J. Lucas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Books of this genre usually have several chapters of fluff before getting to the point. You know the sort:
- Let me tell you about some cherry-picked celebrity stories that overlook survivorship bias
- Let me tell you my life story, the bad parts
- My life story continued, the good parts now
- What this book can do for you, an imaginative pep talk that keeps circling back to me
…then there will be two or three chapters of the actual advertised content, and then a closing chapter that’s another pep talk.
This book, in contrast, throws that out of the window. Instead, Lucas provides a ground-up structure… within which, he makes a point of giving value in each section:
- exercises
- summaries
- actionable advice
For those who like outlines, lists, and overviews (as we do!), this is perfect. There are also plenty of exercises to do, so for those who like exercises, this book will be great too!
Caveat: occasionally, the book’s actionable advices are direct but unclear, for example:
- Use the potential and power of tea, to solve problems
Context: there was no context. This was a bullet-pointed item, with no explanation. It was not a callback to anything earlier; this is the first (and only) reference to tea.
However! The book as a whole is a treasure trove of genuine tips, tools, and voice-of-experience wisdom. Occasional comments may leave you scratching your head, but if you take value from the rest, then the book was already more than worth its while.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pasteurization: What It Does And Doesn’t Do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pasteurization’s Effect On Risks & Nutrients
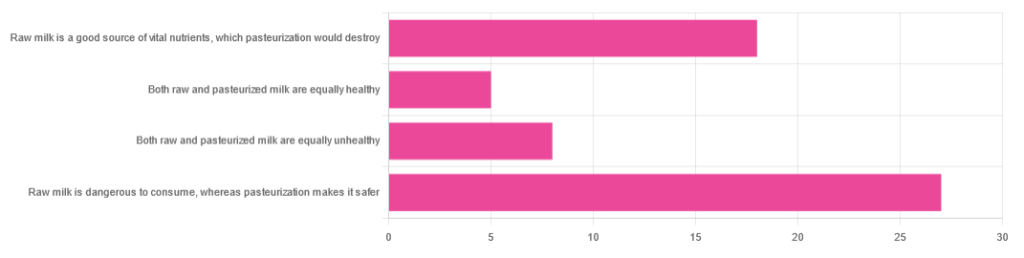
In Wednesday’s newsletter, we asked you for your health-related opinions of raw (cow’s) milk, and got the above-depicted, below-described, set of responses:
- About 47% said “raw milk is dangerous to consume, whereas pasteurization makes it safer”
- About 31% said “raw milk is a good source of vital nutrients which pasteurization would destroy”
- About 14% said “both raw milk and pasteurized milk are equally unhealthy”
- About 9% said “both raw milk and pasteurized milk are equally healthy”
Quite polarizing! So, what does the science say?
“Raw milk is dangerous to consume, whereas pasteurization makes it safer: True or False?”
True! Coincidentally, the 47% who voted for this are mirrored by the 47% of the general US population in a similar poll, deciding between the options of whether raw milk is less safe to drink (47%), just as safe to drink (15%), safer to drink (9%), or not sure (30%):
Public Fails to Appreciate Risk of Consuming Raw Milk, Survey Finds
As for what those risks are, by the way, unpasteurized dairy products are estimated to cause 840x more illness and 45x more hospitalizations than pasteurized products.
This is because unpasteurized milk can (and often does) contain E. coli, Listeria, Salmonella, Cryptosporidium, and other such unpleasantries, which pasteurization kills.
Source for both of the above claims:
(we know the title sounds vague, but all this information is easily visible in the abstract, specifically, the first two paragraphs)
Raw milk is a good source of vital nutrients which pasteurization would destroy: True or False?
False! Whether it’s a “good” source can be debated depending on other factors (e.g., if we considered milk’s inflammatory qualities against its positive nutritional content), but it’s undeniably a rich source. However, pasteurization doesn’t destroy or damage those nutrients.
Incidentally, in the same survey we linked up top, 16% of the general US public believed that pasteurization destroys nutrients, while 41% were not sure (and 43% knew that it doesn’t).
Note: for our confidence here, we are skipping over studies published by, for example, dairy farming lobbies and so forth. Those do agree, by the way, but nevertheless we like sources to be as unbiased as possible. The FDA, which is not completely unbiased, has produced a good list of references for this, about half of which we would consider biased, and half unbiased; the clue is generally in the journal names. For example, Food Chemistry and the Journal of Food Science and Journal of Nutrition are probably less biased than the International Dairy Association and the Journal of Dairy Science:
FDA | Raw Milk Misconceptions and the Danger of Raw Milk Consumption
this page covers a lot of other myths too, more than we have room to “bust” here, but it’s very interesting reading and we recommend to check it out!
Notably, we also weren’t able to find any refutation by counterexample on PubMed, with the very slight exception that some studies sometimes found that in the case of milks that were of low quality, pasteurization can reduce the vitamin E content while increasing the vitamin A content. For most milks however, no significant change was found, and in all cases we looked at, B-vitamins were comparable and vitamin D, popularly touted as a benefit of cow’s milk, is actually added later in any case. And, importantly, because this is a common argument, no change in lipid profiles appears to be findable either.
In science, when something has been well-studied and there aren’t clear refutations by counterexample, and the weight of evidence is clearly very much tipped into one camp, that usually means that camp has it right.
Milk generally is good/bad for the health: True or False?
True or False, depending on what we want to look at. It’s definitely not good for inflammation, but the whole it seems to be cancer-neutral and only increases heart disease risk very slightly:
- Keep Inflammation At Bay ← short version is milk is bad, fermented milk products are fine in moderation
- Is Dairy Scary? ← short version is that milk is neither good nor terrible; fermented dairy products however are health-positive in numerous ways when consumed in moderation
You may be wondering…
…how this goes for the safety of dairy products when it comes to the bird flu currently affecting dairy cows, so:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Vegetarian & Vegan Diets: Good Or Bad For Brain Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s well-established that most people should eat more plants, and generally speaking, less meat. But what about abstaining from meat completely? And what about abstaining from all animal products?
For a more general overview (rather than specifically brain health), check out: Do We Need Animal Products To Be Healthy?
Now, about brains…
Before Homo sapiens was a thing, our precursors such as Homo habilis developed language (thus: greatly enhanced collaborative teamwork) and cooking, resulting in Homo ergaster (who came approximately next in line, give or take taxonomical quibbles) having twice the cranial capacity, generally attributed to being able to acquire and—where appropriate—cook calorie-dense food, which included meat, and also tubers that can’t be safely eaten raw. It’s estimated (based on forensic examination of tooth wear, mineralization, microdeposits of various kinds, etc) that our consumption of animal products in that era was around 10% of our diet (fluctuating by region, of course), but it likely was an important one.
By the time we got to Homo erectus, our skulls (including our cranial cavities, and thus it is presumed, our brains) were actually larger than in Homo sapiens. You may be wondering about Homo neanderthalensis; our cousins (or in some cases, ancestors—but that is beyond the scope of today’s article) also had larger cranial cavities than us, and certainly enjoyed comparatively advanced culture, arts, religion, etc.
Fast-forward to the present day. Nothing is going to meaningfully change our skull size, as individuals. Brain size? Well, keep hydrated or it’ll shrink. Don’t overhydrate or it’ll swell. Neuroplasticity means we can increase (or lose) volume in specific areas of the brain, according to what we do most of. For example, if you were to scan this writer’s brain, you’d probably find overdevelopment in the various areas pertaining to language and memory, as that’s been “my thing” for as long as I can remember (which is a long way). See also: An Underrated Tool Against Alzheimer’s
The impact of diet in the modern day
Unlike our distant ancestors, if we want a high-calorie snack we can buy some nuts from the supermarket, and if anything, this can be a problem (as many people’s go-to high-calorie snack may be a lot less healthy than that), and in turn cause problems for the brain, because too many pizzas, cheeseburgers, tater tots, and so forth cause chronic inflammation, and thus, neuroinflammation.
See also: 6 Worst Foods That Cause Dementia
So much for “calories for the brain”. Yes, the brain definitely needs calories (it expends a very large portion of our daily calorie intake), but you can have too much of a good thing.
In any case, the brain needs more than just calories!
For example, you may remember the “6 Pillars Of Nutritional Psychiatry”, which are:
- Be whole; eat whole
- Eat the rainbow
- The greener, the better
- Tap into your body intelligence
- Consistency & balance are key
- Avoid anxiety-triggering foods
For more on all of those, see Dr. Uma Naidoo’s 6 Pillars Of Nutritional Psychiatry ← She’s a Harvard-trained psychiatrist, professional chef graduating with her culinary school’s most coveted award, and a trained nutritionist. Between those three qualifications, she knows her stuff when it comes to the niche that is nutritional psychiatry.
When it comes to any potential nutritional deficiencies of a vegetarian or vegan diet, it’s a matter of planning.
Properly planned vegetarian diets are rich in essential nutrients like carbohydrates, fiber, magnesium, potassium, folate, vitamins C and E, and an abundance of phytochemicals, which support brain health (and overall health too, but today is about brain health).
However, if not well-planned, they can indeed lack certain nutrients such as vitamin B12, iron, and omega-3 fatty acids, which are critical for brain function.
In essence, there’s a difference between a “whole foods plant-based diet” and junk food that just happens to be vegetarian or vegan.
Vitamin B12 is usually supplemented by vegans, but it can also be enjoyed from nutritional yeast used in cooking (it adds a cheesy flavor to dishes for which that’d be appropriate).
Iron is a fascinating beast, because while everyone thinks of red meat (which is indeed rich in iron), not only are there good plant-based sources of iron, but there are important considerations when it comes to bioavailability differences between heme and non-heme iron. In few words, heme iron (from blood etc) is more bioavailable by 1.8x, but all iron, including non-heme iron (from beans, greens, etc) can have its bioavailability multiplied by 5x just by having it with vitamin C:
Avoiding Anemia (More Than Just “Get More Iron”)
Omega-3 fatty acids, for vegetarians that mostly means eggs. See: Eggs: All Things In Moderation?
For vegans, we must look to nuts and seeds, for the most part. Or supplement—many omega 3 supplements are vegan, made from algae, or seaweed (that in turn is composed partially or entirely of algae):
So really, it comes down to “make sure you still get these things”, and once you’re used to it, it’s easy.
For those who prefer to keep some meat in their diet
Our summary in our top-linked article (Do We Need Animal Products To Be Healthy?) concluded:
- Most of us can live healthily and happily on just plants if we so choose.
- Some people cannot, and will require varying kinds (and quantities) of animal products.
- As for red and/or processed meats, we’re not the boss of you, but from a health perspective, the science is clear: unless you have a circumstance that really necessitates it, just don’t.
- Same goes for pork, which isn’t red and may not be processed, but metabolically it’s associated with the same problems.
- The jury is out on poultry, but it strongly appears to be optional, healthwise, without making much of a difference either way
- Fish is roundly considered healthful in moderation. Enjoy it if you want, don’t if you don’t.
And the paper from which we’ve largely been working from today included such comments as:
❝ Evidence suggests that vegan and vegetarian diets, when well planned, can be rich in phytonutrients and antioxidants, which have been associated with lower levels of inflammatory markers, such as C-reactive protein (CRP) and interleukin-6 (IL-6). These findings indicate a potential role in reducing systemic inflammation and oxidative stress, both of which are linked to neurodegenerative diseases.
However, deficiencies in critical nutrients such as vitamin B12, DHA, EPA, and iron have been consistently associated with an increased risk of cognitive decline, mood disturbances, and neurodegenerative disorders.
While plant-based diets provide anti-inflammatory and antioxidant benefits, their neurological implications depend on nutrient adequacy. Proper planning, supplementation, and food preparation techniques are essential to mitigate risks and enhance cognitive health.❞
Source: Impact of Vegan and Vegetarian Diets on Neurological Health: A Critical Review ← you can see that they also cover the same nutrients that we do
One final note, not discussed above
We often say “what’s good for your heart is good for your brain”, because the former feeds the latter (with oxygen and nutrients) and assists in cleanup (of detritus that otherwise brings about cognitive decline).
So with that in mind…
What Matters Most For Your Heart? ← hint: it’s fiber. So whether you eat animal products or not, please do eat plenty of plants!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: