Thinner Leaner Stronger – by Michael Matthews
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, the elephant in the training room: this book does assume that you want to be thinner, leaner, and stronger. This is the companion book, written for women, to “Bigger, Stronger, Leaner”, which was written for men. Statistically, these assumptions are reasonable, even if the generalizations are imperfect. Also, this reviewer has a gripe with anything selling “thinner”. Leaner was already sufficient, and “stronger” is the key element here, so “thinner” is just marketing, and marketing something that’s often not unhealthy, to sell a book that’s actually full of good advice for building a healthy body.
In other words: don’t judge a book by the cover, however eyeroll-worthy it may be.
The book is broadly aimed at middle-aged readers, but boasts equal worth for young and old alike. If there’s something Matthews knows how to do well in his writing, it’s hedging his bets.
As for what’s in the book: it’s diet and exercise advice, aimed at long-term implementation (i.e. not a crash course, but a lifestyle change), for maximum body composition change results while not doing anything silly (like many extreme short-term courses do) and not compromising other aspects of one’s health, while also not taking up an inordinate amount of time.
The dietary advice is sensible, broadly consistent with what we’d advise here, and/but if you want to maximise your body composition change results, you’re going to need a pocket calculator (or be better than this writer is at mental arithmetic).
The exercise advice is detailed, and a lot more specific than “lift things”; there are programs of specifically how many sets and reps and so forth, and when to increase the weights and when not to.
A strength of this book is that it explains why all those numbers are what they are, instead of just expecting the reader to take on faith that the best for a given exercise is (for example) 3 sets of 8–10 reps of 70–75% of one’s single-rep max for that exercise. Because without the explanation, those numbers would seem very arbitrary indeed, and that wouldn’t help anyone stick with the program. And so on, for any advice he gives.
The style is… A little flashy for this reader’s taste, a little salesy (and yes he does try to upsell to his personal coaching, but really, anything you need is in the book already), but when it comes down to it, all that gym-boy bravado doesn’t take away from the fact his advice is sound and helpful.
Bottom line: if you would like your body to be the three things mentioned in the title, this book can certainly help you get there.
Click here to check out Thinner Leaner Stronger, and become thinner, leaner, stronger!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fruit Is Healthy; Juice Isn’t (Here’s Why)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Biochemist and “Glucose Goddess” Jessie Inchauspé wants us to understand the difference:
Stripped!
A glass of orange juice contains 22 grams of sugar (about six sugar cubes), nearly as much as a can of soda (27 grams).
Orange juice is widely perceived as healthy due to vitamin content—but if you add vitamins to soda, it won’t make it healthy, because the main health effect is still the sugar, leading to glucose spikes and many resultant health risks. The positive image of fruit juice is mainly from industry marketing.
In reality, Inchauspé advises, fruit juice should be treated like a dessert—consumed for pleasure, not health benefits.
But why, then, is fruit healthy if fruit juice is unhealthy? Isn’t the sugar there too?
Whole fruit contains plenty of fiber, which slows sugar absorption and prevents glucose spikes. Juicing strips it of its fiber, leaving water and sugar.
The American Heart Association suggests a sugar limit: 25g/day for women, 36g/day for men. One glass of orange juice nearly meets the daily limit for women. If that’s how you want to “spend” your daily sugar allowance, go for it, but do so consciously, by choice, knowing that the allowance is now “spent”.
In contrast, if you eat whole fruit, that basically “doesn’t count” for sugar purposes. The sugar is there, but the fiber more than offsets it, making whole fruit very good for blood sugars.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Share This Post
-
Rutin For Your Circulation & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rutin is a bioflavonoid so potent it’s also been called “vitamin P”, and it’s found most abundantly in buckwheat, as well appearing in citrus and some stone fruits (apricots, plums, etc) as well as figs and apples—it’s also found in asparagus, and green and black tea.
So, what does it do?
Quite a lot: The Pharmacological Potential of Rutin
There’s much more there than we have room to cover here, but we’ll pick out a few salient properties to focus on.
First, a word of warning
A lot of the extant science for rutin is in non-human animals. Sometimes, what works for non-human animals doesn’t work for humans; we saw a clear example of this here:
Conjugated Linoleic Acid For Weight Loss?
…in which CLA worked for weight loss in mice, hamsters, chickens, and pigs, but stubbornly not humans.
The state of affairs with the science for rutin isn’t nearly that bad and there are human studies showing efficacy, and indeed, rutin is given to (human) patients with capillary fragility, varicose veins, bruising, or hemorrhoids, for example:
So, we’ll try to give you humans-only sources so far as we can today!
Improving blood flow
Rutin does improve various blood metrics, including various kinds of blood pressure (diastolic, systolic, mean arterial, pulse) and heart rate. At least, it did in humans with type 2 diabetes, and we may reasonably assume these results may be extrapolated to humans without type 2 (or any other) diabetes:
As you may gather from the title, it did also significantly improve serum antioxidant levels, and quality of life (which latter was categorized as: emotional limitations, energy and freshness, mental health, social performance, and general health).
We couldn’t find studies for cardioprotective effects in humans (and of course those couldn’t be RCTs, they’d have to be observational studies, because no ethics board allows inducing heart attacks in humans for the sake of science), but here’s a study using rats (with and without diabetes), showing proof of principle at least:
Anti-Alzheimer’s potential
As ever, a good general rule of thumb is “what’s good for the blood is good for the brain”, and that’s true in this case too.
The title says it all, here:
In case that is not clear: everything in that title after the word “inhibits” is bad for the brain and is implicated in Alzheimer’s disease pathogenesis and progression; in other words, rutin is good against all those bad, Alzheimer’s-favoring things.
Other neuroprotective activity
You may remember from the above-linked research that it helps protect against damage caused by Advanced Glycation End-products (AGEs) (the golden-brown stuff that appears as a result of dry-cooking proteins and fats); it also helps against damage caused by acrylamide (the golden-brown stuff that appears as a result of dry-cooking starches).
Note: in both cases “dry-cooking” includes cooking with oil; it simply means “without water”.
Again, this was a rat study, because no ethics board would have let the researchers fry human brains for science.
Want to try some?
As well as simply enjoying the fruits and vegetables that contain it, it is possible to take a rutin supplement.
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
I can’t afford olive oil. What else can I use?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you buy your olive oil in bulk, you’ve likely been in for a shock in recent weeks. Major supermarkets have been selling olive oil for up to A$65 for a four-litre tin, and up to $26 for a 750 millilitre bottle.
We’ve been hearing about the health benefits of olive oil for years. And many of us are adding it to salads, or baking and frying with it.
But during a cost-of-living crisis, these high prices can put olive oil out of reach.
Let’s take a look at why olive oil is in demand, why it’s so expensive right now, and what to do until prices come down.
Joyisjoyful/Shutterstock Remind me, why is olive oil so good for you?
Including olive oil in your diet can reduce your risk of developing type 2 diabetes and improve heart health through more favourable blood pressure, inflammation and cholesterol levels.
This is largely because olive oil is high in monounsaturated fatty acids and polyphenols (antioxidants).
Some researchers have suggested you can get these benefits from consuming up to 20 grams a day. That’s equivalent to about five teaspoons of olive oil.
Why is olive oil so expensive right now?
A European heatwave and drought have limited Spanish and Italian producers’ ability to supply olive oil to international markets, including Australia.
This has been coupled with an unusually cold and short growing season for Australian olive oil suppliers.
The lower-than-usual production and supply of olive oil, together with heightened demand from shoppers, means prices have gone up.
We’ve seen unfavourable growing conditions in Europe and Australia. KaMay/Shutterstock How can I make my olive oil go further?
Many households buy olive oil in large quantities because it is cheaper per litre. So, if you have some still in stock, you can make it go further by:
- storing it correctly – make sure the lid is on tightly and it’s kept in a cool, dark place, such as a pantry or cabinet. If stored this way, olive oil can typically last 12–18 months
- using a spray – sprays distribute oil more evenly than pourers, using less olive oil overall. You could buy a spray bottle to fill from a large tin, as needed
- straining or freezing it – if you have leftover olive oil after frying, strain it and reuse it for other fried dishes. You could also freeze this used oil in an airtight container, then thaw and fry with it later, without affecting the oil’s taste and other characteristics. But for dressings, only use fresh oil.
I’ve run out of olive oil. What else can I use?
Here are some healthy and cheaper alternatives to olive oil:
- canola oil is a good alternative for frying. It’s relatively low in saturated fat so is generally considered healthy. Like olive oil, it is high in healthy monounsaturated fats. Cost? Up to $6 for a 750mL bottle (home brand is about half the price)
- sunflower oil is a great alternative to use on salads or for frying. It has a mild flavour that does not overwhelm other ingredients. Some studies suggest using sunflower oil may help reduce your risk of heart disease by lowering LDL (bad) cholesterol and raising HDL (good) cholesterol. Cost? Up to $6.50 for a 750mL bottle (again, home brand is about half the price)
- sesame oil has a nutty flavour. It’s good for Asian dressings, and frying. Light sesame oil is typically used as a neutral cooking oil, while the toasted type is used to flavour sauces. Sesame oil is high in antioxidants and has some anti-inflammatory properties. Sesame oil is generally sold in smaller bottles than canola or sunflower oil. Cost? Up to $5 for a 150mL bottle.
There are plenty of alternative oils you can use in salads or for frying. narai chal/Shutterstock How can I use less oil, generally?
Using less oil in your cooking could keep your meals healthy. Here are some alternatives and cooking techniques:
- use alternatives for baking – unless you are making an olive oil cake, if your recipe calls for a large quantity of oil, try using an alternative such as apple sauce, Greek yoghurt or mashed banana
- use non-stick cookware – using high-quality, non-stick pots and pans reduces the need for oil when cooking, or means you don’t need oil at all
- steam instead – steam vegetables, fish and poultry to retain nutrients and moisture without adding oil
- bake or roast – potatoes, vegetables or chicken can be baked or roasted rather than fried. You can still achieve crispy textures without needing excessive oil
- grill – the natural fats in meat and vegetables can help keep ingredients moist, without using oil
- use stock – instead of sautéing vegetables in oil, try using vegetable broth or stock to add flavour
- try vinegar or citrus – use vinegar or citrus juice (such as lemon or lime) to add flavour to salads, marinades and sauces without relying on oil
- use natural moisture – use the natural moisture in ingredients such as tomatoes, onions and mushrooms to cook dishes without adding extra oil. They release moisture as they cook, helping to prevent sticking.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Better With Age – by Dr. Alan Castel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one isn’t about the biology of aging, so much as (as the subtitle promises) the psychology of it.
Dr. Castel first covers the grounds of what “successful aging” is, and the benefits that can be expected from doing it right. Spoiler, it’s not just “reduced decline”, there are numerous things that actually get better, too.
We also learn how our memory works differently—it can be worse, of course, but it can also be just different, in a way that tends to tie in with vastness of the accumulated knowledge over the years, allowing for easiest access to the things the brain thinks are most important—ranging from expertise in a certain field, to life-experience “wisdom”.
There’s a lot of advice that’s mostly not going to be anything new to regular readers of 10almonds, in terms of staying sharp with an active lifestyle and a well-nourished brain.
The style is very soft pop-science; there are citations dotted throughout, but mostly this is more of a “curl up with a book” book, not a textbook.
In the category of subjective criticism, it can be a little repetitive (but for those who like repetition for ease of learning, you will love this), and his name-dropping habit gets quite eyeroll-worthy quite quickly.
Bottom line: if you’d like to learn about the very many ways in which “over the hill” is simply defeatist pessimism, then this book can help you to ensure you do better.
Click here to check out Better With Age, and get better with age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
This Naked Mind – by Annie Grace
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all read about the many, many, dangers of drinking. We’ve also probably all read about how to make the change to not drinking. Put things out of sight, tell your friends, have this rule, have this excuse (for not drinking) ready to give to people who challenge you, consider a support group, and so on.
What Annie Grace offers in this #1 bestseller is different:
A blend of mostly psychology and sociology, to examine the “liminal thinking” stages that funnel us to drink in the first place… and where that leads, and how to clamber back out of the pitcher plant we weren’t necessarily aware we were sliding into.
While she kicks off citing Jung, from a psychological perspective more of this book is CBTish, as it pertains a lot to examining the process of:
- belief—held and defended, based on the…
- conclusion—drawn, often irrationally, from the…
- experience—that we had upon acting on an…
- observation—often mistaking an illusion for the underlying…
- reality
…and how we can and often do go wrong at each step, and how little of the previous steps we can perceive at any given time.
What does this mean for managing/treating alcoholism or a tendency towards alchoholism?
It means interrupting those processes in a careful, surgically precise fashion, so that suddenly… The thing has no more power over us.
Whether you or a loved one struggle with a tendency to addiction (any addiction, actually, the advice goes the same), or are just curious about the wider factors at hand in the epidemiology of addiction, this book is for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s the difference between shyness and social anxiety?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
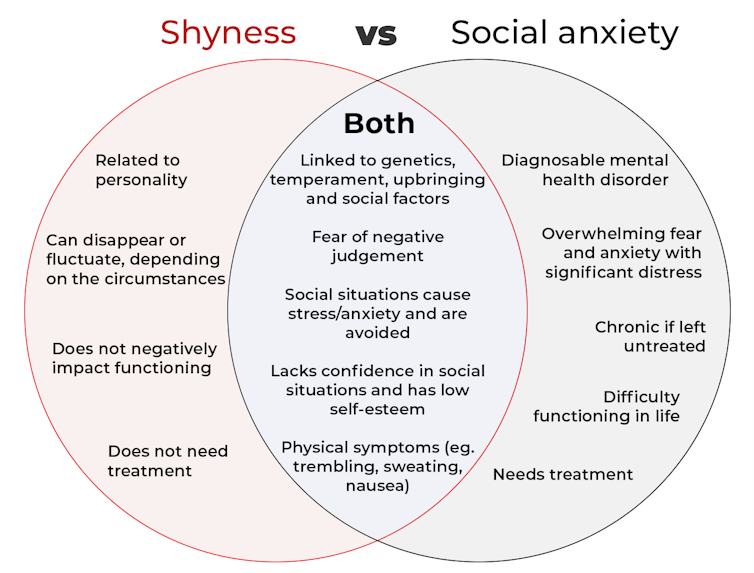
The terms “shyness” and “social anxiety” are often used interchangeably because they both involve feeling uncomfortable in social situations.
However, feeling shy, or having a shy personality, is not the same as experiencing social anxiety (short for “social anxiety disorder”).
Here are some of the similarities and differences, and what the distinction means.
pathdoc/Shutterstock How are they similar?
It can be normal to feel nervous or even stressed in new social situations or when interacting with new people. And everyone differs in how comfortable they feel when interacting with others.
For people who are shy or socially anxious, social situations can be very uncomfortable, stressful or even threatening. There can be a strong desire to avoid these situations.
People who are shy or socially anxious may respond with “flight” (by withdrawing from the situation or avoiding it entirely), “freeze” (by detaching themselves or feeling disconnected from their body), or “fawn” (by trying to appease or placate others).
A complex interaction of biological and environmental factors is also thought to influence the development of shyness and social anxiety.
For example, both shy children and adults with social anxiety have neural circuits that respond strongly to stressful social situations, such as being excluded or left out.
People who are shy or socially anxious commonly report physical symptoms of stress in certain situations, or even when anticipating them. These include sweating, blushing, trembling, an increased heart rate or hyperventilation.
How are they different?
Social anxiety is a diagnosable mental health condition and is an example of an anxiety disorder.
For people who struggle with social anxiety, social situations – including social interactions, being observed and performing in front of others – trigger intense fear or anxiety about being judged, criticised or rejected.
To be diagnosed with social anxiety disorder, social anxiety needs to be persistent (lasting more than six months) and have a significant negative impact on important areas of life such as work, school, relationships, and identity or sense of self.
Many adults with social anxiety report feeling shy, timid and lacking in confidence when they were a child. However, not all shy children go on to develop social anxiety. Also, feeling shy does not necessarily mean a person meets the criteria for social anxiety disorder.
People vary in how shy or outgoing they are, depending on where they are, who they are with and how comfortable they feel in the situation. This is particularly true for children, who sometimes appear reserved and shy with strangers and peers, and outgoing with known and trusted adults.
Individual differences in temperament, personality traits, early childhood experiences, family upbringing and environment, and parenting style, can also influence the extent to which people feel shy across social situations.
Not all shy children go on to develop social anxiety. 249 Anurak/Shutterstock However, people with social anxiety have overwhelming fears about embarrassing themselves or being negatively judged by others; they experience these fears consistently and across multiple social situations.
The intensity of this fear or anxiety often leads people to avoid situations. If avoiding a situation is not possible, they may engage in safety behaviours, such as looking at their phone, wearing sunglasses or rehearsing conversation topics.
The effect social anxiety can have on a person’s life can be far-reaching. It may include low self-esteem, breakdown of friendships or romantic relationships, difficulties pursuing and progressing in a career, and dropping out of study.
The impact this has on a person’s ability to lead a meaningful and fulfilling life, and the distress this causes, differentiates social anxiety from shyness.
Children can show similar signs or symptoms of social anxiety to adults. But they may also feel upset and teary, irritable, have temper tantrums, cling to their parents, or refuse to speak in certain situations.
If left untreated, social anxiety can set children and young people up for a future of missed opportunities, so early intervention is key. With professional and parental support, patience and guidance, children can be taught strategies to overcome social anxiety.
Why does the distinction matter?
Social anxiety disorder is a mental health condition that persists for people who do not receive adequate support or treatment.
Without treatment, it can lead to difficulties in education and at work, and in developing meaningful relationships.
Receiving a diagnosis of social anxiety disorder can be validating for some people as it recognises the level of distress and that its impact is more intense than shyness.
A diagnosis can also be an important first step in accessing appropriate, evidence-based treatment.
Different people have different support needs. However, clinical practice guidelines recommend cognitive-behavioural therapy (a kind of psychological therapy that teaches people practical coping skills). This is often used with exposure therapy (a kind of psychological therapy that helps people face their fears by breaking them down into a series of step-by-step activities). This combination is effective in-person, online and in brief treatments.
Treatment is available online as well as in-person. ImYanis/Shutterstock For more support or further reading
Online resources about social anxiety include:
- This Way Up’s online program for managing excessive shyness and fear of social situations
- Beyond Blue’s resources on social anxiety
- a guide to looking after yourself if you have social anxiety, from the Western Australian health department
- social anxiety online program for children and teens from the University of Queensland
- inroads, a self-guided online program for young adults who drink alcohol to manage their anxiety.
We thank the Black Dog Institute Lived Experience Advisory Network members for providing feedback and input for this article and our research.
Kayla Steele, Postdoctoral research fellow and clinical psychologist, UNSW Sydney and Jill Newby, Professor, NHMRC Emerging Leader & Clinical Psychologist, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: