The Simple Six – by Clinton Dobbins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We at 10almonds don’t believe in keeping things a mystery, so…
“The Simple Six” are:
- the squat
- the goblet squat
- the hinge
- the kettlebell swing
- the push
- the push-up
- the kettle-bell press
- the pull
- the chin-up
- the gait, and
- walking.
Ok, we’re being a little glib here because to be fair, those are chunked into six groups, but the point is: don’t let the title fool you into thinking the book could have been an article; there’s plenty of valuable content here.
That said, it is a short book (64 pages), but with an average of 10 pages per exercise type, it’s a lot more than for example we could ever put into our newsletter.
Bottom line: we know that 10almonds readers like simple, clear, evidence-based, to-the-point health information, and that’s what this book is, so we do recommend it.
Click here to check out The Simple Six, and streamline your workouts!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Spreading Mental Health Awareness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Request: more people need to be aware of suicidal tendencies and what they can do to ward them off
That’s certainly a very important topic! We’ll cover that properly in one of our Psychology Sunday editions. In the meantime, we’ll mention a previous special that we did, that was mostly about handling depression (in oneself or a loved one), and obviously there’s a degree of crossover:
The Mental Health First-Aid That You’ll Hopefully Never Need
Share This Post
-
Doctors From 15 Specialties Tell The Worst Common Mistakes People Make
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whatever your professional background, you probably know many things about it that are very obvious to you, but that most people don’t know. So it is for doctors too; here are the things that doctors from 15 specialties would never do, and thus advise people against doing:
Better safe than sorry
We’ll leap straight into it:
- General Surgery: avoid rushing into musculoskeletal or spinal surgery unless absolutely necessary; conservative treatments like physical therapy are often effective.
- Interventional Gastroenterology: avoid long-term, around-the-clock use of anti-inflammatory pain medications (e.g. Ibuprofen and friends) to prevent stomach ulcers.
- Podiatry: never place feet on the car dashboard due to the risk of severe injuries from airbag deployment.
- Rheumatology: avoid daily use of high heels to prevent joint and foot deformities, bunions, and pain.
- Otorhinolaryngology: never smoke, as it can lead to severe consequences like laryngectomy and other life-altering conditions.
- Pediatrics: avoid dangerous activities for children, such as swimming alone, eating choking hazards, biking or skiing without a helmet, or consuming raw meat/fish/dairy. Also, be cautious with firearms in homes.
- Orthopedic Surgery: avoid riding motorcycles and handling fireworks due to high risks of accidents.
- Emergency Medicine: never drink and drive or ride ATVs. Always use eye protection during activities like woodworking.
- Ophthalmology: always wear safety glasses during activities like grinding metal or woodworking. Sunglasses are essential to prevent UV damage even on cloudy days.
- Urology: avoid shaving pubic hair if diabetic or immunocompromised to prevent severe infections like Fournier’s gangrene.
- Gastroenterology: do not use gut health supplements as they lack proven efficacy and are often a waste of money*
- Plastic Surgery: avoid contour threads (barbed sutures for facial rejuvenation) and butt implants due to risks like infection, complications, and poor outcomes.
- Psychiatry: never take recreational drugs from unknown sources to avoid accidental overdoses, especially from substances laced with fentanyl. Carry Narcan for emergencies.
- Dermatology: use sunscreen daily to prevent skin cancer, aging, pigmentation issues, and texture problems caused by UV exposure.
- Cardiology: avoid the carnivore diet as it increases heart disease risks due to its negligible fiber content and high saturated fat intake.
*We had an article about this a while back; part of the problem is that taking probiotics without prebiotics can mean your new bacteria just die in about 20 minutes, which is their approximate lifespan in which to multiply or else die out. Similar problems arise if taking them with sugar that feeds their competitors instead. See: Stop Sabotaging Your Gut!
For more on each of these, in the words of the respective doctors, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
Why ’10almonds’? Newsletter Name Explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Each Thursday, we respond to subscriber questions and requests! If it’s something small, we’ll answer it directly; if it’s something bigger, we’ll do a main feature in a follow-up day instead!
So, no question/request to big or small; they’ll just get sorted accordingly
Remember, you can always hit reply to any of our emails, or use the handy feedback widget at the bottom. We always look forward to hearing from you!
Q: Why is your newsletter called 10almonds? Maybe I missed it in the intro email, but my curiosity wants to know the significance. Thanks!”
It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was online… So, calling ourselves 10almonds was a bit of a tongue-in-cheek reference to that story… but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Share This Post
Related Posts
-
Eating on the Wild Side: – by Jo Robinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is an investigative journalist, and it shows here, as she leaves no stone unturned in her quest for the truth in the face of many food myths.
She covers a lot of “popular wisdom” things that are varyingly true or false, or sometimes even both—in the case of food lore that’s a good rule of thumb, but has notable exceptions (e.g. “more colorful and/or darker-colored fruits/vegetables contain more nutrients”, which is a very good rule of thumb until one meets a cauliflower, for example).
She also covers food preparation myths, and how, to give one example, in spite of the popularity of “less cooked is better”, in some cases certain cooking methods will indeed destroy nutrients; in others, certain cooking methods will improve nutritional availability. Either by destroying an adjacent antinutrient (e.g. phytates), or by breaking something down into a more manageable form that our body can absorb. Knowing which is which, is important.
The book is organized by kinds of food, and does exclusively cover plants, but there’s more than enough material for any omnivore to enjoy.
The style is… Journalistic, it would be fair to say. Which is not surprising, given the author. But it means that it is written in a fairly narrative way, to draw the reader in and make it an enjoyable read while still being informative in all parts (there is no padding). In terms of science, the in-the-prose science is as minimal as possible to still convey what needs to be conveyed, while 25 pages of bibliography stack up at the end to show that indeed, this journalist cites sources.
Bottom line: this is a really enjoyable book, packed with a wealth of knowledge, and is perfect to uplift your cooking by knowing your ingredients a little more intimately!
Click here to check out Eating On The Wild Side, and, enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From banning junk food ads to a sugar tax: with diabetes on the rise, we can’t afford to ignore the evidence any longer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are renewed calls this week for the Australian government to implement a range of measures aimed at improving our diets. These include restrictions on junk food advertising, improvements to food labelling, and a levy on sugary drinks.
This time the recommendations come from a parliamentary inquiry into diabetes in Australia. Its final report, tabled in parliament on Wednesday, was prepared by a parliamentary committee comprising members from across the political spectrum.
The release of this report could be an indication that Australia is finally going to implement the evidence-based healthy eating policies public health experts have been recommending for years.
But we know Australian governments have historically been unwilling to introduce policies the powerful food industry opposes. The question is whether the current government will put the health of Australians above the profits of companies selling unhealthy food.
benjamas11/Shutterstock Diabetes in Australia
Diabetes is one of the fastest growing chronic health conditions in the nation, with more than 1.3 million people affected. Projections show the number of Australians diagnosed with the condition is set to rise rapidly in coming decades.
Type 2 diabetes accounts for the vast majority of cases of diabetes. It’s largely preventable, with obesity among the strongest risk factors.
This latest report makes it clear we need an urgent focus on obesity prevention to reduce the burden of diabetes. Type 2 diabetes and obesity cost the Australian economy billions of dollars each year and preventive solutions are highly cost-effective.
This means the money spent on preventing obesity and diabetes would save the government huge amounts in health care costs. Prevention is also essential to avoid our health systems being overwhelmed in the future.
What does the report recommend?
The report puts forward 23 recommendations for addressing diabetes and obesity. These include:
- restrictions on the marketing of unhealthy foods to children, including on TV and online
- improvements to food labelling that would make it easier for people to understand products’ added sugar content
- a levy on sugary drinks, where products with higher sugar content would be taxed at a higher rate (commonly called a sugar tax).
These key recommendations echo those prioritised in a range of reports on obesity prevention over the past decade. There’s compelling evidence they’re likely to work.
Restrictions on unhealthy food marketing
There was universal support from the committee for the government to consider regulating marketing of unhealthy food to children.
Public health groups have consistently called for comprehensive mandatory legislation to protect children from exposure to marketing of unhealthy foods and related brands.
An increasing number of countries, including Chile and the United Kingdom, have legislated unhealthy food marketing restrictions across a range of settings including on TV, online and in supermarkets. There’s evidence comprehensive policies like these are having positive results.
In Australia, the food industry has made voluntary commitments to reduce some unhealthy food ads directly targeting children. But these promises are widely viewed as ineffective.
The government is currently conducting a feasibility study on additional options to limit unhealthy food marketing to children.
But the effectiveness of any new policies will depend on how comprehensive they are. Food companies are likely to rapidly shift their marketing techniques to maximise their impact. If any new government restrictions do not include all marketing channels (such as TV, online and on packaging) and techniques (including both product and brand marketing), they’re likely to fail to adequately protect children.
Food labelling
Food regulatory authorities are currently considering a range of improvements to food labelling in Australia.
For example, food ministers in Australia and New Zealand are soon set to consider mandating the health star rating front-of-pack labelling scheme.
Public health groups have consistently recommended mandatory implementation of health star ratings as a priority for improving Australian diets. Such changes are likely to result in meaningful improvements to the healthiness of what we eat.
Regulators are also reviewing potential changes to how added sugar is labelled on product packages. The recommendation from the committee to include added sugar labelling on the front of product packaging is likely to support this ongoing work.
But changes to food labelling laws are notoriously slow in Australia. And food companies are known to oppose and delay any policy changes that might hurt their profits.
Health star ratings are not compulsory in Australia. BLACKDAY/Shutterstock A sugary drinks tax
Of the report’s 23 recommendations, the sugary drinks levy was the only one that wasn’t universally supported by the committee. The four Liberal and National party members of the committee opposed implementation of this policy.
As part of their rationale, the dissenting members cited submissions from food industry groups that argued against the measure. This follows a long history of the Liberal party siding with the sugary drinks industry to oppose a levy on their products.
The dissenting members didn’t acknowledge the strong evidence that a sugary drinks levy has worked as intended in a wide range of countries.
In the UK, for example, a levy on sugary drinks implemented in 2018 has successfully lowered the sugar content in UK soft drinks and reduced sugar consumption.
The dissenting committee members argued a sugary drinks levy would hurt families on lower incomes. But previous Australian modelling has shown the two most disadvantaged quintiles would reap the greatest health benefits from such a levy, and accrue the highest savings in health-care costs.
What happens now?
Improvements to population diets and prevention of obesity will require a comprehensive and coordinated package of policy reforms.
Globally, a range of countries facing rising epidemics of obesity and diabetes are starting to take such strong preventive action.
In Australia, after years of inaction, this week’s report is the latest sign that long-awaited policy change may be near.
But meaningful and effective policy change will require politicians to listen to the public health evidence rather than the protestations of food companies concerned about their bottom line.
Gary Sacks, Professor of Public Health Policy, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
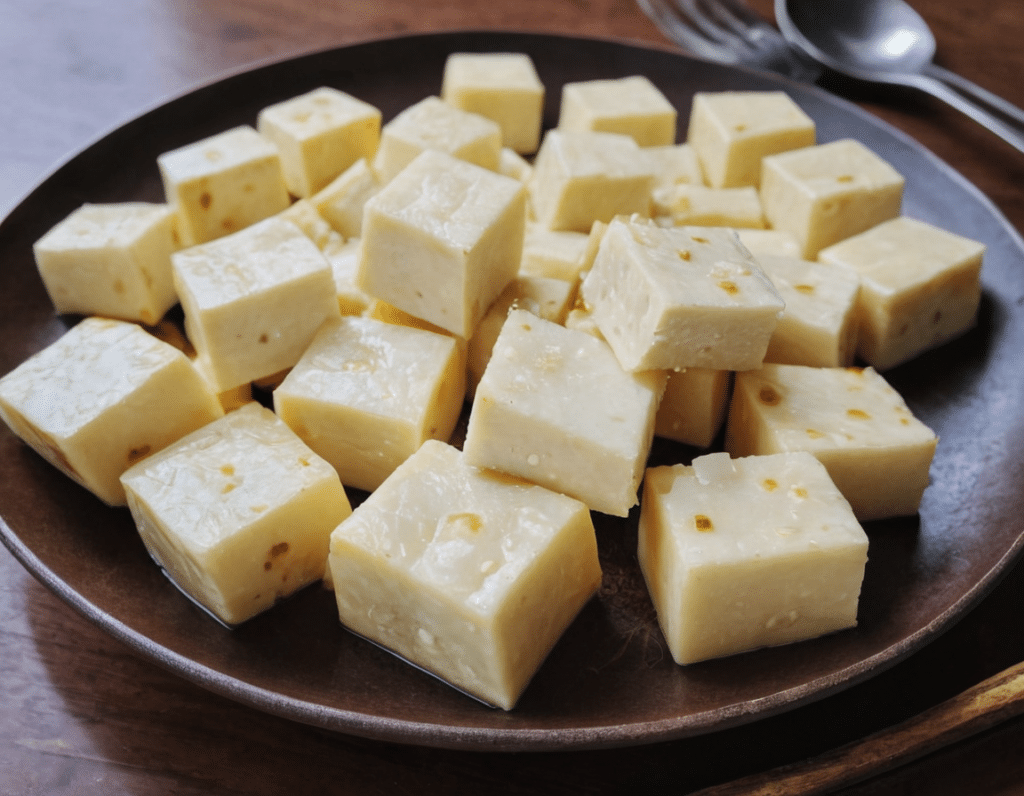
High-Protein Paneer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Paneer (a kind of Desi cheese used in many recipes from that region) is traditionally very high in fat, mostly saturated. Which is delicious, but not exactly the most healthy.
Today we’ll be making a plant-based paneer that does exactly the same jobs (has a similar texture and gentle flavor, takes on the flavors of dishes in the same way, etc) but with a fraction of the fat (of which only a trace amount is saturated, in this plant-based version), and even more protein. We’ll use this paneer in some recipes in the future, but it can be enjoyed by itself already, so let’s get going…
You will need
- ½ cup gram flour (unwhitened chickpea flour)
- Optional: 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Whisk the flour (and salt, if using) with 2 cups water in a big bowl, whisking until the texture is smooth.
2) Transfer to a large saucepan on a low-to-medium heat; you want it hot, but not quite a simmer. Keep whisking until the mixture becomes thick like polenta. This should take 10–15 minutes, so consider having someone else to take shifts if the idea of whisking continually for that long isn’t reasonable to you.
3) Transfer to a non-stick baking tin that will allow you to pour it about ½” deep. If the tin’s too large, you can always use a spatula to push it up against two or three sides, so that it’s the right depth
3) Refrigerate for at least 10 minutes, but longer is better if you have the time.
4) When ready to serve/use, cut it into ½” cubes. These can be served/used now, or kept for about a week in the fridge.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: