The Science-Backed Anti-Inflammatory Diet for Beginners – by Dr. Yasmine Elamir & Dr. William Grist
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have written about how to eat to beat inflammation, but what we didn’t do is include 75 recipes and a plan for building up one’s culinary repertoire around those core dishes!
That’s what this book does. It covers briefly the science of inflammation and anti-inflammatory diet, discusses experimental elimination diets (e.g. you eliminate likely culprits of triggering your inflammation, then reintroduce them one by one to see which it was), and ingredients likely to increase or decrease inflammation.
The 75 recipes are good, and/but a caveat is “yes, one of the recipes is ketchup and another is sour cream” so it’s not exactly 75 mains.
However! Where this book excels is in producing anti-inflammatory versions of commonly inflammatory dishes. That ketchup? Not sugary. The sour cream? Vegan. And so forth. We also see crispy roast potatoes, an array of desserts, and sections for popular holiday dishes too, so you will not need to be suddenly inflamed into the next dimension when it comes to festive eating.
The recipes are what the title claims them to be, “science-backed anti-inflammatory”, and that is clearly the main criterion for their inclusion. They are not by default vegan, vegetarian, dairy-free, nut-free, gluten-free, etc. For this reason, all recipes are marked with such tags as “V, VG, DF, GF, EF, NF” etc as applicable.
Bottom line: we’d consider this book more of a jumping-off point than a complete repertoire, but it’s a very good jumping-off point, and will definitely get you “up and running” (there’s a 21-day meal plan, for example).
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Habits of a Happy Brain – by Dr. Loretta Graziano Breuning
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are lots of books on “happy chemicals” and “how to retrain your brain”, so what makes this one different?
Firstly, it focuses on four “happy chemicals”, not just one:
- Serotonin
- Dopamine
- Oxytocin
- Endorphins
It also looks at the role of cortisol, and how it caps off each of those just a little bit, to keep us just a little malcontent.
Behavioral psychology tends to focus most on dopamine, while prescription pharmaceuticals for happiness (i.e., most antidepressants) tend to focus on serotonin. Here, Dr. Breuning helps us understand the complex interplay of all of the aforementioned chemicals.
She also clears up many misconceptions, since a lot of people misattribute the functions of each of these.
Common examples include “I’m doing this for the serotonin!” when the activity is dopaminergic not serotoninergic, or considering dopamine “the love molecule” when oxytocin, or even something else like phenylethylamine would be more appropriate.
The above may seem like academic quibbles and not something of practical use, but if we want to biohack our brains, we need to do better than the equivalent of a chef who doesn’t know the difference between salt and sugar.
Where things are of less practical use, she tends to skip over or at least streamline them. For example, she doesn’t really discuss the role of post-dopamine prolactin in men—but the discussion of post-happiness cortisol covers the same ground anyway, for practical purposes.
Dr. Breuning also looks at where our evolved neurochemical responses go wrong, and lays out guidelines for such challenges as overcoming addiction, or embracing delayed gratification.
Bottom line: this book is a great user-manual for the brain. If you’d like to be happier and more effective with fewer bad habits, this is the book for you.
Click here to check out Habits of a Happy Brain, and get biohacking yours!
Share This Post
-
How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
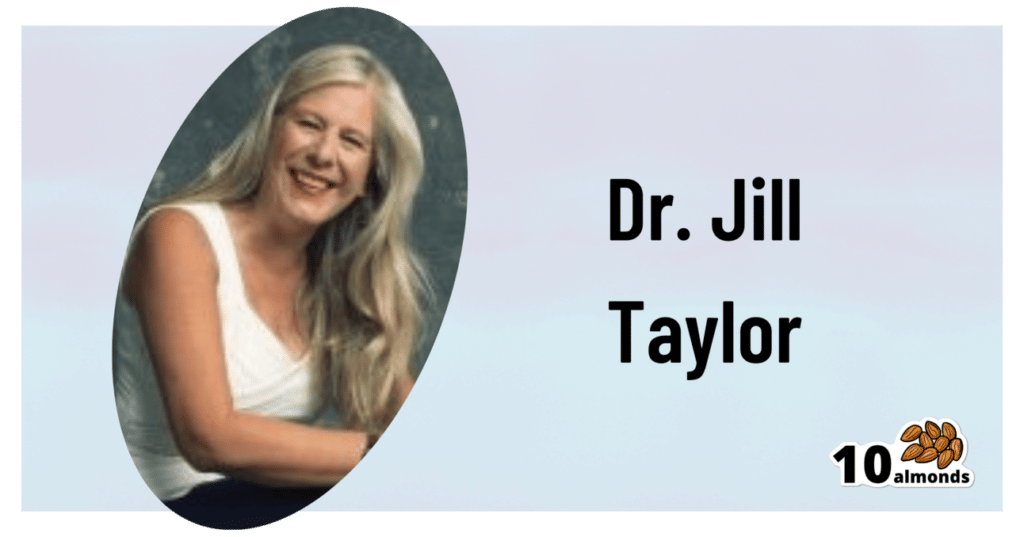
The Stroke Of Insight That Nobody Wants
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Share This Post
-
Pistachios vs Pine Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to pine nuts, we picked the pistachios.
Why?
First looking at the macros, pistachios have nearly 2x the protein while pine nuts have nearly 2x the fat. The fats are healthy in moderation (mostly polyunsaturated, a fair portion of monounsaturated, and a little saturated), but we’re going to value the protein content higher. Also, pistachios have approximately 2x the carbs, and/but nearly 3x the fiber. All in all, we’ll call this section a moderate win for pistachios.
When it comes to vitamins, pistachios have more of vitamins A, B1, B5, B6, B9, and C, while pine nuts have more of vitamins B2, B3, E, K, and choline. All in all, pistachios are scraping a 6:5 win here, or we could call it a tie if we want to value pine nuts’ vitamins more (due to the difference in how many foods each vitamin is found in, and thus the likelihood of having a deficiency or not).
In the category of minerals, pistachios have more calcium, copper, potassium, and selenium, while pine nuts have more iron, magnesium, manganese, and zinc. This would be a tie if we just call it 4:4, but what’s worth noting is that while both of these nuts are a good source of most of the minerals mentioned, pine nuts aren’t a very good source of calcium or selenium, so we’re going to declare this section a very marginal win for pistachios.
Adding up the moderate win, the scraped win, and the barely scraped win, all adds up to a win for pistachios. However, as you might have noticed, both are great so do enjoy both if you can!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
Related Posts
-
Pain Doesn’t Belong on a Scale of Zero to 10
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Over the past two years, a simple but baffling request has preceded most of my encounters with medical professionals: “Rate your pain on a scale of zero to 10.”
I trained as a physician and have asked patients the very same question thousands of times, so I think hard about how to quantify the sum of the sore hips, the prickly thighs, and the numbing, itchy pain near my left shoulder blade. I pause and then, mostly arbitrarily, choose a number. “Three or four?” I venture, knowing the real answer is long, complicated, and not measurable in this one-dimensional way.
Pain is a squirrely thing. It’s sometimes burning, sometimes drilling, sometimes a deep-in-the-muscles clenching ache. Mine can depend on my mood or how much attention I afford it and can recede nearly entirely if I’m engrossed in a film or a task. Pain can also be disabling enough to cancel vacations, or so overwhelming that it leads people to opioid addiction. Even 10+ pain can be bearable when it’s endured for good reason, like giving birth to a child. But what’s the purpose of the pains I have now, the lingering effects of a head injury?
The concept of reducing these shades of pain to a single number dates to the 1970s. But the zero-to-10 scale is ubiquitous today because of what was called a “pain revolution” in the ’90s, when intense new attention to addressing pain — primarily with opioids — was framed as progress. Doctors today have a fuller understanding of treating pain, as well as the terrible consequences of prescribing opioids so readily. What they are learning only now is how to better measure pain and treat its many forms.
About 30 years ago, physicians who championed the use of opioids gave robust new life to what had been a niche specialty: pain management. They started pushing the idea that pain should be measured at every appointment as a “fifth vital sign.” The American Pain Society went as far as copyrighting the phrase. But unlike the other vital signs — blood pressure, temperature, heart rate, and breathing rate — pain had no objective scale. How to measure the unmeasurable? The society encouraged doctors and nurses to use the zero-to-10 rating system. Around that time, the FDA approved OxyContin, a slow-release opioid painkiller made by Purdue Pharma. The drugmaker itself encouraged doctors to routinely record and treat pain, and aggressively marketed opioids as an obvious solution.
To be fair, in an era when pain was too often ignored or undertreated, the zero-to-10 rating system could be regarded as an advance. Morphine pumps were not available for those cancer patients I saw in the ’80s, even those in agonizing pain from cancer in their bones; doctors regarded pain as an inevitable part of disease. In the emergency room where I practiced in the early ’90s, prescribing even a few opioid pills was a hassle: It required asking the head nurse to unlock a special prescription pad and making a copy for the state agency that tracked prescribing patterns. Regulators (rightly) worried that handing out narcotics would lead to addiction. As a result, some patients in need of relief likely went without.
After pain doctors and opioid manufacturers campaigned for broader use of opioids — claiming that newer forms were not addictive, or much less so than previous incarnations — prescribing the drugs became far easier and were promoted for all kinds of pain, whether from knee arthritis or back problems. As a young doctor joining the “pain revolution,” I probably asked patients thousands of times to rate their pain on a scale of zero to 10 and wrote many scripts each week for pain medication, as monitoring “the fifth vital sign” quickly became routine in the medical system. In time, a zero-to-10 pain measurement became a necessary box to fill in electronic medical records. The Joint Commission on the Accreditation of Healthcare Organizations made regularly assessing pain a prerequisite for medical centers receiving federal health care dollars. Medical groups added treatment of pain to their list of patient rights, and satisfaction with pain treatment became a component of post-visit patient surveys. (A poor showing could mean lower reimbursement from some insurers.)
But this approach to pain management had clear drawbacks. Studies accumulated showing that measuring patients’ pain didn’t result in better pain control. Doctors showed little interest in or didn’t know how to respond to the recorded answer. And patients’ satisfaction with their doctors’ discussion of pain didn’t necessarily mean they got adequate treatment. At the same time, the drugs were fueling the growing opioid epidemic. Research showed that an estimated 3% to 19% of people who received a prescription for pain medication from a doctor developed an addiction.
Doctors who wanted to treat pain had few other options, though. “We had a good sense that these drugs weren’t the only way to manage pain,” Linda Porter, director of the National Institutes of Health’s Office of Pain Policy and Planning, told me. “But we didn’t have a good understanding of the complexity or alternatives.” The enthusiasm for narcotics left many varietals of pain underexplored and undertreated for years. Only in 2018, a year when nearly 50,000 Americans died of an overdose, did Congress start funding a program — the Early Phase Pain Investigation Clinical Network, or EPPIC-Net — designed to explore types of pain and find better solutions. The network connects specialists at 12 academic specialized clinical centers and is meant to jump-start new research in the field and find bespoke solutions for different kinds of pain.
A zero-to-10 scale may make sense in certain situations, such as when a nurse uses it to adjust a medication dose for a patient hospitalized after surgery or an accident. And researchers and pain specialists have tried to create better rating tools — dozens, in fact, none of which was adequate to capture pain’s complexity, a European panel of experts concluded. The Veterans Health Administration, for instance, created one that had supplemental questions and visual prompts: A rating of 5 correlated with a frown and a pain level that “interrupts some activities.” The survey took much longer to administer and produced results that were no better than the zero-to-10 system. By the 2010s, many medical organizations, including the American Medical Association and the American Academy of Family Physicians, were rejecting not just the zero-to-10 scale but the entire notion that pain could be meaningfully self-reported numerically by a patient.
In the years that opioids had dominated pain remedies, a few drugs — such as gabapentin and pregabalin for neuropathy, and lidocaine patches and creams for musculoskeletal aches — had become available. “There was a growing awareness of the incredible complexity of pain — that you would have to find the right drugs for the right patients,” Rebecca Hommer, EPPIC-Net’s interim director, told me. Researchers are now looking for biomarkers associated with different kinds of pain so that drug studies can use more objective measures to assess the medications’ effect. A better understanding of the neural pathways and neurotransmitters that create different types of pain could also help researchers design drugs to interrupt and tame them.
Any treatments that come out of this research are unlikely to be blockbusters like opioids; by design, they will be useful to fewer people. That also makes them less appealing prospects to drug companies. So EPPIC-Net is helping small drug companies, academics, and even individual doctors design and conduct early-stage trials to test the safety and efficacy of promising pain-taming molecules. That information will be handed over to drug manufacturers for late-stage trials, all with the aim of getting new drugs approved by the FDA more quickly.
The first EPPIC-Net trials are just getting underway. Finding better treatments will be no easy task, because the nervous system is a largely unexplored universe of molecules, cells, and electronic connections that interact in countless ways. The 2021 Nobel Prize in Physiology or Medicine went to scientists who discovered the mechanisms that allow us to feel the most basic sensations: cold and hot. In comparison, pain is a hydra. A simple number might feel definitive. But it’s not helping anyone make the pain go away.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
AC: The Power of Appetite Correction – by Dr. Bert Herring
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Appetite Correction” is an intriguing concept, and so it intrigued us sufficiently to read this book. So what’s it about?
It’s about modifying our response to hunger, and treating it as a messenger to whom we may say “thank you for your opinion” and then do as we already planned to do. And what is that?
Simply, this book is about intermittent fasting, specifically, 19:5 fasting, i.e., fast for 19 hours and eat during a 5hr window each day (the author proposes 5pm–10pm, but honestly, go with what works for you).
During the fasting period, drinking water, or consuming other non insulin-signalling things (e.g. black coffee, black tea, herbal tea, etc) is fine, but not so much as a bite of anything else (nor calorific drinks, e.g. with milk/cream or sugar in, and certainly not sodas, juices, etc).
During the eating period, the idea is to eat at will without restriction (even unhealthy things, if such is your desire) during those 5 hours, with the exception that one should start with something healthy. In other words, you can line up that take-out if you want, but eat a carrot first to break the fast. Or some nuts. Or whatever, but healthy.
The “appetite correction” part of it comes in with how, after a short adjustment period, you will get used to not suffering from hunger during the fasting period, and during the eating period, you will—paradoxically—be more able to practise moderation in your portions.
Most of the book is given over the dealing with psychological difficulties/objections, as well as some social objections, but he does also explain some of the science at hand too (i.e. how intermittent fasting works, on a physiological level). On which note…
The style is on the very light end of pop-science, and unusually, he doesn’t cite any sources for his claims at all. Now, no science that he claimed struck this reviewer as out of the ordinary, but it would have been nice to see a good few pages of bibliography at the back.
Bottom line: this is a super quick-and-easy read that makes a strong (albeit unsourced) case for intermittent fasting. It’s probably best for someone who would like the benefits and needs some persuading, but who is not very interested in delving into the science beyond being content to understand what is explained and put it into practice.
Click here to check out AC: The Power of Appetite Correction, and get yours where you want it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
You Are the One You’ve Been Waiting For – by Dr. Richard Schwartz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As self-therapy approaches go, the title here could be read two ways: as pop-psychology fluff, or a suggestion of something deeper. And, while written in a way to make it accessible to all, we’re happy to report the content consists of serious therapeutic ideas, presented clearly.
Internal Family Systems (IFS) is a large, internationally recognized, and popular therapeutic approach. It’s also an approach that lends itself quite well to self-therapy, as this book illustrates.
Dr. Schwartz kicks off by explaining not IFS, but the problem that it solves… We (most of us, anyway) have over the course of our lives tried to plug the gaps in our own unmet psychological needs. And, that can cause resentment, strain, and can even be taken out on others if we’re not careful.
The real meat of the book, however, is in its illustrative explanations of how IFS works, and can be applied by an individual. The goal is to recognize all the parts that make us who we are, understand what they need in order to be at peace, and give them that. Spoiler: most what they will need is just being adequately heard, rather than locked in a box untended.
One of the benefits of using this book for self-therapy, of course, is that it requires a lot less vulnerability with a third party.
But, speaking of which, what of these intimate relationships the subtitle of the book referenced? Mostly the benefits to such come from a “put your own oxygen mask on first” angle… but the book does also cover discussions between intimate partners, and approaches to love, including what the author calls “courageous love”.
Bottom line: this is a great book if you want to do some “spring-cleaning of the soul” and live a little more lightly as a result.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: