The End Of Diabetes – by Dr. Joel Fuhrman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed another of Dr. Fuhrman’s books, “Eat To Live”, and this time, he’s focusing specifically on preventing/reversing type 2 diabetes.
And yes, this is really only about type 2 diabetes. Type 1 diabetics can still benefit from this dietary approach (it won’t cure T1D but it will help manage it), as indeed can people with one of the rarer forms of diabetes or for that matter people with no diabetes at all (it’s great for all of us to avoid blood sugar spikes and improve insulin sensitivity)… But this book is written with the type diabetic firmly in mind.
The title “The End Of…” is fair, by the way—on an individual level, at the very least. While most doctors treat type 2 diabetes as a lifelong condition to be managed, the simple (well-evidenced and honestly uncontroversial at this point) truth is that it can be reversed. So, why not do that?
The dietary approach here is sensible: eat many plants, aim for high protein, high fiber, low carb, and limit animal products to just small portions of those that don’t spike insulin levels.
It’s worth noting that Dr. Fuhrman’s “Nutritarian Diet” (which works by assigning all foods a single numerical aggregate nutritional value) has been criticised as being pseudoscientific, and technically it is (there is no evidence-base that optimizing nutrients in this fashion is best; indeed, it could result in missing out on some nutrients that are critical but occur only in otherwise lower-scoring foods—see for example if someone notes how highly Brussels sprouts score and decides to eat only Brussels sprouts, thus missing out on nutrients that aren’t in this otherwise top-tier food), but in practical application, it clearly works well and helps people to eat more nutritionally-dense foods, on balance, which can only be a good thing.
The style of the book is information-dense pop-science (with more than 20 pages of bibliography to back it up), with also a recipe section (60 pages of that). The recipes are a touch on the basic side for this reviewer’s tastes, but perhaps that’s no bad thing—it provides a good “base” from which we can all personalize our recipes according to our preferences and local availability of ingredients.
Bottom line: whether or not you (and/or a loved one) are diabetic, this is a great book for understanding glycemic control and insulin sensitivity, and a great resource for improving those in one’s own life and one’s own body.
Click here to check out The End Of Diabetes, and put an end to diabetes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Gut Feelings – by Dr Will Cole
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More and more, science is uncovering links between our gut health and the rest of our health—including our mental health! We all know “get some fiber and consider probiotics”, but what else is there that we can do?
Quite a lot, actually. And part of it, which Dr. Cole also explores, is the fact that the gut-brain highway is a two-way street!
The book looks a lot especially at the particular relationship between shame and eating. The shame need not initially be about eating, though it can certainly end up that way too. But any kind of shame—be it relating to one’s body, work, relationship, or anything else, can not only have a direct effect on the gut, but indirect too:
Once our “eating our feelings” instinct kicks in, things can spiral from there, after all.
So, Dr. Cole walks us through tackling this from both sides—nutrition and psychology. With chapters full of tips and tricks, plus a 21-day plan (not a diet plan, a habit integration plan), this book hits shame (and inflammation, incidentally) hard and leads us into much healthier habits and cycles.
In short: if you’d like to have a better relationship with your food, improve your gut health, and/or reduce inflammation, this is definitely a book for you!
Share This Post
-
The Checklist Manifesto – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Gawande, himself a general surgeon, uses checklists a lot. He is, unequivocally, an expert in his field. He “shouldn’t” need a checklist to tell him to do such things as “Check you have the correct patient”. But checklists are there as a safety net. And, famously, “safety regulations are written in blood”, after all.
And, who amongst us has never made such a “silly” error? From forgetting to turn the oven on, to forgetting to take the handbrake off, it takes only a momentary distraction to think we’ve done something we haven’t.
You may be wondering: why a whole book on this? Is it just many examples of the usefulness of checklists? Because I’m already sold on that, so, what else am I going to get out of it?
Dr. Gawande also explains in clear terms:
- How to optimize “all necessary steps” with “as few steps as possible”
- The important difference between read-do checklists and do-confirm checklists
- To what extent we should try to account for the unexpected
- How to improve compliance (i.e., making sure you actually use it, no matter how tempting it will be to go “yeah this is automatic for me now” and gloss over it)
- The role of checklists in teams, and in passing on knowledge
…and more.
Bottom line: if you’ve ever tried to make tea without putting the tea-leaves in the pot, this is the book that will help you avoid making more costly mistakes—whatever your area of activity or interest.
Click here to check out the Checklist Manifesto, and make fewer mistakes!
Share This Post
-
A short history of sunscreen, from basting like a chook to preventing skin cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australians have used commercial creams, lotions or gels to manage our skin’s sun exposure for nearly a century.
But why we do it, the preparations themselves, and whether they work, has changed over time.
In this short history of sunscreen in Australia, we look at how we’ve slathered, slopped and spritzed our skin for sometimes surprising reasons.
At first, suncreams helped you ‘tan with ease’
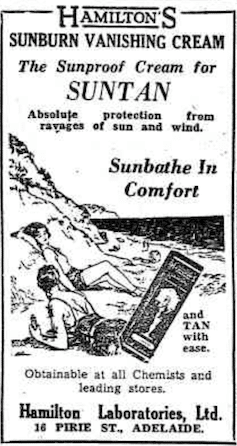
This early sunscreen claimed you could ‘tan with ease’.
Trove/NLASunscreens have been available in Australia since the 30s. Chemist Milton Blake made one of the first.
He used a kerosene heater to cook batches of “sunburn vanishing cream”, scented with French perfume.
His backyard business became H.A. Milton (Hamilton) Laboratories, which still makes sunscreens today.
Hamilton’s first cream claimed you could “
Sunbathe in Comfort and TAN with ease”. According to modern standards, it would have had an SPF (or sun protection factor) of 2.The mirage of ‘safe tanning’
A tan was considered a “modern complexion” and for most of the 20th century, you might put something on your skin to help gain one. That’s when “safe tanning” (without burning) was thought possible.
This 1967 Coppertone advertisement urged you to ‘tan, not burn’.
SenseiAlan/Flickr, CC BY-SASunburn was known to be caused by the UVB component of ultraviolet (UV) light. UVA, however, was thought not to be involved in burning; it was just thought to darken the skin pigment melanin. So, medical authorities advised that by using a sunscreen that filtered out UVB, you could “safely tan” without burning.
But that was wrong.
From the 70s, medical research suggested UVA penetrated damagingly deep into the skin, causing ageing effects such as sunspots and wrinkles. And both UVA and UVB could cause skin cancer.
Sunscreens from the 80s sought to be “broad spectrum” – they filtered both UVB and UVA.
Researchers consequently recommended sunscreens for all skin tones, including for preventing sun damage in people with dark skin.
Delaying burning … or encouraging it?
Up to the 80s, sun preparations ranged from something that claimed to delay burning, to preparations that actively encouraged it to get that desirable tan – think, baby oil or coconut oil. Sun-worshippers even raided the kitchen cabinet, slicking olive oil on their skin.
One manufacturer’s “sun lotion” might effectively filter UVB; another’s merely basted you like a roast chicken.
Since labelling laws before the 80s didn’t require manufacturers to list the ingredients, it was often hard for consumers to tell which was which.
At last, SPF arrives to guide consumers
In the 70s, two Queensland researchers, Gordon Groves and Don Robertson, developed tests for sunscreens – sometimes experimenting on students or colleagues. They printed their ranking in the newspaper, which the public could use to choose a product.
An Australian sunscreen manufacturer then asked the federal health department to regulate the industry. The company wanted standard definitions to market their products, backed up by consistent lab testing methods.
In 1986, after years of consultation with manufacturers, researchers and consumers, Australian Standard AS2604 gave a specified a testing method, based on the Queensland researchers’ work. We also had a way of expressing how well sunscreens worked – the sun protection factor or SPF.
This is the ratio of how long it takes a fair-skinned person to burn using the product compared with how long it takes to burn without it. So a cream that protects the skin sufficiently so it takes 40 minutes to burn instead of 20 minutes has an SPF of 2.
Manufacturers liked SPF because businesses that invested in clever chemistry could distinguish themselves in marketing. Consumers liked SPF because it was easy to understand – the higher the number, the better the protection.
Australians, encouraged from 1981 by the Slip! Slop! Slap! nationwide skin cancer campaign, could now “slop” on a sunscreen knowing the degree of protection it offered.
How about skin cancer?
It wasn’t until 1999 that research proved that using sunscreen prevents skin cancer. Again, we have Queensland to thank, specifically the residents of Nambour. They took part in a trial for nearly five years, carried out by a research team led by Adele Green of the Queensland Institute of Medical Research. Using sunscreen daily over that time reduced rates of squamous cell carcinoma (a common form of skin cancer) by about 60%.
Follow-up studies in 2011 and 2013 showed regular sunscreen use almost halved the rate of melanoma and slowed skin ageing. But there was no impact on rates of basal cell carcinoma, another common skin cancer.
By then, researchers had shown sunscreen stopped sunburn, and stopping sunburn would prevent at least some types of skin cancer.
What’s in sunscreen today?
An effective sunscreen uses one or more active ingredients in a cream, lotion or gel. The active ingredient either works:
-
“chemically” by absorbing UV and converting it to heat. Examples include PABA (para-aminobenzoic acid) and benzyl salicylate, or
-
“physically” by blocking the UV, such as zinc oxide or titanium dioxide.
Physical blockers at first had limited cosmetic appeal because they were opaque pastes. (Think cricketers with zinc smeared on their noses.)
With microfine particle technology from the 90s, sunscreen manufacturers could then use a combination of chemical absorbers and physical blockers to achieve high degrees of sun protection in a cosmetically acceptable formulation.
Where now?
Australians have embraced sunscreen, but they still don’t apply enough or reapply often enough.
Although some people are concerned sunscreen will block the skin’s ability to make vitamin D this is unlikely. That’s because even SPF50 sunscreen doesn’t filter out all UVB.
There’s also concern about the active ingredients in sunscreen getting into the environment and whether their absorption by our bodies is a problem.
Sunscreens have evolved from something that at best offered mild protection to effective, easy-to-use products that stave off the harmful effects of UV. They’ve evolved from something only people with fair skin used to a product for anyone.
Remember, slopping on sunscreen is just one part of sun protection. Don’t forget to also slip (protective clothing), slap (hat), seek (shade) and slide (sunglasses).
Laura Dawes, Research Fellow in Medico-Legal History, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Related Posts
-
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight
Debra Prichard was a retired factory worker who was careful with her money, including what she spent on medical care, said her daughter, Alicia Wieberg. “She was the kind of person who didn’t go to the doctor for anything.”
That ended last year, when the rural Tennessee resident suffered a devastating stroke and several aneurysms. She twice was rushed from her local hospital to Vanderbilt University Medical Center in Nashville, 79 miles away, where she was treated by brain specialists. She died Oct. 31 at age 70.
One of Prichard’s trips to the Nashville hospital was via helicopter ambulance. Wieberg said she had heard such flights could be pricey, but she didn’t realize how extraordinary the charge would be — or how her mother’s skimping on Medicare coverage could leave the family on the hook.
Then the bill came.
The Patient: Debra Prichard, who had Medicare Part A insurance before she died.
Medical Service: An air-ambulance flight to Vanderbilt University Medical Center.
Service Provider: Med-Trans Corp., a medical transportation service that is part of Global Medical Response, an industry giant backed by private equity investors. The larger company operates in all 50 states and says it has a total of 498 helicopters and airplanes.
Total Bill: $81,739.40, none of which was covered by insurance.
What Gives: Sky-high bills from air-ambulance providers have sparked complaints and federal action in recent years.
For patients with private insurance coverage, the No Surprises Act, which went into effect in 2022, bars air-ambulance companies from billing people more than they would pay if the service were considered “in-network” with their health insurers. For patients with public coverage, such as Medicare or Medicaid, the government sets payment rates at much lower levels than the companies charge.
But Prichard had opted out of the portion of Medicare that covers ambulance services.
That meant when the bill arrived less than two weeks after her death, her estate was expected to pay the full air-ambulance fee of nearly $82,000. The main assets are 12 acres of land and her home in Decherd, Tennessee, where she lived for 48 years and raised two children. The bill for a single helicopter ride could eat up roughly a third of the estate’s value, said Wieberg, who is executor.
The family’s predicament stems from the complicated nature of Medicare coverage.
Prichard was enrolled only in Medicare Part A, which is free to most Americans 65 or older. That section of the federal insurance program covers inpatient care, and it paid most of her hospital bills, her daughter said.
But Prichard declined other Medicare coverage, including Part B, which handles such things as doctor visits, outpatient treatment, and ambulance rides. Her daughter suspects she skipped that coverage to avoid the premiums most recipients pay, which currently are about $175 a month.
Loren Adler, a health economist for the Brookings Institution who studies ambulance bills, estimated the maximum charge that Medicare would have allowed for Prichard’s flight would have been less than $10,000 if she’d signed up for Part B. The patient’s share of that would have been less than $2,000. Her estate might have owed nothing if she’d also purchased supplemental “Medigap” coverage, as many Medicare members do to cover things like coinsurance, he said.
Nicole Michel, a spokesperson for Global Medical Response, the ambulance provider, agreed with Adler’s estimate that Medicare would have limited the charge for the flight to less than $10,000. But she said the federal program’s payment rates don’t cover the cost of providing air-ambulance services.
“Our patient advocacy team is actively engaged with Ms. Wieberg’s attorney to determine if there was any other applicable medical coverage on the date of service that we could bill to,” Michel wrote in an email to KFF Health News. “If not, we are fully committed to working with Ms. Wieberg, as we do with all our patients, to find an equitable solution.”
The Resolution: In mid-February, Wieberg said the company had not offered to reduce the bill.
Wieberg said she and the attorney handling her mother’s estate both contacted the company, seeking a reduction in the bill. She said she also contacted Medicare officials, filled out a form on the No Surprises Act website, and filed a complaint with Tennessee regulators who oversee ambulance services. She said she was notified Feb. 12 that the company filed a legal claim against the estate for the entire amount.
Wieberg said other health care providers, including ground ambulance services and the Vanderbilt hospital, wound up waiving several thousand dollars in unpaid fees for services they provided to Prichard that are normally covered by Medicare Part B.
But as it stands, Prichard’s estate owes about $81,740 to the air-ambulance company.
More from Bill of the Month
- The Colonoscopies Were Free. But the ‘Surgical Trays’ Came With $600 Price Tags. Jan 25, 2024
- When a Quick Telehealth Visit Yields Multiple Surprises Beyond a Big Bill Dec 19, 2023
- Out for Blood? For Routine Lab Work, the Hospital Billed Her $2,400 Nov 21, 2023
The Takeaway: People who are eligible for Medicare are encouraged to sign up for Part B, unless they have private health insurance through an employer or spouse.
“If someone with Medicare finds that they are having difficulty paying the Medicare Part B premiums, there are resources available to help compare Medicare coverage choices and learn about options to help pay for Medicare costs,” Meena Seshamani, director of the federal Center for Medicare, said in an email to KFF Health News.
She noted that every state offers free counseling to help people navigate Medicare.
In Tennessee, that counseling is offered by the State Health Insurance Assistance Program. Its director, Lori Galbreath, told KFF Health News she wishes more seniors would discuss their health coverage options with trained counselors like hers.
“Every Medicare recipient’s experience is different,” she said. “We can look at their different situations and give them an unbiased view of what their next best steps could be.”
Counselors advise that many people with modest incomes enroll in a Medicare Savings Program, which can cover their Part B premiums. In 2023, Tennessee residents could qualify for such assistance if they made less than $1,660 monthly as a single person or $2,239 as a married couple. Many people also could obtain help with other out-of-pocket expenses, such as copays for medical services.
Wieberg, who lives in Missouri, has been preparing the family home for sale.
She said the struggle over her mother’s air-ambulance bill makes her wonder why Medicare is split into pieces, with free coverage for inpatient care under Part A, but premiums for coverage of other crucial services under Part B.
“Anybody past the age of 70 is likely going to need both,” she said. “And so why make it a decision of what you can afford or not afford, or what you think you’re going to use or not use?”
Bill of the Month is a crowdsourced investigation by KFF Health News and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
ADHD medication – can you take it long term? What are the risks and do benefits continue?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Attention deficit hyperactivity disorder (ADHD) is a condition that can affect all stages of life. Medication is not the only treatment, but it is often the treatment that can make the most obvious difference to a person who has difficulties focusing attention, sitting still or not acting on impulse.
But what happens once you’ve found the medication that works for you or your child? Do you just keep taking it forever? Here’s what to consider.
What are ADHD medications?
The mainstay of medication for ADHD is stimulants. These include methylphenidate (with brand names Ritalin, Concerta) and dexamfetamine. There is also lisdexamfetamine (branded Vyvanse), a “prodrug” of dexamfetamine (it has a protein molecule attached, which is removed in the body to release dexamfetamine).
There are also non-stimulants, in particular atomoxetine and guanfacine, which are used less often but can also be highly effective. Non-stimulants can be prescribed by GPs but this may not always be covered by the Pharmaceutical Benefits Scheme and could cost more.
How stimulants work
Some stimulants prescribed for ADHD are “short acting”. This means the effect comes on after around 20 minutes and lasts around four hours.
Longer-acting stimulants give a longer-lasting effect, usually by releasing medication more slowly. The choice between the two will be guided by whether the person wants to take medication once a day or prefers to target the medication effect to specific times or tasks.
For the stimulants (with the possible exception of lisdexamfetamine) there is very little carry-over effect to the next day. This means the symptoms of ADHD may be very obvious until the first dose of the morning takes effect.
One of the main aims of treatment is the person with ADHD should live their best life and achieve their goals. In young children it is the parents who have to consider the risks and benefits on behalf of the child. As children mature, their role in decision making increases.
What about side effects?
The most consistent side effects of the stimulants are they suppress appetite, resulting in weight loss. In children this is associated with temporary slowing of the growth rate and perhaps a slight delay in pubertal development. They can also increase the heart rate and may cause a rise in blood pressure. Stimulants often cause insomnia.
These changes are largely reversible on stopping medication. However, there is concern the small rises in blood pressure could accelerate the rate of heart disease, so people who take medication over a number of years might have heart attacks or strokes slightly sooner than would have happened otherwise.
This does not mean older adults should not have their ADHD treated. Rather, they should be aware of the potential risks so they can make an informed decision. They should also make sure high blood pressure and attacks of chest pain are taken seriously.
Stimulants can be associated with stomach ache or headache. These effects may lessen over time or with a reduction in dose. While there have been reports about stimulants being misused by students, research on the risks of long-term prescription stimulant dependence is lacking.
Will medication be needed long term?
Although ADHD can affect a person’s functioning at all stages of their life, most people stop medication within the first two years.
People may stop taking it because they don’t like the way it makes them feel, or don’t like taking medication at all. Their short period on medication may have helped them develop a better understanding of themselves and how best to manage their ADHD.
In teenagers the medication may lose its effectiveness as they outgrow their dose and so they stop taking it. But this should be differentiated from tolerance, when the dose becomes less effective and there are only temporary improvements with dose increases.
Tolerance may be managed by taking short breaks from medication, switching from one stimulant to another or using a non-stimulant.
Medication is usually prescribed by a specialist but rules differ around Australia.
Ground Picture/ShutterstockToo many prescriptions?
ADHD is becoming increasingly recognised, with more people – 2–5% of adults and 5–10% of children – being diagnosed. In Australia stimulants are highly regulated and mainly prescribed by specialists (paediatricians or psychiatrists), though this differs from state to state. As case loads grow for this lifelong diagnosis, there just aren’t enough specialists to fit everyone in.
In November, a Senate inquiry report into ADHD assessment and support services highlighted the desperation experienced by people seeking treatment.
There have already been changes to the legislation in New South Wales that may lead to more GPs being able to treat ADHD. Further training could help GPs feel more confident to manage ADHD. This could be in a shared-care arrangement or independent management of ADHD by GPs like a model being piloted at Nepean Blue Mountains Local Health District, with GPs training within an ADHD clinic (where I am a specialist clinician).
Not every person with ADHD will need or want to take medication. However, it should be more easily available for those who could find it helpful.
Alison Poulton, Senior Lecturer, Brain Mind Centre Nepean, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Somatic Exercises For Nervous System Regulation – by Rose Kilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about the vagus nerve, its importance, and how to make use of it, but it’s easy to let it slip from one’s mind when it comes to exercises. This book fixes that!
The promised 35 exercises are quite a range, and are organized into sections:
- Revitalizing through breath
- Stress and tension release
- Spinal and postural health
- Mindfulness and grounding
- Movements for flexibility
- Graceful balance and focus
While it’s not necessary to do all 35 exercises, it’s recommended to do at least some from each section, to “cover one’s bases”, and enjoy the best of all worlds.
The exercises are drawn from many sources, but tai chi and yoga are certainly the most well-represented. Others, meanwhile, are straight from physiotherapy or are things one might expect to be advised at a neurology consultation.
Bottom line: if you’d like to take better care of your vagus nerve, the better for it to take care of you, this book can certainly help with that.
Click here to check out Somatic Exercises For Nervous System Regulation, and take care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: