The Comfort Book – by Matt Haig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book “is what it says on the tin”. Matt Haig, bestselling author of “Reasons to Stay Alive” (amongst other works) is here with “a hug in a book”.
The format of the book is an “open it at any page and you’ll find something of value” book. Its small chapters are sometimes a few pages long, but often just a page. Sometimes just a line. Always deep.
All of us, who live long enough, will ponder our mortality sometimes. The feelings we may have might vary on a range from “afraid of dying” to “despairing of living”… but Haig’s single biggest message is that life is full of wonder; each moment precious.
- That hope is an incredible (and renewable!) resource.
- That we are more than a bad week, or month, or year, or decade.
- That when things are taken from us, the things that remain have more value.
Bottom line: you might cry (this reviewer did!), but it’ll make your life the richer for it, and remind you—if ever you need it—the value of your amazing life.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anti-Aging Myths This Dermatologist Wants You To Stop Believing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dermatologist Dr. Sam Ellis lays all bare:
Bare-faced lies?
Obviously, we are hearing from a dermatologist here, so the focus is on skin aging specifically. We may well also not want to age our brain, joints, etc, but that’s not what this one is about.
So, without further ado, here are the myths she wants to bust:
- “Medical grade skincare”: the term “medical grade” is a marketing term and does not indicate superior efficacy or better ingredients.
- “Expensive skincare is more effective”: price does not always correlate with effectiveness; some high-end products justify their cost, but many do not.
- “More products = better results”: using too many products can reduce effectiveness and cause irritation; a simple routine with sunscreen and a retinoid is key.
- “Drink more water for better skin”: if you’re dehydrated, then yes, hydrate—but drinking excessive water does not improve skin appearance beyond normal hydration levels.
- “You don’t need anti-aging products until you see signs of aging”: starting skincare early, especially sun protection, helps maintain youthful skin longer.
- “Wrinkles are the first signs of aging”: hyperpigmentation and sagging are often more significant early indicators of aging than wrinkles.
- “Skincare is all you need for anti-aging”: by “skincare” here she means creams, lotions, tonics, etc, and recommends other treatments such as laser treatment and even Botox*.
- “Non-prescription retinoids are a waste of time”: over-the-counter retinoids like retinol and retinal can still be effective alternatives to prescription retinoids.
- “You must use retinoids every night”: retinoids are effective even when used a few times per week, depending on individual tolerance.
*We’re not convinced about the Botox; we’ll have to do a deep-dive research review one of these days!
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Retinoids: Retinol vs Retinal vs Retinoic Acid vs..?
Take care!
Share This Post
-
5 Stretches To Relieve The Pain From Sitting & Poor Posture
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sitting is not good for the health, yes often it’s a necessity of modern life, especially if driving. To make things worse, it can often be difficult to remember to maintain good posture the rest of the time, if it’s not a habit. So, while reducing sitting and improving posture are both very good things to do, here are 5 stretches to mitigate the damage meanwhile:
Daily doses:
These are best done at a rate of 2–3 sets daily:
Cat-Cow Stretch:
- Benefits: eases spinal tension, boosts flexibility, improves posture.
- How to: start on all fours, alternate between arching and rounding your back while syncing with your breath (10-15 times).
Butterfly Stretch:
- Benefits: loosens tight hips, improves lower back flexibility, and enhances mobility for activities like squats.
- How to: sit with soles of feet together, let knees fall toward the floor, lean forward slightly, and hold for 30 seconds to 1 minute.
Supine Twist:
- Benefits: unlocks the spine, relieves post-workout tension, and relaxes the shoulders and hips.
- How to: lie on your back, bend knees, twist to one side while keeping shoulders grounded, and hold for 30 seconds to 1 minute per side.
Calf Stretch:
- Benefits: improves ankle mobility, loosens tight calves, and prevents injuries like Achilles tendinitis.
- How to: stand facing a wall, extend one leg back with the heel on the ground, lean into the stretch, or use a step for deeper stretches. Hold for 30 seconds to 1 minute per leg.
Child’s Pose:
- Benefits: decompresses the spine, relaxes hips, and relieves tension in back and thighs.
- How to: start on hands and knees, sit back onto your heels, stretch arms forward, and rest forehead on the mat. Hold for 30 seconds to 1 minute.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
10 Tips To Reduce Morning Pain & Stiffness With Arthritis
Take care!
Share This Post
-
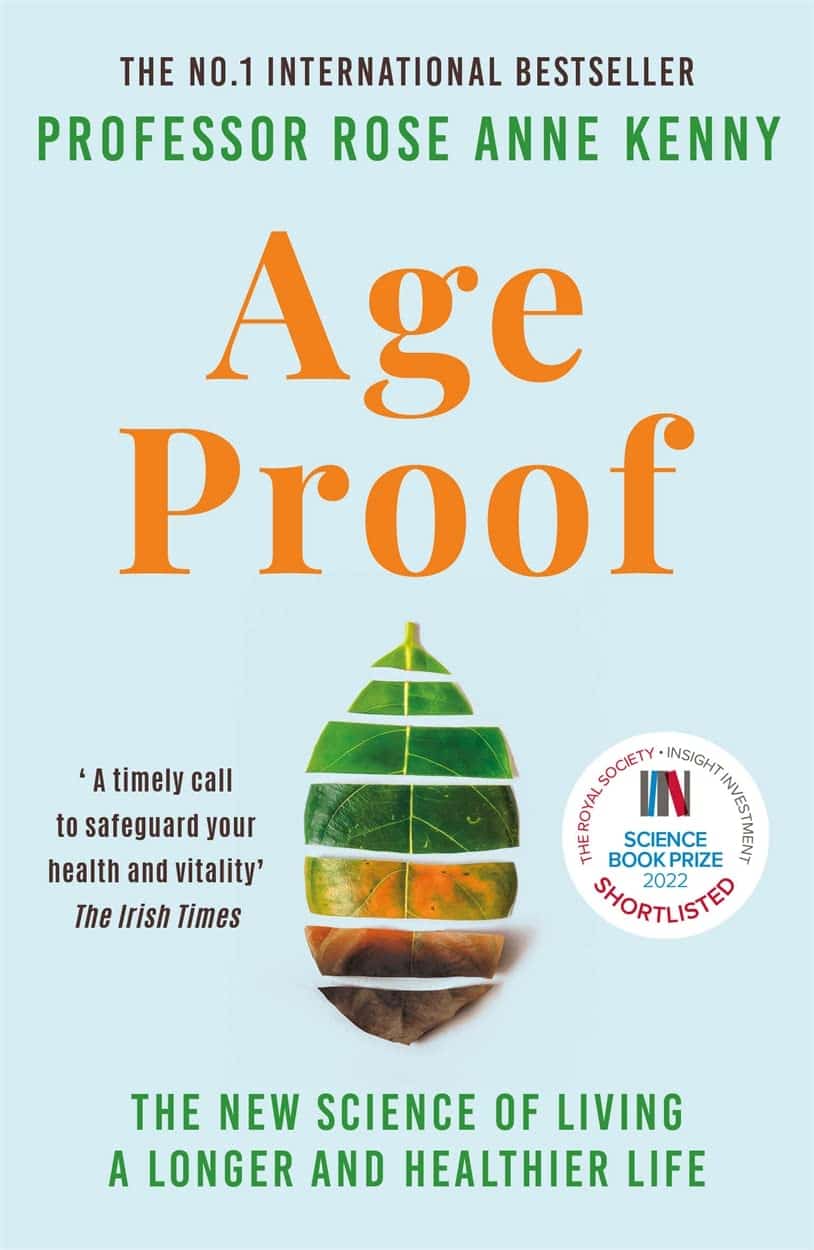
Age Proof – by Dr. Rose Anne Kenny
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t generally include an author bio, but in this case it’s worth noting that Dr. Kenny, the Chair of Medical Gerontology at Trinity College Dublin, with over 300 staff under her, has 704 peer-reviewed publications to her name, and enough awards and honors and achievements to more than fill a page on her university’s website.
In short, she knows her stuff.
A lot of the material in this book will not be completely new to regular 10almonds readers; there’s a lot about Blue Zones supercentenarians, the usual qualities associated with healthy longevity in those places (diet, lifestyle, etc), as well as genetic factors and epigenetic, and so forth.
Some items are… Not new, but not so commonly focused on in such works; for example, Dr. Kenny devotes a chapter to sleep, a chapter to laughter, a chapter to hormesis, and a chapter to sexual activity, amongst others.
Another thing she delivers that a lot of books of this kind don’t is that she has a collection of “Test Yourself” appendices, so that you can establish where you are relative to various benchmarks of aging.
Dr. Kenny also references her own work especially with TILDA (The Irish Longitudinal Study on Aging) that she has directed for many years, which has a vast amount of data and many important findings, which adds another extra strength to this book often not found in others.
The style is surprisingly personal, making it an enjoyable read as well as an educational one, and yet with a lot of hard science throughout—explained well for the layperson though, and thoroughly referenced with an extensive bibliography.
Bottom line: if you’d like to be (and continue to be!) “young for your years”, then this is an excellent book to get (and/or keep) you on the right track.
Share This Post
Related Posts
-
The Bare-Bones Truth About Osteoporosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
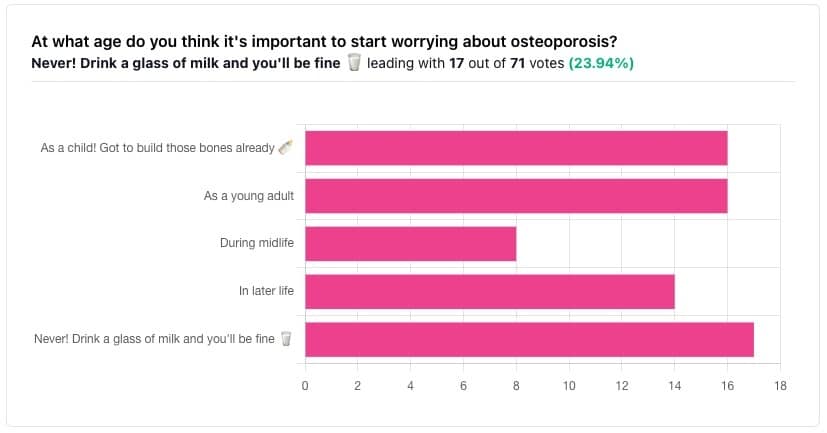
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
The Bare-bones Truth About Osteoporosis
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
At first glance it may seem shocking that a majority of respondents to a poll in a health-focused newsletter think it’ll never be an issue worth worrying about, but in fact this is partly a statistical quirk, because the vote of the strongest “early prevention” crowd was divided between “as a child” and “as a young adult”.
This poll also gave you the option to add a comment with your vote. Many subscribers chose to do so, explaining your choices… But, interestingly, not one single person who voted for “never” had any additional thoughts to add.
We loved reading your replies, by the way, and wish we had room to include them here, because they were very interesting and thought-provoking.
Let’s get to the myths and facts:
Top myth: “you will never need to worry about it; drink a glass of milk and you’ll be fine!”
The body is constantly repairing itself. Its ability to do that declines with age. Until about 35 on average, we can replace bone mineral as quickly as it is lost. After that, we lose it by up to 1% per year, and that rate climbs after 50, and climbs even more steeply for those who go through (untreated) menopause.
Losing 1% per year might not seem like a lot, but if you want to live to 100, there are some unfortunate implications!
About that menopause, by the way… Because declining estrogen levels late in life contribute significantly to osteoporosis, hormone replacement therapy (HRT) may be of value to many for the sake of bone health, never mind the more obvious and commonly-sought benefits.
On the topic of that glass of milk…
- Milk is a great source of calcium, which is useless to the body if you don’t also have good levels of vitamin D and magnesium.
- People’s vitamin D levels tend to directly correlate to the level of sun where they live, if supplementation isn’t undertaken.
- Plant-based milks are usually fortified with vitamin D (and calcium), by the way.
- Most people are deficient in magnesium, because green leafy things don’t form as big a part of most people’s diets as they should.
See also: An update on magnesium and bone health
Next most common myth: “bone health is all about calcium”
We spoke a little above about the importance of vitamin D and magnesium for being able to properly use that. But potassium is also critical:
Read more: The effects of potassium on bone health
While we’re on the topic…
People think of collagen as being for skin health. And it is important for that, but collagen’s benefits (and the negative effects of its absence) go much deeper, to include bone health. We’ve written about this before, so rather than take more space today, we’ll just drop the link:
We Are Such Stuff As Fish Are Made Of
Want to really maximize your bone health?
You might want to check out this well-sourced LiveStrong article:
Bone Health: Best and Worst Foods
(Teaser: leafy greens are in 2nd place, topped by sardines at #1—where do you think milk ranks?)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Diet Compass – by Bas Kast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Facts about nutrition and health can be hard to memorize. There’s just so much! And often there are so many studies, and while the science is not usually contradictory, pop-science headlines sure can be. What to believe?
Bas Kast brings us a very comprehensive and easily digestible solution.
A science journalist himself, he has gone through the studies so that you don’t have to, and—citing them along the way—draws out the salient points and conclusions.
But, he’s not just handing out directions (though he does that too); he’s arranged and formatted the information in a very readable and logical fashion. Chapter by chapter, we learn the foundations of important principles for “this is better than that” choices in diet.
Most importantly, he lays out for us his “12 simple rules for healthy eating“, and they are indeed as simple as they are well-grounded in good science.
Bottom line: if you want “one easy-reading book” to just tell you how to make decisions about your diet, simply follow those rules and enjoy the benefits… Then this book is exactly that.
Click here to check out The Diet Compass and get your diet on the right track!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Practical Optimism – by Dr. Sue Varma
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about how to get your brain onto a more positive track (without toxic positivity), but there’s a lot more to be said than we can fit into an article, so here’s a whole book packed full with usable advice.
The subtitle claims “the art, science, and practice of…”, but mostly it’s the science of. If there’s art to be found here, then this reviewer missed it, and as for the practice of, well, that’s down to the reader, of course.
However, it is easy to use the contents of this book to translate science into practice without difficulty.
If you’re a fan of acronyms, initialisms, and other mnemonics (such as the rhyming “Name, Claim, Tame, and Reframe”), then you’ll love this book as they come thick and fast throughout, and they contribute to the overall ease of application of the ideas within.
The writing style is conversational but with enough clinical content that one never forgets who is speaking—not in the egotistical way that some authors do, but rather, just, she has a lot of professional experience to share and it shows.
Bottom line: if you’d like to be more optimistic without delving into the delusional, this book can really help a lot with that (in measurable ways, no less!).
Click here to check out Practical Optimism, and brighten up your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: