Teen Daily Delivery Requested
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I thoroughly enjoy your daily delivery. I’d love to see one for teens too!
That’s great to hear! The average age of our subscribers is generally rather older, but it’s good to know there’s an interest in topics for younger people. We’ll bear that in mind, and see what we can do to cater to that without alienating our older readers!
That said: it’s never too soon to be learning about stuff that affects us when we’re older—there are lifestyle factors at 20 that affect Alzheimer’s risk at 60, for example (e.g. drinking—excessive drinking at 20* is correlated to higher Alzheimer’s risk at 60).
*This one may be less of an issue for our US readers, since the US doesn’t have nearly as much of a culture of drinking under 21 as some places. Compare for example with general European practices of drinking moderately from the mid-teens, or the (happily, diminishing—but historically notable) British practice of drinking heavily from the mid-teens.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
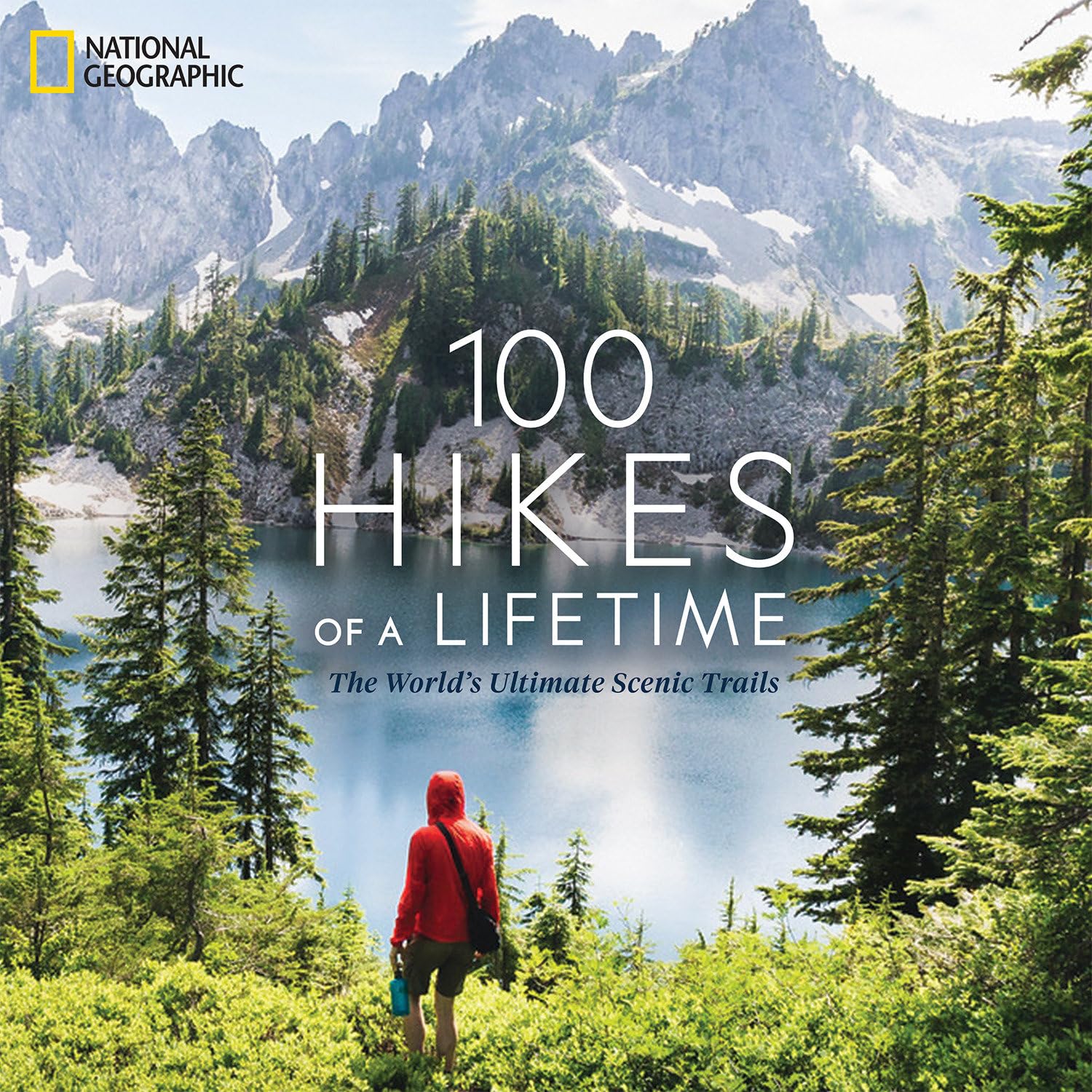
100 Hikes of a Lifetime – by Kate Siber
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is published by National Geographic, so you can imagine the quality of the photos throughout.
Inside, and after a general introduction and guide to gear and packing appropriately, it’s divided into continents, with a diverse array of “trips of a lifetime” for anyone who enjoys hiking.
It’s not a narrative book, rather, it is a guide, a little in the style of “Lonely Planet”, with many “know before you go” tips, information about the best time to go, difficult level, alternative routes if you want to get most of the enjoyment while having an easier time of it (or, conversely, if you want to see some extra sights along the way), and what to expect at all points.
Where the book really excels is in balancing inspiration with information. There are some books that make you imagine being in a place, but you’ll never actually go there. There are other books that are technical manuals but not very encouraging. This one does both; it provides the motivation and the “yes, you really can, here’s how” information that, between them, can actually get you packing and on your way.
Bottom line: if you yearn for breathtaking views and time in the great outdoors, but aren’t sure where to start, this will give you an incredible menu to choose from, and give you the tools to go about doing it.
Click here to check out 100 Hikes Of A Lifetime, and live it!
Share This Post
-
One Critical Mistake That Costs Seniors Their Mobility
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Will Harlow, the over-50s specialist physio, advises what to do instead:
Nose over toes
Often considered the most important test of mobility in later life (or in general, but later life is when it tends to decline) is the ability to get up off the floor without using your arms.
Many seniors, meanwhile, struggle to get out of a chair without using their arms.
Now, sitting in chairs in the first place is not good for the health, but that’s another matter and beyond the scope of today’s article.
If, perchance, you struggle to get up from a chair (especially if it’s low/deep, like many armchairs are) without using your hands, then here’s the way to do it:
- While practicing, cross your arms in front of you, so that you cannot use them.
- Shuffle yourself towards the front of the chair. No, don’t use your arms for this either, do a little butt-walk instead, to get you to the front edge of the chair.
- Lean forwards to position your nose over your toes (hence the mnemonic: “nose over toes”; memorize that!), as this will put your center of gravity where it needs to be.
- Now, push with your feet to rise up and forwards; slowly is better than quickly (quickly may be easier, but slowly will improve your strength and balance).
For more on all of this plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
We looked at over 166,000 psychiatric records. Over half showed people were admitted against their will
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Picture two people, both suffering from a serious mental illness requiring hospital admission. One was born in Australia, the other in Asia.
Hopefully, both could be treated on a voluntary basis, taking into account their individual needs, preferences and capacity to consent. If not, you might imagine they should be equally likely to receive treatment against their will (known colloquially as being “sectioned” or “scheduled”).
However, our research published in British Journal of Psychiatry Open suggests this is not the case.
In the largest study globally of its kind, we found Australians are more likely to be treated in hospital for their acute mental illness against their will if they are born overseas, speak a language other than English or are unemployed.
What we did and what we found
We examined more than 166,000 episodes of voluntary and involuntary psychiatric care in New South Wales public hospitals between 2016 and 2021. Most admissions (54%) included at least one day of involuntary care.
Being brought to hospital via legal means, such as by police or via a court order, was strongly linked to involuntary treatment.
While our study does not show why this is the case, it may be due to mental health laws. In NSW, which has similar laws to most jurisdictions in Australia, doctors may treat a person on an involuntary basis if they present with certain symptoms indicating serious mental illness (such as hallucinations and delusions) which cause them to require protection from serious harm, and there is no other less-restrictive care available. Someone who has been brought to hospital by police or the courts may be more likely to meet the legal requirement of requiring protection from serious harm.
The likelihood of involuntary care was also linked to someone’s diagnosis. A person with psychosis or organic brain diseases, such as dementia and delirium, were about four times as likely to be admitted involuntarily compared to someone with anxiety or adjustment disorders (conditions involving a severe reaction to stressors).
However, our data suggest non-clinical factors contribute to the decision to impose involuntary care.
Compared with people born in Australia, we found people born in Asia were 42% more likely to be treated involuntarily.
People born in Africa or the Middle East were 32% more likely to be treated this way.
Overall, people who spoke a language other than English were 11% more likely to receive involuntary treatment compared to those who spoke English as their first language.
Some international researchers have suggested higher rates of involuntary treatment seen in people born overseas might be due to higher rates of psychotic illness. But our research found a link between higher rates of involuntary care in people born overseas or who don’t speak English regardless of their diagnosis.
We don’t know why this is happening. It is likely to reflect a complex interplay of factors about both the people receiving treatment and the way services are provided to them.
People less likely to be treated involuntarily included those who hold private health insurance, and those referred through a community health centre or outpatients unit.
Our findings are in line with international studies. These show higher rates of involuntary treatment among people from Black and ethnic minority groups, and people living in areas of higher socioeconomic disadvantage.
A last resort? Or should we ban it?
Both the NSW and Australian mental health commissions have called involuntary psychiatric care an avoidable harm that should only be used as a last resort.
Despite this, one study found Australia’s rate of involuntary admissions has increased by 3.4% per year and it has one of the highest rates of involuntary admissions in the world.
Involuntary psychiatric treatment is also under increasing scrutiny globally.
When Australia signed up to the UN Convention on the Rights of Persons with Disabilities, it added a declaration noting it would allow for involuntary treatment of people with mental illness where such treatments are “necessary, as a last resort and subject to safeguards”.
However, the UN has rejected this, saying it is a fundamental human right “to be free from involuntary detention in a mental health facility and not to be forced to undergo mental health treatment”.
Others question if involuntary treatment could ever be removed entirely.
Where to from here?
Our research not only highlights concerns regarding how involuntary psychiatric treatment is implemented, it’s a first step towards decreasing its use. Without understanding how and when it is used it will be difficult to create effective interventions to reduce it.
But Australia is still a long way from significantly reducing involuntary treatment.
We need to provide more care options outside hospital, ones accessible to all Australians, including those born overseas, who don’t speak English, or who come from disadvantaged communities. This includes intervening early enough that people are supported to not become so unwell they end up being referred for treatment via police or the criminal justice system.
More broadly, we need to do more to reduce stigma surrounding mental illness and to ensure poverty and discrimination are tackled to help prevent more people becoming unwell in the first place.
Our study also shows we need to do more to respect the autonomy of someone with serious mental illness to choose if they are treated. That’s whether they are in NSW or other jurisdictions.
And legal reform is required to ensure more states and territories more fully reflect the principal that people who have the capacity to make such decisions should have the right to decline mental health treatment in the same way they would any other health care.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Amy Corderoy, Medical doctor and PhD candidate studying involuntary psychiatric treatment, School of Psychiatry, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
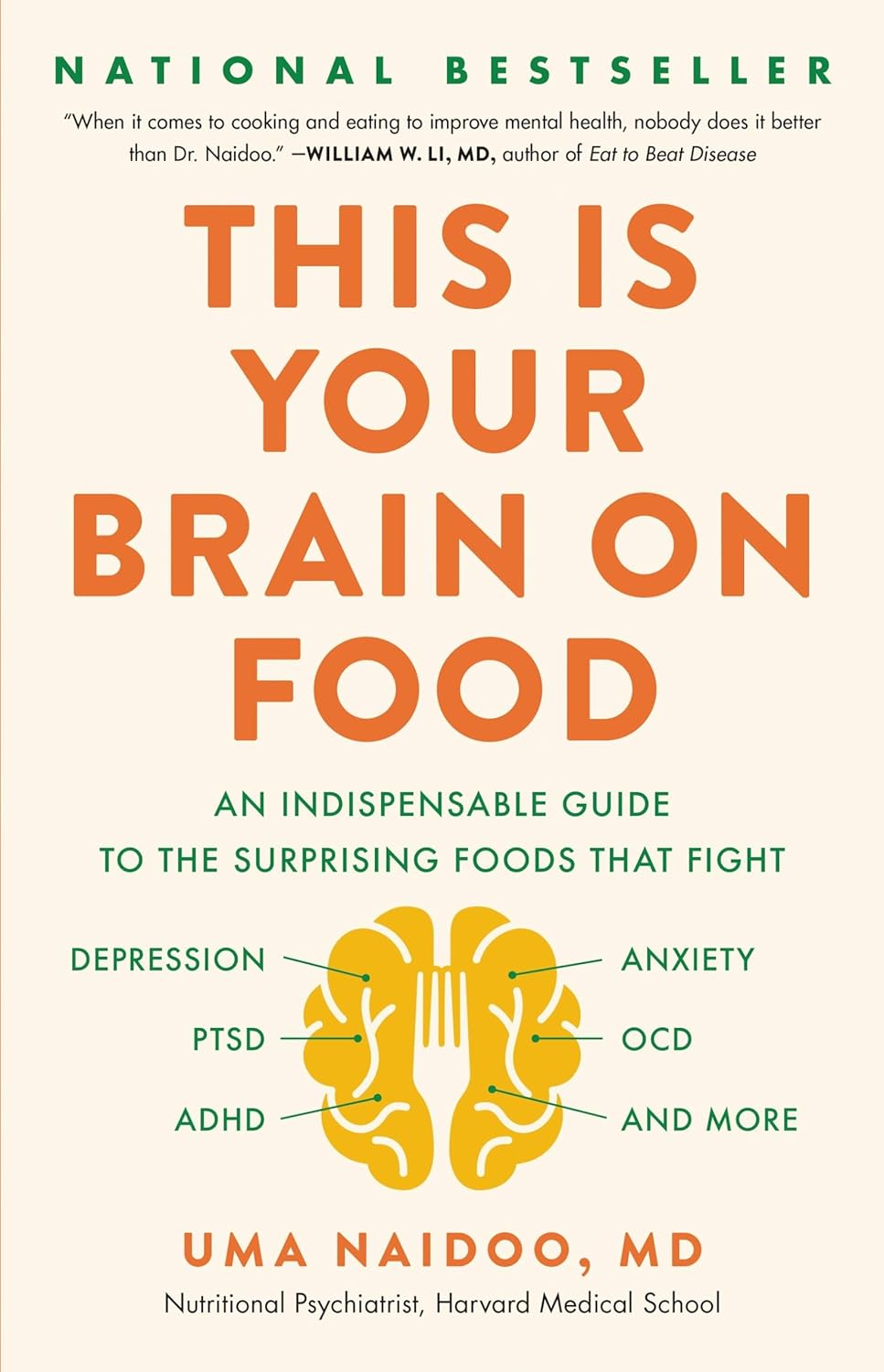
This Is Your Brain on Food – by Dr. Uma Naidoo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Diet will fix your brain” is a bold claim that often comes from wishful thinking and an optimistic place where anecdote is louder than evidence. But, diet does incontrovertibly also affect brain health. So, what does Dr. Naidoo bring to the table?
The author is a Harvard-trained psychiatrist, a professional chef who graduated with her culinary school’s most coveted award, and a trained-and-certified nutritionist. Between those three qualifications, it’s safe to she knows her stuff when it comes to the niche that is nutritional psychiatry. And it shows.
She takes us through the neurochemistry involved, what chemicals are consumed, made, affected, inhibited, upregulated, etc, what passes through the blood-brain barrier and what doesn’t, what part the gut really plays in its “second brain” role, and how we can leverage that—as well as mythbusting a lot of popular misconceptions about certain foods and moods.
There’s hard science in here, but presented in quite a pop-science way, making for a very light yet informative read.
Bottom line: if you’d like to better understand what your food is doing to your brain (and what it could be doing instead), then this is a top-tier book for you!
Click here to check out This Is Your Brain On Food, and get to know yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why do I need to take some medicines with food?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have you ever been instructed to take your medicine with food and wondered why? Perhaps you’ve wondered if you really need to?
There are varied reasons, and sometimes complex science and chemistry, behind why you may be advised to take a medicine with food.
To complicate matters, some similar medicines need to be taken differently. The antibiotic amoxicillin with clavulanic acid (sold as Amoxil Duo Forte), for example, is recommended to be taken with food, while amoxicillin alone (sold as Amoxil), can be taken with or without food.
Different brands of the same medicine may also have different recommendations when it comes to taking it with food.
Ron Lach/Pexels Food impacts drug absorption
Food can affect how fast and how much a drug is absorbed into the body in up to 40% of medicines taken orally.
When you have food in your stomach, the makeup of the digestive juices change. This includes things like the fluid volume, thickness, pH (which becomes less acidic with food), surface tension, movement and how much salt is in your bile. These changes can impair or enhance drug absorption.
Eating a meal also delays how fast the contents of the stomach move into the small intestine – this is known as gastric emptying. The small intestine has a large surface area and rich blood supply – and this is the primary site of drug absorption.
Eating a meal with medicine will delay its onset. Farhad/Pexels Eating a larger meal, or one with lots of fibre, delays gastric emptying more than a smaller meal. Sometimes, health professionals will advise you to take a medicine with food, to help your body absorb the drug more slowly.
But if a drug can be taken with or without food – such as paracetamol – and you want it to work faster, take it on an empty stomach.
Food can make medicines more tolerable
Have you ever taken a medicine on an empty stomach and felt nauseated soon after? Some medicines can cause stomach upsets.
Metformin, for example, is a drug that reduces blood glucose and treats type 2 diabetes and polycystic ovary syndrome. It commonly causes gastrointestinal symptoms, with one in four users affected. To combat these side effects, it is generally recommended to be taken with food.
The same advice is given for corticosteroids (such as prednisolone/prednisone) and certain antibiotics (such as doxycycline).
Taking some medicines with food makes them more tolerable and improves the chance you’ll take it for the duration it’s prescribed.
Can food make medicines safer?
Ibuprofen is one of the most widely used over-the-counter medicines, with around one in five Australians reporting use within a two-week period.
While effective for pain and inflammation, ibuprofen can impact the stomach by inhibiting protective prostaglandins, increasing the risk of bleeding, ulceration and perforation with long-term use.
But there isn’t enough research to show taking ibuprofen with food reduces this risk.
Prolonged use may also affect kidney function, particularly in those with pre-existing conditions or dehydration.
The Australian Medicines Handbook, which guides prescribers about medicine usage and dosage, advises taking ibuprofen (sold as Nurofen and Advil) with a glass of water – or with a meal if it upsets your stomach.
If it doesn’t upset your stomach, ibuprofen can be taken with water. Tbel Abuseridze/Unsplash A systematic review published in 2015 found food delays the transit of ibuprofen to the small intestine and absorption, which delays therapeutic effect and the time before pain relief. It also found taking short courses of ibuprofen without food reduced the need for additional doses.
To reduce the risk of ibuprofen causing damage to your stomach or kidneys, use the lowest effective dose for the shortest duration, stay hydrated and avoid taking other non-steroidal anti-inflammatory medicines at the same time.
For people who use ibuprofen for prolonged periods and are at higher risk of gastrointestinal side effects (such as people with a history of ulcers or older adults), your prescriber may start you on a proton pump inhibitor, a medicine that reduces stomach acid and protects the stomach lining.
How much food do you need?
When you need to take a medicine with food, how much is enough?
Sometimes a full glass of milk or a couple of crackers may be enough, for medicines such as prednisone/prednisolone.
However, most head-to-head studies that compare the effects of a medicine “with food” and without, usually use a heavy meal to define “with food”. So, a cracker may not be enough, particularly for those with a sensitive stomach. A more substantial meal that includes a mix of fat, protein and carbohydrates is generally advised.
Your health professional can advise you on which of your medicines need to be taken with food and how they interact with your digestive system.
Mary Bushell, Clinical Associate Professor in Pharmacy, University of Canberra
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Elderhood – by Dr. Louise Aronson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Where does “middle age” end, and “old age” begin? By the United States’ CDC’s categorization, human life involves:
- 17 stages of childhood, deemed 0–18
- 5 stages of adulthood, deemed 18–60
- 1 stage of elderhood, deemed 60+
Isn’t there something missing here? Do we just fall off some sort of conveyor belt on our sixtieth birthdays, into one big bucket marked “old”?
Yesterday you were 59 and enjoying your middle age; today you have, apparently, the same medical factors and care needs as a 114-year-old.
Dr. Louise Aronson, a geriatrician, notes however that medical science tends to underestimate the differences found in more advanced old age, and underresearch them. That elders consume half of a country’s medicines, but are not required to be included in clinical trials. That side effects not only are often different than for younger adults, but also can cause symptoms that are then dismissed as “Oh she’s just old”.
She explores, mostly through personal career anecdotes, the well-intentioned disregard that is frequently given by the medical profession, and—importantly—how we might overcome that, as individuals and as a society.
Bottom line: if you are over the age of 60, love someone over the age of 60, this is a book for you. Similarly if you and/or they plan to live past the age of 60, this is also a book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: