Starfruit vs Soursop – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing starfruit to soursop, we picked the soursop.
Why?
First, by starfruit, we also mean carambola, which is a different name for the same fruit, and by soursop we also mean graviola/guyabano/guanábana, which are different namers for the same fruit. Now, as for their health qualities:
In terms of macros, the soursop has more carbs and fiber, the ratio of which also give it the lower glycemic index. So, a win for soursop here.
When it comes to vitamins, starfruit has more of vitamins A, B5, C, and E, while soursop has more of vitamins B1, B2, B3, B6, B7, B9, and K. Another win for soursop.
In the category of minerals, starfruit has slightly more copper, manganese, and zinc, while soursop has much more calcium, iron, magnesium, phosphorus, and potassium. One more win for soursop!
Adding up the sections makes for a clear and overwhelming win for soursop, but let’s address to quick safety considerations while we’re here:
- Soursop extract has been claimed to be an effective cancer treatment. It isn’t. There is no evidence for this at all; just one unscrupulous company that spread the claims.
- Soursop contains annonacin, a neurotoxin. That sounds scary, but much like with apple seeds and cyanide, the quantities you’d have to consume to suffer ill effects are absurd. Remember how capsaicin (as found in hot peppers) is also a neurotoxin, too and has many health benefits. Humans have a long and happy tradition of enjoying things that are toxic at high doses, but in small doses are neutral or even beneficial. Pretty much all things we can consume (including oxygen, and water) are toxic at sufficient doses.
In short, both of these fruits are fine and good, neither will treat cancer, but both will help to keep you in good health. As for nutritional density, the soursop wins in every category.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← soursop has no special cancer treatment properties, but actual evidence shows these fruits are beneficial (being good as a preventative, and also definitely a worthy adjunct to—but not a replacement for—mainstream anticancer therapies if you have cancer).
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Taking A Trip Through The Evidence On Psychedelics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
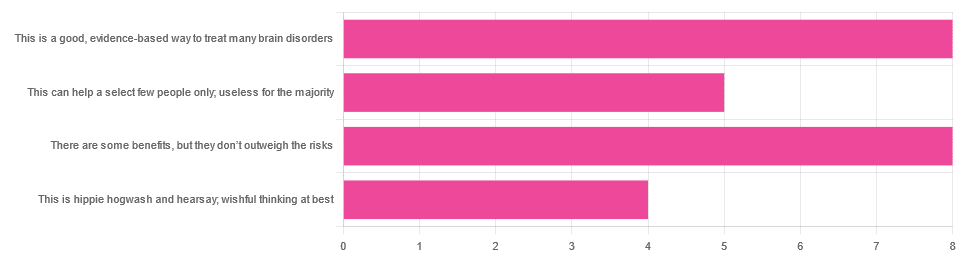
In Tuesday’s newsletter, we asked you for your opinions on the medicinal use of psychedelics, and got the above-depicted, below-described, set of responses:
- 32% said “This is a good, evidence-based way to treat many brain disorders”
- 32% said “There are some benefits, but they don’t outweigh the risks”
- 20% said “This can help a select few people only; useless for the majority”
- 16% said “This is hippie hogwash and hearsay; wishful thinking at best”
Quite a spread of answers, so what does the science say?
This is hippie hogwash and hearsay; wishful thinking at best! True or False?
False! We’re tackling this one first, because it’s easiest to answer:
There are some moderately-well established [usually moderate] clinical benefits from some psychedelics for some people.
If that sounds like a very guarded statement, it is. Part of this is because “psychedelics” is an umbrella term; perhaps we should have conducted separate polls for psilocybin, MDMA, ayahuasca, LSD, ibogaine, etc, etc.
In fact: maybe we will do separate main features for some of these, as there is a lot to say about each of them separately.
Nevertheless, looking at the spread of research as it stands for psychedelics as a category, the answers are often similar across the board, even when the benefits/risks may differ from drug to drug.
To speak in broad terms, if we were to make a research summary for each drug it would look approximately like this in each case:
- there has been research into this, but not nearly enough, as “the war on drugs” may well have manifestly been lost (the winner of the war being: drugs; still around and more plentiful than ever), but it did really cramp science for a few decades.
- the studies are often small, heterogenous (often using moderately wealthy white student-age population samples), and with a low standard of evidence (i.e. the methodology often has some holes that leave room for reasonable doubt).
- the benefits recorded are often small and transient.
- in their favor, though, the risks are also generally recorded as being quite low, assuming proper safe administration*.
*Illustrative example:
Person A takes MDMA in a club, dances their cares away, has had only alcohol to drink, sweats buckets but they don’t care because they love everyone and they see how we’re all one really and it all makes sense to them and then they pass out from heat exhaustion and dehydration and suffer kidney damage (not to mention a head injury when falling) and are hospitalized and could die;
Person B takes MDMA in a lab, is overwhelmed with a sense of joy and the clarity of how their participation in the study is helping humanity; they want to hug the researcher and express their gratitude; the researcher reminds them to drink some water.
Which is not to say that a lab is the only safe manner of administration; there are many possible setups for supervised usage sites. But it does mean that the risks are often as much environmental as they are risks inherent to the drug itself.
Others are more inherent to the drug itself, such as adverse cardiac events for some drugs (ibogaine is one that definitely needs medical supervision, for example).
For those who’d like to see numbers and clinical examples of the bullet points we gave above, here you go; this is a great (and very readable) overview:
NIH | Evidence Brief: Psychedelic Medications for Mental Health and Substance Use Disorders
Notwithstanding the word “brief” (intended in the sense of: briefing), this is not especially brief and is rather an entire book (available for free, right there!), but we do recommend reading it if you have time.
This can help a select few people only; useless for the majority: True or False?
True, technically, insofar as the evidence points to these drugs being useful for such things as depression, anxiety, PTSD, addiction, etc, and estimates of people who struggle with mental health issues in general is often cited as being 1 in 4, or 1 in 5. Of course, many people may just have moderate anxiety, or a transient period of depression, etc; many, meanwhile, have it worth.
In short: there is a very large minority of people who suffer from mental health issues that, for each issue, there may be one or more psychedelic that could help.
This is a good, evidence-based way to treat many brain disorders: True or False?
True if and only if we’re willing to accept the so far weak evidence that we discussed above. False otherwise, while the jury remains out.
One thing in its favor though is that while the evidence is weak, it’s not contradictory, insofar as the large preponderance of evidence says such therapies probably do work (there aren’t many studies that returned negative results); the evidence is just weak.
When a thousand scientists say “we’re not completely sure, but this looks like it helps; we need to do more research”, then it’s good to believe them on all counts—the positivity and the uncertainty.
This is a very different picture than we saw when looking at, say, ear candling or homeopathy (things that the evidence says simply do not work).
We haven’t been linking individual studies so far, because that book we linked above has many, and the number of studies we’d have to list would be:
n = number of kinds of psychedelic drugs x number of conditions to be treated
e.g. how does psilocybin fare for depression, eating disorders, anxiety, addiction, PTSD, this, that, the other; now how does ayahuasca fare for each of those, and so on for each drug and condition; at least 25 or 30 as a baseline number, and we don’t have that room.
But here are a few samples to finish up:
- Psilocybin as a New Approach to Treat Depression and Anxiety in the Context of Life-Threatening Diseases—A Systematic Review and Meta-Analysis of Clinical Trials
- Therapeutic Use of LSD in Psychiatry: A Systematic Review of Randomized-Controlled Clinical Trials
- Efficacy of Psychoactive Drugs for the Treatment of Posttraumatic Stress Disorder: A Systematic Review of MDMA, Ketamine, LSD and Psilocybin
- Changes in self-rumination and self-compassion mediate the effect of psychedelic experiences on decreases in depression, anxiety, and stress.
- Psychedelic Treatments for Psychiatric Disorders: A Systematic Review and Thematic Synthesis of Patient Experiences in Qualitative Studies
- Repeated lysergic acid diethylamide (LSD) reverses stress-induced anxiety-like behavior, cortical synaptogenesis deficits and serotonergic neurotransmission decline
In closing…
The general scientific consensus is presently “many of those drugs may ameliorate many of those conditions, but we need a lot more research before we can say for sure”.
On a practical level, an important take-away from this is twofold:
- drugs, even those popularly considered recreational, aren’t ontologically evil, generally do have putative merits, and have been subject to a lot of dramatization/sensationalization, especially by the US government in its famous war on drugs.
- drugs, even those popularly considered beneficial and potentially lifechangingly good, are still capable of doing great harm if mismanaged, so if putting aside “don’t do drugs” as a propaganda of the past, then please do still hold onto “don’t do drugs alone”; trained professional supervision is a must for safety.
Take care!
Share This Post
-
The Case Against Sugar – by Gary Taubes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We generally already know that sugar is bad for the health. Most people don’t know how bad.
Taubes makes, as the title goes, “the case against sugar”. Implicated in everything from metabolic syndrome to cancer to Alzheimer’s, sugar is ruinous to the health.
It’s hard to review this book without making a comparison to William Duffy’s 1975 bestseller, “Sugar Blues“. Stylistically it’s very similar, and the general gist is certainly the same.
However! Where this book beats Sugar Blues is in content; Duffy’s book often makes bold claims without scientific backing. Some of those claims didn’t stand the test of time and are now disproven. Instead, Taubes’ book leans on actual up-to-date science, and talks more about what we actually know, than what we imagine.
If this book has a weak point, it’s when it veers away from its main topic and starts talking about, for example, saturated fat. In this side-topic, the book makes some good points, but is less well-considered, cherry-picks data, and lacks nuance.
On its main topic, though, the investigation of sugar, it is rather more thorough.
Bottom line: if you want a next-level motivation to reduce or eliminate dietary sugar, this book may certainly provide that.
Click here to check out The Case Against Sugar and reduce a lot of your health risks!
Share This Post
-
You Are Not Broken – by Dr. Kelly Casperson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many women express “I think I’m broken down there”, and it turns out simply that neither they nor their partners had the right knowledge, that’s all. The good news is: bedroom competence is an entirely learnable skill!
Dr. Casperson is a urologist, and over the years has expanded her work into all things pelvic, including the relevant use of both systemic and topical hormones (as in, hormones to increase overall blood serum levels of that hormone, like most HRT, and also, creams and lotions to increase levels of a given hormone in one particular place).
However, this is not 200 pages to say “take hormones”. Rather, she covers many areas of female sexual health and wellbeing, including yes, simply pleasure. From the physiological to the psychological, Dr. Casperson talks the reader through avoiding blame games and “getting out of your head and into your body”.
Bottom line: if you (or a loved one) are one of the many women who have doubts about being entirely correctly set up down there, then this book is definitely for you.
Click here to check out You Are Not Broken, and indeed stop “should-ing” all over your sex life!
Share This Post
Related Posts
-
Where Nutrition Meets Habits!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Where Nutrition Meets Habits…
This is Claudia Canu, MSc., INESEM. She’s on a mission to change the way we eat:
Often, diet is a case of…
- Healthy
- Easy
- Cheap
(choose two)
She wants to make it all three, and tasty too. She has her work cut out for her, but she’s already blazed quite a trail personally:
❝Nine months before turning 40 years old, I set a challenge for myself: Arrive to the day I turn 40 as the best possible version of myself, physically, mentally and emotionally.❞
~ Claudia Canu
In Her Own Words: My Journey To My Healthy 40s
And it really was quite a journey:
- September: Changes That Destabilize
- October: Looking for Focus
- November: New Habits
- December: Analyzing The First Results
- January: Traveling & Perfectionism
- February: Habits & Goals
- March: Connection, Cravings, & Organization
- April: Physical & Emotional Changes After 7 Months
- May: Reflections & Considerations
- June: Challenge Is Over
For those of us who’d like the short-cut rather than a nine-month quasi-spiritual journey… based on both her experience, and her academic and professional background in nutrition, her main priorities that she settled on were:
- Making meals actually nutritionally balanced, which meant re-thinking what she thought a meal “should” be
- Making nutritionally balanced meals that didn’t require a lot of skill and/or resources
- That’s it!
But, easier said than done… Where to begin?
She shares an extensive list of recipes, from meals to snacks (I thought I was the only one who made coffee overnight oats!), but the most important thing from her is:
Claudia’s 10 Guiding Principles:
- Buy only fresh ingredients that you are going to cook yourself. If you decide to buy pre-cooked ones, make sure they do not have added ingredients, especially sugar (in all its forms).
- Use easy and simple cooking methods.
- Change ingredients every time you prepare your meals.
- Prepare large quantities for three or four days.
- Store the food separately in tightly closed Tupperware.
- Organize yourself to always have ready-to-eat food in the fridge.
- When hungry, mix the ingredients in the ideal amounts to cover the needs of your body.
- Chew well and take the time to taste your food.
- Eat foods that you like and enjoy.
- Do not overeat but don’t undereat either.
We have only two quibbles with this fine list, which are:
About Ingredients!
Depending on what’s available around you, frozen and/or tinned “one-ingredient” foods can be as nutritional as (if not more nutritional than) fresh ones. By “one-ingredient” foods here we mean that if you buy a frozen pack of chopped onions, the ingredients list will be: “chopped onions”. If you buy a tin of tomatoes, the ingredients will say “Tomatoes” or at most “Tomatoes, Tomato Juice”, for example.
She does list the ingredients she keeps in; the idea that with these in the kitchen, you’ll never be in the position of “oh, we don’t have much in, I guess it’s a pizza delivery night” or “well there are some chicken nuggets at the back of the freezer”.
Check Out And Plan: 10 Types Of Ingredients You Should Always Keep In Your Kitchen
Here Today, Gone Tomorrow?
Preparing large quantities for three or four days can result in food for one or two days if the food is unduly delicious
But! Claudia has a remedy for that:
Read: How To Eliminate Food Cravings And What To Do When They Win
Anyway, there’s a wealth of resources in the above-linked pages, so do check them out!
Perhaps the biggest take-away is to ask yourself:
“What are my guiding principles when it comes to food?”
If you don’t have a ready answer, maybe it’s time to tackle that—whether Claudia’s way or your own!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fasting, eating earlier in the day or eating fewer meals – what works best for weight loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, one in eight people are living with obesity. This is an issue because excess fat increases the risk of type 2 diabetes, heart disease and certain cancers.
Modifying your diet is important for managing obesity and preventing weight gain. This might include reducing your calorie intake, changing your eating patterns and prioritising healthy food.
But is one formula for weight loss more likely to result in success than another? Our new research compared three weight-loss methods, to see if one delivered more weight loss than the others:
- altering calorie distribution – eating more calories earlier rather than later in the day
- eating fewer meals
- intermittent fasting.
We analysed data from 29 clinical trials involving almost 2,500 people.
We found that over 12 weeks or more, the three methods resulted in similar weight loss: 1.4–1.8kg.
So if you do want to lose weight, choose a method that works best for you and your lifestyle.
chalermphon_tiam/Shutterstock Eating earlier in the day
When our metabolism isn’t functioning properly, our body can’t respond to the hormone insulin properly. This can lead to weight gain, fatigue and can increase the risk of a number of chronic diseases such as diabetes.
Eating later in the day – with a heavy dinner and late-night snacking – seems to lead to worse metabolic function. This means the body becomes less efficient at converting food into energy, managing blood sugar and regulating fat storage.
In contrast, consuming calories earlier in the day appears to improve metabolic function.
However, this might not be the case for everyone. Some people naturally have an evening “chronotype”, meaning they wake up and stay up later.
People with this chronotype appear to have less success losing weight, no matter the method. This is due to a combination of factors including genes, an increased likelihood to have a poorer diet overall and higher levels of hunger hormones.
Eating fewer meals
Skipping breakfast is common, but does it hinder weight loss? Or is a larger breakfast and smaller dinner ideal?
While frequent meals may reduce disease risk, recent studies suggest that compared to eating one to two meals a day, eating six times a day might increase weight loss success.
However, this doesn’t reflect the broader research, which tends to show consuming fewer meals can lead to greater weight loss. Our research suggests three meals a day is better than six. The easiest way to do this is by cutting out snacks and keeping breakfast, lunch and dinner.
Most studies compare three versus six meals, with limited evidence on whether two meals is better than three.
However, front-loading your calories (consuming most of your calories between breakfast and lunch) appears to be better for weight loss and may also help reduce hunger across the day. But more studies with a longer duration are needed.
Fasting, or time-restricted eating
Many of us eat over a period of more than 14 hours a day.
Eating late at night can throw off your body’s natural rhythm and alter how your organs function. Over time, this can increase your risk of type 2 diabetes and other chronic diseases, particularly among shift workers.
Time-restricted eating, a form of intermittent fasting, means eating all your calories within a six- to ten-hour window during the day when you’re most active. It’s not about changing what or how much you eat, but when you eat it.
Some people limit their calories to a six hour window, while others opt for ten hours. Shutterstock/NIKS ADS Animal studies suggest time-restricted eating can lead to weight loss and improved metabolism. But the evidence in humans is still limited, especially about the long-term benefits.
It’s also unclear if the benefits of time-restricted eating are due to the timing itself or because people are eating less overall. When we looked at studies where participants ate freely (with no intentional calorie limits) but followed an eight-hour daily eating window, they naturally consumed about 200 fewer calories per day.
What will work for you?
In the past, clinicians have thought about weight loss and avoiding weight gain as a simile equation of calories in and out. But factors such as how we distribute our calories across the day, how often we eat and whether we eat late at night may also impact our metabolism, weight and health.
There are no easy ways to lose weight. So choose a method, or combination of methods, that suits you best. You might consider
- aiming to eat in an eight-hour window
- consuming your calories earlier, by focusing on breakfast and lunch
- opting for three meals a day, instead of six.
The average adult gains 0.4 to 0.7 kg per year. Improving the quality of your diet is important to prevent this weight gain and the strategies above might also help.
Finally, there’s still a lot we don’t know about these eating patterns. Many existing studies are short-term, with small sample sizes and varied methods, making it hard to make direct comparisons.
More research is underway, including well-controlled trials with larger samples, diverse populations and consistent methods. So hopefully future research will help us better understand how altering our eating patterns can result in better health.
Hayley O’Neill, Assistant Professor, Faculty of Health Sciences and Medicine, Bond University and Loai Albarqouni, Assistant Professor | NHMRC Emerging Leadership Fellow, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bushfire smoke affects children differently. Here’s how to protect them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Bushfires are currently burning in Australian states including Victoria, Tasmania, Western Australia and South Australia. In some areas, fire authorities have warned residents about the presence of smoke.
Bushfire smoke is harmful to our health. Tiny particles of ash can lodge deep in the lungs.
Exposure to this type of smoke may worsen existing conditions such as asthma, and induce a range of health effects from irritation of the eyes, nose and throat to changes in the cardiovascular system.
Public health recommendations during smoke events tend to provide general advice, and don’t often include advice specifically geared at children. But children are not just little adults. They are uniquely vulnerable to environmental hazards such as bushfire smoke for a number of reasons.
Different physiology, different behaviour
Children’s lungs are still developing and maturing.
Airways are smaller in children, especially young children, which is associated with greater rates of particle deposition – when particles settle on the surfaces of the airways.
Children also breathe more air per kilogram of body weight compared with adults, and therefore inhale more polluted air relative to their size.
Further, children’s detoxification systems are still developing, so environmental toxins take longer to effectively clear from their bodies.
Meanwhile, children’s behaviour and habits may expose them to more environmental toxins than adults. For example, they tend to do more physical activity and spend more time outdoors. Higher levels of physical activity lead to more air inhaled per kilogram of body weight.
Also, a normal and important part of children’s early play is exploring their environment, including by putting things in their mouth. This can result in kids ingesting soil, dust and dirt, which often contain environmental contaminants.
For these reasons, it’s important to consider the specific needs of children when providing advice on what to do when there’s smoke in the air.
Keeping our environments healthy
The Australian government offers recommendations for minimising the health risks from exposure to bushfire smoke. The main advice includes staying indoors and keeping doors and windows closed.
This is great advice when the smoke is thick outside, but air pollutants may still accumulate inside the home. So it’s important to air your home once the smoke outside starts to clear. Take advantage of wind changes to open up and get air moving out of the house with a cross breeze.
Kids are natural scientists, so get them involved. For example, you and your child can “rate” the air each hour by looking at a landmark outside your home and rating how clearly you can see it. When you notice the haze is reducing, open up the house and clear the air.
Because air pollutants settle onto surfaces in our home and into household dust, an easy way to protect kids during smoky periods is to do a daily dust with a wet cloth and vacuum regularly. This will remove pollutants and reduce ingestion by children as they play. Frequent hand washing helps too.
Healthy bodies and minds
Research exploring the effects of bushfire smoke exposure on children’s health is sparse. However, during smoke events, we do see an increase in hospital visits for asthma, as well as children reporting irritation to their eyes, nose and throat.
If your child has asthma or another medical condition, ensure they take any prescribed medications on a regular schedule to keep their condition well controlled. This will minimise the risk of a sudden worsening of their symptoms with bushfire smoke exposure.
Make sure any action plans for symptom flare-ups are up to date, and ensure you have an adequate supply of in-date medication somewhere easy to locate and access.
Children may be anxious during a bushfire.
Media_Photos/ShutterstockKids can get worried during bushfires, and fire emergencies have been linked with a reduction in children’s mental health. Stories such as the Birdie’s Tree books can help children understand these events do pass and people help one another in times of difficulty.
Learning more about air pollution can help too. Our group has a children’s story explaining how air pollution affects our bodies and what can help.
It’s also important for parents and caregivers not to get too stressed, as children cope better when their parents manage their own anxiety and help their children do the same. Try to strike a balance between being vigilant and staying calm.
What about masks?
N95 masks can protect the wearer from fine particles in bushfire smoke, but their use is a bit complicated when it comes to kids. Most young children won’t be able to fit properly into an N95 mask, or won’t tolerate the tight fit for long periods. Also, their smaller airways make it harder for young children to breathe through a mask.
If you choose to use an N95 mask for your children, it’s best to save them for instances when high-level outdoor exposure is unavoidable, such as if you’re going outside when the smoke is very thick.
N95 masks should be replaced after around four hours or when they become damp.
If your child has an existing heart or lung condition, consult their doctor before having them wear an N95 mask.
Our team is currently recruiting for a study exploring the effects of bushfire smoke in children. If you live in south east Queensland and are interested in participating in the event of a bushfire or hazard reduction burn near your home, please express your interest here.
Dwan Vilcins, Group leader, Environmental Epidemiology, Children’s Health Environment Program, The University of Queensland; Nicholas Osborne, Associate Professor, School of Public Health, The University of Queensland, and Paul D. Robinson, Conjoint Professor in Respiratory and Sleep Medicine, Child Health Research Centre, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: