Sleep wrinkles are real. Here’s how they leave their mark
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You wake up, stagger to the bathroom and gaze into the mirror. No, you’re not imagining it. You’ve developed face wrinkles overnight. They’re sleep wrinkles.
Sleep wrinkles are temporary. But as your skin loses its elasticity as you age, they can set in.
Here’s what you can do to minimise the chance of them forming in the first place.
How side-sleeping affects your face
Your skin wrinkles for a number of reasons, including ageing, sun damage, smoking, poor hydration, habitual facial expressions (such as grinning, pouting, frowning, squinting) and sleeping positions.
When you sleep on your side or stomach, your face skin is squeezed and crushed a lot more than if you sleep on your back. When you sleep on your side or stomach, gravity presses your face against the pillow. Your face skin is distorted as your skin is stretched, compressed and pulled in all directions as you move about in your sleep.
You can reduce these external forces acting on the face by sleeping on your back or changing positions frequently.
Doctors can tell which side you sleep on by looking at your face
In a young face, sleep wrinkles are transient and disappear after waking.
Temporary sleep wrinkles can become persistent with time and repetition. As we age, our skin loses elasticity (recoil) and extensibility (stretch), creating ideal conditions for sleep wrinkles or lines to set in and last longer.
The time spent in each sleeping position, the magnitude of external forces applied to each area of the face, as well as the surface area of contact with the pillow surface, also affects the pattern and rate of sleep wrinkle formation.
Skin specialists can often recognise this. People who favour sleeping on one side of their body tend to have a flatter face on their sleeping side and more visible sleep lines.
Can a night skincare routine avoid sleep wrinkles?
Collagen and elastin are two primary components of the dermis (inner layer) of skin. They form the skin structure and maintain the elasticity of skin.
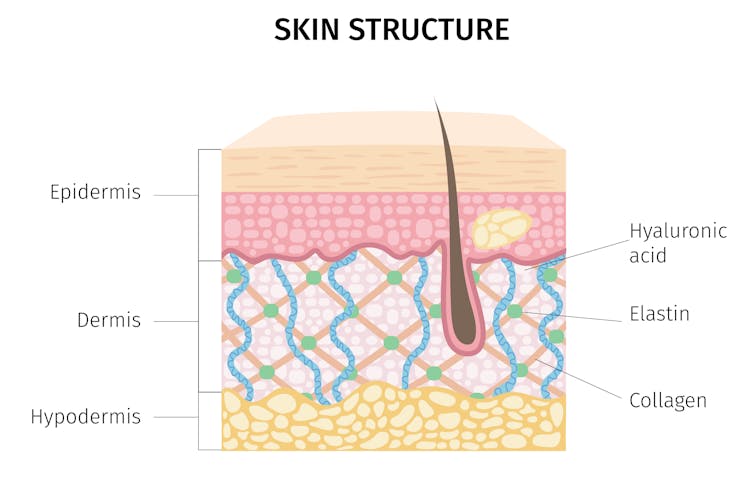
Supplementing collagen through skincare routines to enhance skin elasticity can help reduce wrinkle formation.
Hyaluronic acid is a naturally occurring molecule in human bodies. It holds our skin’s collagen and elastin in a proper configuration, stimulates the production of collagen and adds hydration, which can help slow down wrinkle formation. Hyaluronic acid is one of the most common active ingredients in skincare creams, gels and lotions.
Moisturisers can hydrate the skin in different ways. “Occlusive” substances produce a thin layer of oil on the skin that prevents water loss due to evaporation. “Humectants” attract and hold water in the skin, and they can differ in their capacity to bind with water, which influences the degree of skin hydration.
Do silk pillowcases actually make a difference?

Silk pillowcases can make a difference in wrinkle formation, if they let your skin glide and move, rather than adding friction and pressure on a single spot. If you can, use silk sheets and silk pillows.
Studies have also shown pillows designed to reduce mechanical stress during sleep can prevent skin deformations. Such a pillow could be useful in slowing down and preventing the formation of certain facial wrinkles.
Sleeping on your back can reduce the risk of sleep lines, as can a nighttime routine of moisturising before sleep.
Otherwise, lifestyle choices and habits, such quitting smoking, drinking plenty of water, a healthy diet (eating enough vegetables, fruits, nuts, seeds, healthy fats, yogurt and other fermented foods) and regular use of sunscreens can help improve the appearance of the skin on our face.
Yousuf Mohammed, Dermatology researcher, The University of Queensland; Khanh Phan, Postdoctoral Research Fellow, Frazer Institute, The University of Queensland, and Vania Rodrigues Leite E. Silva, Honorary Associate Professor, Frazer Institute, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Habits For Your Heart – by Monique Tello
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Did you guess we’d review this one today? Well, you’ve already had a taste of what Dr. Tello has to offer, but if you want to take your heart health seriously, this incredibly accessible guide is excellent.
Because Dr. Tello doesn’t assume prior knowledge, the first part of the book (the first three chapters) are given over to “heart and habit basics”—heart science, the effect your lifestyle can have on such, and how to change your habits.
The second part of the book is rather larger, and addresses changing foundational habits, nutrition habits, weight loss/maintenance, healthy activity habits, and specifically addressing heart-harmful habits (especially drinking, smoking, and the like).
She then follows up with a section of recipes, references, and other useful informational appendices.
The writing style throughout is super simple and clear, even when giving detailed clinical information. This isn’t a dusty old doctor who loves the sound of their own jargon, this is good heart health rendered as easy and accessible as possible to all.
Share This Post
-
The Galveston Diet – by Dr. Mary Claire Haver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed “It’s Not You, It’s Your Hormones” by nutritionist Nikki Williams, and noted at the time that it was very similar to the bestselling “The Galveston Diet”, not just in its content but all the way down its formatting. Some Amazon reviewers have even gone so far as to suggest that “It’s Not You, It’s Your Hormones” (2017) brazenly plagiarized “The Galveston Diet” (2023). However, after carefully examining the publication dates, we feel quite confident that the the earlier book did not plagiarize the later one.
Of course, we would not go so far as to make a counter-accusation of plagiarism the other way around; it was surely just a case of Dr. Haver having the same good ideas 6 years later.
Still, while the original book by Nikki Williams did not get too much international acclaim, the later one by Dr. Mary Claire Haver has had very good marketing and thus received a lot more attention, so let’s review it:
Dr. Haver’s basic principle is (again) that we can manage our hormonal fluctuations, by managing our diet. Specifically, in the same three main ways:
- Intermittent fasting
- Anti-inflammatory diet
- Eating more protein and healthy fats
Why should these things matter to our hormones? The answer is to remember that our hormones aren’t just the sex hormones. We have hormones for hunger and satedness, hormones for stress and relaxation, hormones for blood sugar regulation, hormones for sleep and wakefulness, and more. These many hormones make up our endocrine system, and affecting one part of it will affect the others.
Will these things magically undo the effects of the menopause? Well, some things yes, other things no. No diet can do the job of HRT. But by tweaking endocrine system inputs, we can tweak endocrine system outputs, and that’s what this book is for.
The style is once again very accessible and just as clear, and Dr. Haver also walks us just as skilfully through the changes we may want to make, to avoid the changes we don’t want. The recipes are also very similar, so if you loved the recipes in the other book, you certainly won’t dislike this book’s menu.
In the category of criticism, there is (as with the other book by the other author) some extra support that’s paywalled, in the sense that she wants the reader to buy her personally-branded online plan, and it can feel a bit like she’s holding back in order to upsell to that.
Bottom line: this book is (again) aimed at peri-menopausal and post-menopausal women. It could also (again) definitely help a lot of people with PCOS too, and, when it comes down to it, pretty much anyone with an endocrine system. It’s (still) a well-evidenced, well-established, healthy way of eating regardless of age, sex, or (most) physical conditions.
Click here to check out The Galveston Diet, and enjoy its well-told, well-formatted advice!
Share This Post
-
How Healers Heal – by Dr. Shilpi Pradhan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First note: the listed author here is in fact the compiler, with the authors being a collection of no fewer than 33 board-certified lifestyle medicine physicians. So, we’re not getting just a single person’s opinions/bias here!
But what is lifestyle medicine? This book holds the six pillars of lifestyle medicine to be:
- Nutrition
- Physical activity
- Stress management
- Restorative sleep
- Social connections
- Avoidance of risky substances
…and those things are what we read about throughout the book, both in highly educational mini-lecture form, and sometimes highly personal storytelling.
It’s not just a “do these things” book, though yes, there’s a large part of that. It also covers wide topics, from COVID to alopecia, burnout to grief, immune disorders to mysterious chest pains (and how such mysteries are unravelled, when taken seriously).
One of the greatest strengths of this book is that it’s very much “medicine, as it should be”, so that the reader knows how to recognize the difference.
Bottom line: this book doesn’t fit into a very neat category, but it’s a very worthwhile book to read, and one that could help inform a decision that changes the entire path of your life or that of a loved one.
Click here to check out How Healers Heal, and learn to recognize the healthcare you deserve!
Share This Post
Related Posts
-
Turkish Saffron Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Summer is upon us, and we need salad options. Coleslaw’s all well and good, until you’re the 4th person to bring it to the pot luck. Tzatziki’s great—and healthier than a standard coleslaw, being based in yogurt rather than mayonnaise as most Western coleslaws are (Eastern European coleslaws, for example, more often use a vinaigrette), but today our tastebuds are traveling to Turkey for this gut-healthy, phytochemical-rich, delicious dish.
You will need
- 12 oz carrots, cut into very thin batons (alternatively: use a peeler to peel it into super-thin strips)
- 2 oz chopped nuts (pistachios are traditional, almonds are also used sometimes; many other nuts would work too e.g. walnuts, hazelnuts, etc; not peanuts though)
- 2 cups kefir yogurt (if unavailable, substitute any 2 cups plain unsweetened yogurt; comparable plant yogurt is fine if you’re vegan; those healthy bacteria love plant yogurts as much as animal ones)
- 1 bulb garlic, grated
- 1 tsp chili flakes
- 1 pinch saffron, ground, then soaked in 1 tbsp warm water for a few hours
- 2 tbsp olive oil for cooking; ideally Extra Virgin, but at least Virgin
Method
(we suggest you read everything at least once before doing anything)
1) Put the olive oil and carrots into a saucepan and heat gently, stirring. You want to soften the carrots just a little and absorb the olive oil, without actually fully cooking the carrots; this will probably only take 2–3 minutes at most. Take it off the heat and transfer it to a bowl to cool.
When the mixture has cooled…
2) Add the kefir yogurt, garlic, chili flakes, and saffron water into the carrots, mixing thoroughly.
3) Add the chopped nuts as a garnish
(after mixing thoroughly, you will probably see more of the yogurt mixture and less of the carrots; that’s fine and correct))
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- The Many Health Benefits Of Garlic
- Capsaicin For Weight Loss And Against Inflammation
- Why You Should Diversify Your Nuts!
- Saffron For The Brain (& More) ← do not underestimate saffron’s neuroprotective qualities, and many other beneficial properties!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Younger Next Year – by Chris Crowley & Dr. Henry Lodge
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is it diet and exercise? Well, of course that’s a component. Specific kinds of exercise, too. But, as usual when we feature a book, there’s more:
In this case, strong throughout is the notion of life being a marathon not a sprint—and training for it accordingly.
Doing the things now that you’ll really wish you’d started doing sooner, and finding ways to build them into daily life.
Not just that, though! The authors take a holistic approach to life and health, and thus also cover work life, social life, and so forth. Now, you may be thinking “I’m already in the 80 and beyond category; I don’t work” and well, the authors advise that you do indeed work. You don’t have to revamp your career, but science strongly suggests that people who work longer, live longer.
Of course that doesn’t have to mean going full-throttle like a 20-year-old determined to make their mark on the world (you can if you want, though). It could be volunteering for a charity, or otherwise just finding a socially-engaging “work-like” activity that gives you purpose.
About the blend of motivational pep talk and science—this book is heavily weighted towards the former. It has, however, enough science to keep it on the right track throughout. Hence the two authors! Crowley for motivational pep, and Dr. Lodge for the science (with extra input from brain surgeon Dr. Hamilton, too).
Bottom line: if you want to feel the most prepared possible for the coming years and decades, this is a great book that covers a lot of bases.
Click here to check out “Younger Next Year” and get de-aging!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Endure – by Alex Hutchinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Life is a marathon, not a sprint. For most of us, at least. But how do we pace ourselves to go the distance, without falling into complacency along the way?
According to our author Alex Hutchinson, there’s a lot more to it than goal-setting and strategy.
Hutchinson set out to write a running manual, and ended up writing a manual for life. To be clear, this is still mostly centered around the science of athletic endurance, but covers the psychological factors as much as the physical… and notes how the capacity to endure is the key trait that underlies great performance in every field.
The writing style is both personal and personable, and parts read like a memoir (Hutchinson himself being a runner and sports journalist), while others are scientific in nature.
As for the science, the kind of science examined runs the gamut from case studies to clinical studies. We examine not just the science of physical endurance, but the science of psychological endurance too. We learn about such things as:
- How perception of ease/difficulty plays its part
- What factors make a difference to pain tolerance
- How mental exhaustion affects physical performance
- What environmental factors increase or lessen our endurance
- …and many other elements that most people don’t consider
Bottom line: whether you want to run a marathon in under two hours, or just not quit after one minute forty seconds on the exercise bike, or to get through a full day’s activities while managing chronic pain, this book can help.
Click here to check out Endure, and find out what you are capable of when you move your limits!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: