Six Ways To Eat For Healthier Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sadia Badiei, the nutritionist-chef of “Pick Up Limes” fame, has advice:
More than skin-deep:
We’ll not keep them a mystery; here are the six points of focus:
1. Collagen and skin elasticity
Collagen is the structural protein that provides firmness and elasticity to the skin, but its production decreases with age, resulting in about a 1% annual loss starting at age 20. To support collagen, a diet rich in protein is essential, including foods like beans, lentils, tofu, tempeh, nuts, and seeds. They can’t do their work alone though; vitamins C and E play a critical role in collagen production and repair, protecting against damage from sun exposure, pollution, and free radicals. Vitamin E can be found in almonds, sunflower seeds, leafy greens, peanuts, and avocados, while vitamin C is abundant in citrus fruits, bell peppers, and broccoli.
2. Skin healing and zinc
Zinc is critical for wound healing and reducing inflammation, making it particularly helpful in managing skin conditions such as acne, eczema, psoriasis, and rosacea. Great dietary sources of zinc include nutritional yeast, pumpkin, sesame, and hemp seeds, as well as legumes and whole grains. However, zinc absorption can be hindered by phytate levels in some foods. Soaking, sprouting, or fermenting foods where possible can correct for that and improve zinc absorption.
3. Dry skin and hydration
Dry skin can result from many things, including dry air, hot water, abrasive soaps, and certain medications. While moisturizers provide external hydration, dietary omega-3 fats are essential for improving the skin’s barrier function, helping it retain moisture. Plant-based sources of omega-3s include walnuts, hemp seeds, chia seeds, flax seeds, and algae-based supplements. Staying adequately hydrated also supports overall health of course (everything runs on water in one way or another, after all), which indirectly benefits skin hydration, although drinking additional water only helps if dehydration is present.
4. Sebum regulation
Sebum, an oily substance that lubricates the skin, can cause issues like acne and blackheads when overproduced. Hormonal fluctuations and diet both influence sebum levels (in either direction). High glycemic index foods, such as sweetened beverages, refined grains, and sugary snacks, can lead to spikes in insulin, which in turn stimulates excess sebum production. In contrast, low glycemic index foods like vegetables, whole grains, tofu, nuts, and seeds regulate blood sugar and help manage sebum production, promoting clearer skin without an excess or a shortage of sebum.
5. Gut health and skin
The gut-skin connection means that imbalances in gut bacteria can contribute to skin issues like acne, eczema, and psoriasis. Supporting gut health involves increasing the diversity of beneficial bacteria through probiotic-rich foods. Fermented options like plant-based yogurts, kimchi, miso, sauerkraut, and kombucha not only improve gut microbiome health but also positively impact skin health by reducing inflammation and improving overall skin conditions.
6. Inflammation and skin health
Chronic inflammation is associated with so many health issues, and when it comes to skin, that includes acne, rosacea, and even wrinkles. Anti-inflammatory foods, especially those rich in antioxidants, can mitigate these effects and improve skin elasticity, smoothness, and color. Diets centered around fruits, vegetables, and other plant-based foods provide the necessary nutrients to combat inflammation, showcasing the significant role of nutrition in promoting radiant, healthy skin.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Undo The Sun’s Damage To Your Skin
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Homeopathy: Evidence So Tiny That It’s Not there?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Homeopathy: Evidence So Tiny That It’s Not There?
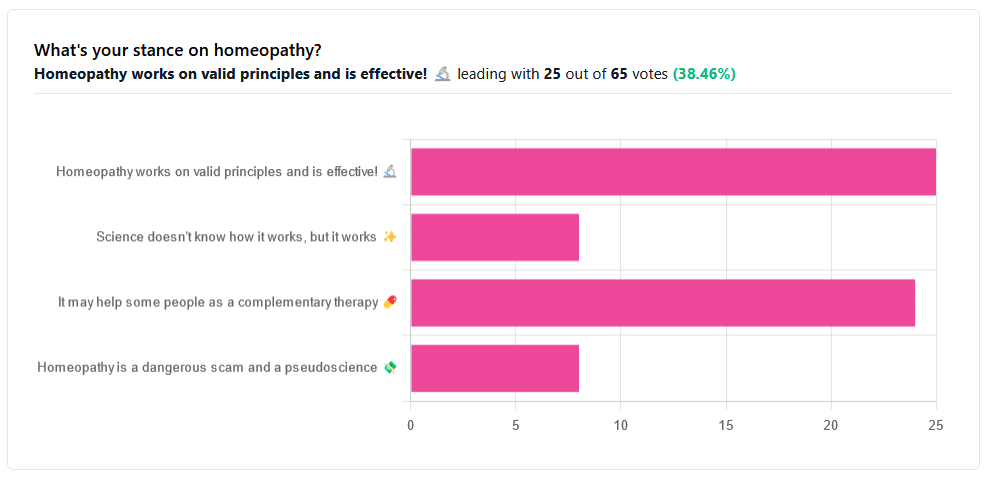
Yesterday, we asked you your opinions on homeopathy. The sample size of responses was a little lower than we usually get, but of those who did reply, there was a clear trend:
- A lot of enthusiasm for “Homeopathy works on valid principles and is effective”
- Near equal support for “It may help some people as a complementary therapy”
- Very few people voted for “Science doesn’t know how it works, but it works”; this is probably because people who considered voting for this, voted for the more flexible “It may help some people as a complementary therapy” instead.
- Very few people considered it a dangerous scam and a pseudoscience.
So, what does the science say?
Well, let us start our investigation by checking out the position of the UK’s National Health Service, an organization with a strong focus on providing the least expensive treatments that are effective.
Since homeopathy is very inexpensive to arrange, they will surely want to put it atop their list of treatments, right?
❝Homeopathy is a “treatment” based on the use of highly diluted substances, which practitioners claim can cause the body to heal itself.
There’s been extensive investigation of the effectiveness of homeopathy. There’s no good-quality evidence that homeopathy is effective as a treatment for any health condition.❞
The NHS actually has a lot more to say about that, and you can read their full statement here.
But that’s just one institution. Here’s what Australia’s National Health and Medical Research Council had to say:
❝There was no reliable evidence from research in humans that homeopathy was effective for treating the range of health conditions considered: no good-quality, well-designed studies with enough participants for a meaningful result reported either that homeopathy caused greater health improvements than placebo, or caused health improvements equal to those of another treatment❞
You can read their full statement here.
The American FDA, meanwhile, have a stronger statement:
❝Homeopathic drug products are made from a wide range of substances, including ingredients derived from plants, healthy or diseased animal or human sources, minerals and chemicals, including known poisons. These products have the potential to cause significant and even permanent harm if they are poorly manufactured, since that could lead to contaminated products or products that have potentially toxic ingredients at higher levels than are labeled and/or safe, or if they are marketed as substitute treatments for serious or life-threatening diseases and conditions, or to vulnerable populations.❞
You can read their full statement here.
Homeopathy is a dangerous scam and a pseudoscience: True or False?
False and True, respectively, mostly.
That may be a confusing answer, so let’s elaborate:
- Is it dangerous? Mostly not; it’s mostly just water. However, two possibilities for harm exist:
- Careless preparation could result in a harmful ingredient still being present in the water—and because of the “like cures like” principle, many of the ingredients used in homeopathy are harmful, ranging from heavy metals to plant-based neurotoxins. However, the process of “ultra-dilution” usually removes these so thoroughly that they are absent or otherwise scientifically undetectable.
- Placebo treatment has its place, but could result in “real” treatment going undelivered. This can cause harm if the “real” treatment was critically needed, especially if it was needed on a short timescale.
- Is it a scam? Probably mostly not; to be a scam requires malintent. Most practitioners probably believe in what they are practising.
- Is it a pseudoscience? With the exception that placebo effect has been highly studied and is a very valid complementary therapy… Yes, aside from that it is a pseudoscience. There is no scientific evidence to support homeopathy’s “like cures like” principle, and there is no scientific evidence to support homeopathy’s “water memory” idea. On the contrary, they go against the commonly understood physics of our world.
It may help some people as a complementary therapy: True or False?
True! Not only is placebo effect very well-studied, but best of all, it can still work as a placebo even if you know that you’re taking a placebo… Provided you also believe that!
Science doesn’t know how it works, but it works: True or False?
False, simply. At best, it performs as a placebo.
Placebo is most effective when it’s a remedy against subjective symptoms, like pain.
However, psychosomatic effect (the effect that our brain has on the rest of our body, to which it is very well-connected) can mean that placebo can also help against objective symptoms, like inflammation.
After all, our body, directed primarily by the brain, can “decide” what immunological defenses to deploy or hold back, for example. This is why placebo can help with conditions as diverse as arthritis (an inflammatory condition) or diabetes (an autoimmune condition, and/or a metabolic condition, depending on type).
Here’s how homeopathy measures up, for those conditions:
(the short answer is “no better than placebo”)
Homeopathy works on valid principles and is effective: True or False?
False, except insofar as placebo is a valid principle and can be effective.
The stated principles of homeopathy—”like cures like” and “water memory”—have no scientific basis.
We’d love to show the science for this, but we cannot prove a negative.
However, the ideas were conceived in 1796, and are tantamount to alchemy. A good scientific attitude means being open-minded to new ideas and testing them. In homeopathy’s case, this has been done, extensively, and more than 200 years of testing later, homeopathy has consistently performed equal to placebo.
In summary…
- If you’re enjoying homeopathic treatment and that’s working for you, great, keep at it.
- If you’re open-minded to enjoying a placebo treatment that may benefit you, be careful, but don’t let us stop you.
- If your condition is serious, please do not delay seeking evidence-based medical treatment.
Share This Post
-
From banning junk food ads to a sugar tax: with diabetes on the rise, we can’t afford to ignore the evidence any longer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are renewed calls this week for the Australian government to implement a range of measures aimed at improving our diets. These include restrictions on junk food advertising, improvements to food labelling, and a levy on sugary drinks.
This time the recommendations come from a parliamentary inquiry into diabetes in Australia. Its final report, tabled in parliament on Wednesday, was prepared by a parliamentary committee comprising members from across the political spectrum.
The release of this report could be an indication that Australia is finally going to implement the evidence-based healthy eating policies public health experts have been recommending for years.
But we know Australian governments have historically been unwilling to introduce policies the powerful food industry opposes. The question is whether the current government will put the health of Australians above the profits of companies selling unhealthy food.
benjamas11/Shutterstock Diabetes in Australia
Diabetes is one of the fastest growing chronic health conditions in the nation, with more than 1.3 million people affected. Projections show the number of Australians diagnosed with the condition is set to rise rapidly in coming decades.
Type 2 diabetes accounts for the vast majority of cases of diabetes. It’s largely preventable, with obesity among the strongest risk factors.
This latest report makes it clear we need an urgent focus on obesity prevention to reduce the burden of diabetes. Type 2 diabetes and obesity cost the Australian economy billions of dollars each year and preventive solutions are highly cost-effective.
This means the money spent on preventing obesity and diabetes would save the government huge amounts in health care costs. Prevention is also essential to avoid our health systems being overwhelmed in the future.
What does the report recommend?
The report puts forward 23 recommendations for addressing diabetes and obesity. These include:
- restrictions on the marketing of unhealthy foods to children, including on TV and online
- improvements to food labelling that would make it easier for people to understand products’ added sugar content
- a levy on sugary drinks, where products with higher sugar content would be taxed at a higher rate (commonly called a sugar tax).
These key recommendations echo those prioritised in a range of reports on obesity prevention over the past decade. There’s compelling evidence they’re likely to work.
Restrictions on unhealthy food marketing
There was universal support from the committee for the government to consider regulating marketing of unhealthy food to children.
Public health groups have consistently called for comprehensive mandatory legislation to protect children from exposure to marketing of unhealthy foods and related brands.
An increasing number of countries, including Chile and the United Kingdom, have legislated unhealthy food marketing restrictions across a range of settings including on TV, online and in supermarkets. There’s evidence comprehensive policies like these are having positive results.
In Australia, the food industry has made voluntary commitments to reduce some unhealthy food ads directly targeting children. But these promises are widely viewed as ineffective.
The government is currently conducting a feasibility study on additional options to limit unhealthy food marketing to children.
But the effectiveness of any new policies will depend on how comprehensive they are. Food companies are likely to rapidly shift their marketing techniques to maximise their impact. If any new government restrictions do not include all marketing channels (such as TV, online and on packaging) and techniques (including both product and brand marketing), they’re likely to fail to adequately protect children.
Food labelling
Food regulatory authorities are currently considering a range of improvements to food labelling in Australia.
For example, food ministers in Australia and New Zealand are soon set to consider mandating the health star rating front-of-pack labelling scheme.
Public health groups have consistently recommended mandatory implementation of health star ratings as a priority for improving Australian diets. Such changes are likely to result in meaningful improvements to the healthiness of what we eat.
Regulators are also reviewing potential changes to how added sugar is labelled on product packages. The recommendation from the committee to include added sugar labelling on the front of product packaging is likely to support this ongoing work.
But changes to food labelling laws are notoriously slow in Australia. And food companies are known to oppose and delay any policy changes that might hurt their profits.
Health star ratings are not compulsory in Australia. BLACKDAY/Shutterstock A sugary drinks tax
Of the report’s 23 recommendations, the sugary drinks levy was the only one that wasn’t universally supported by the committee. The four Liberal and National party members of the committee opposed implementation of this policy.
As part of their rationale, the dissenting members cited submissions from food industry groups that argued against the measure. This follows a long history of the Liberal party siding with the sugary drinks industry to oppose a levy on their products.
The dissenting members didn’t acknowledge the strong evidence that a sugary drinks levy has worked as intended in a wide range of countries.
In the UK, for example, a levy on sugary drinks implemented in 2018 has successfully lowered the sugar content in UK soft drinks and reduced sugar consumption.
The dissenting committee members argued a sugary drinks levy would hurt families on lower incomes. But previous Australian modelling has shown the two most disadvantaged quintiles would reap the greatest health benefits from such a levy, and accrue the highest savings in health-care costs.
What happens now?
Improvements to population diets and prevention of obesity will require a comprehensive and coordinated package of policy reforms.
Globally, a range of countries facing rising epidemics of obesity and diabetes are starting to take such strong preventive action.
In Australia, after years of inaction, this week’s report is the latest sign that long-awaited policy change may be near.
But meaningful and effective policy change will require politicians to listen to the public health evidence rather than the protestations of food companies concerned about their bottom line.
Gary Sacks, Professor of Public Health Policy, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How extreme heat can affect you—and how you can protect yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Because of climate change, last summer was the hottest in the Northern Hemisphere in 2,000 years—and this summer is expected to be even hotter. The record may continue to be broken: Extreme heat is expected to become even more frequent.
The scorching heat has led to an increase in heat-related deaths in the United States, according to the Department of Health and Human Services, with approximately 2,300 deaths in the summer of 2023. Extreme heat, defined as a period of two to three days with high heat and humidity with temperatures above 90 degrees Fahrenheit, can have serious health consequences, including symptoms like headache, dizziness, loss of consciousness, nausea, and confusion.
As we face more extreme heat, you may be wondering how you can protect yourself and your loved ones. Read on to learn about heat-related illness, who’s most at risk, and more.
What happens when our bodies are exposed to extreme heat?
As our body temperature rises, our bodies attempt to cool down by opening up more blood vessels near the skin to begin sweating. The evaporation of our sweat regulates our body temperature, but it also leads to losing fluids and minerals.
When it’s too humid, sweating alone doesn’t do the trick. The heart must work harder to bring blood around the body. It starts beating faster, which can cause light-headedness, nausea, and headache.
This process can affect our health in different ways, including increasing our risk of hospitalization for heart disease, worsening asthma, and injuring kidneys due to dehydration. It can also result in heat-related illness. Below are some effects of heat on our bodies:
- Heat cramps: Occur when a person loses salt through sweating, which causes painful cramps. Symptoms begin as painful spasms after heavy sweating, usually in the legs or the stomach. Heat cramps can lead to heat exhaustion or heat stroke.
- Heat exhaustion: This occurs when the body loses an excessive amount of water and salt, usually during intense physical activity. Symptoms include irritability, heavy sweating, and weakness, including muscle cramps. Heat exhaustion can lead to heat stroke.
- Heat stroke: This is the most severe heat-related illness. It happens when the body can’t cool down and reaches a temperature of 106 Fahrenheit or higher within 10 to 15 minutes. If the person doesn’t receive emergency treatment, it can cause permanent disability or death. Symptoms include confusion, loss of consciousness, and seizures.
What should I do if someone experiences a heat-related illness?
If you or someone you’re with begins to show signs of heat illness, the Centers for Disease Control and Prevention recommends the following:
- Heat cramps: Stop all physical activity, drink water or a sports drink, move to a cool place, and wait for cramps to go away before resuming activity. If the cramps last more than an hour, you’re on a low-sodium diet, or you have heart problems, get medical help.
- Heat exhaustion: Move the person to a cool place, loosen their clothes, use a cool bath or cloths to try to lower their body temperature, and give them a sip of water. If the person throws up, or if their symptoms last longer than an hour or worsen, get medical help.
- Heat stroke: Call 911 immediately. Then, move the person to a cooler place, use cool cloths or a cool bath to help lower their temperature, and don’t give them anything to drink.
Read more about heat-related illness and what to do in each case.
Who’s more vulnerable to extreme heat?
While everyone can be affected by extreme heat, some people are more at risk, including people of color.
A 2023 KFF report outlined that because of historical residential segregation in the U.S. (known as “redlining”), people of color are more likely to live in areas that experience higher temperatures from rooftops, asphalt, and sidewalks that retain the sun’s heat (known as the “urban heat island effect”). Additionally, communities of color are more likely to live in areas with fewer trees, which act as a canopy and provide shade, making the heat worse and more direct.
Children under 5, adults 65 or over, and pregnant people are also more vulnerable to extreme heat. If you have a chronic health condition like diabetes, heart problems, or a mental health condition, you’re also at higher risk. (Some psychiatric medications, like antidepressants, can also make people more susceptible to heat).
Lastly, anyone exposed to the sun and extreme heat for long periods is also at higher risk. This includes athletes, people who work outdoors, and unhoused people.
What can I do to prevent heat-related illness during a heat wave?
During a heat wave, follow these tips to stay cool and protect yourself from heat-related illness:
- Never leave your pets or children inside a car.
- Wear loose, light-colored clothing (dark colors absorb more heat).
- Find shade if you’re outside.
- If you don’t have air conditioning in your home, go to a place where you can cool down, such as a local library, community center, local pool or splash pad, or mall. Check to see if your city has designated cooling centers. (Cities like New York have a list of places.)
- Wear a hat.
- Drink (non-alcoholic) fluids often to stay hydrated—and if you have pets, give them water frequently as well.
- Check on your family members or older neighbors who may be more sensitive to extreme heat.
- Avoid using your stove or oven too often or during the hottest parts of the day.
- Cover your windows with shades to keep the heat out.
What are some resources to prevent heat-related illness?
If you need financial assistance to cool down your home, such as to purchase an air conditioner, apply to the federal government’s Low Income Home Energy Assistance Program.
Before you head outside during a heat wave, use the CDC’s HeatRisk tool: Enter your zip code to find the current heat risk in your area and get tips on what to do to stay safe with each risk level.
During a heat wave, also look for a cooling center in your state using the National Center for Healthy Housing’s list.
Check out the National Weather Service’s for more tips and resources.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Mammography AI Can Cost Patients Extra. Is It Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As I checked in at a Manhattan radiology clinic for my annual mammogram in November, the front desk staffer reviewing my paperwork asked an unexpected question: Would I like to spend $40 for an artificial intelligence analysis of my mammogram? It’s not covered by insurance, she added.
I had no idea how to evaluate that offer. Feeling upsold, I said no. But it got me thinking: Is this something I should add to my regular screening routine? Is my regular mammogram not accurate enough? If this AI analysis is so great, why doesn’t insurance cover it?
I’m not the only person posing such questions. The mother of a colleague had a similar experience when she went for a mammogram recently at a suburban Baltimore clinic. She was given a pink pamphlet that said: “You Deserve More. More Accuracy. More Confidence. More power with artificial intelligence behind your mammogram.” The price tag was the same: $40. She also declined.
In recent years, AI software that helps radiologists detect problems or diagnose cancer using mammography has been moving into clinical use. The software can store and evaluate large datasets of images and identify patterns and abnormalities that human radiologists might miss. It typically highlights potential problem areas in an image and assesses any likely malignancies. This extra review has enormous potential to improve the detection of suspicious breast masses and lead to earlier diagnoses of breast cancer.
While studies showing better detection rates are extremely encouraging, some radiologists say, more research and evaluation are needed before drawing conclusions about the value of the routine use of these tools in regular clinical practice.
“I see the promise and I hope it will help us,” said Etta Pisano, a radiologist who is chief research officer at the American College of Radiology, a professional group for radiologists. However, “it really is ambiguous at this point whether it will benefit an individual woman,” she said. “We do need more information.”
The radiology clinics that my colleague’s mother and I visited are both part of RadNet, a company with a network of more than 350 imaging centers around the country. RadNet introduced its AI product for mammography in New York and New Jersey last February and has since rolled it out in several other states, according to Gregory Sorensen, the company’s chief science officer.
Sorensen pointed to research the company conducted with 18 radiologists, some of whom were specialists in breast mammography and some of whom were generalists who spent less than 75% of their time reading mammograms. The doctors were asked to find the cancers in 240 images, with and without AI. Every doctor’s performance improved using AI, Sorensen said.
Among all radiologists, “not every doctor is equally good,” Sorensen said. With RadNet’s AI tool, “it’s as if all patients get the benefit of our very top performer.”
But is the tech analysis worth the extra cost to patients? There’s no easy answer.
“Some people are always going to be more anxious about their mammograms, and using AI may give them more reassurance,” said Laura Heacock, a breast imaging specialist at NYU Langone Health’s Perlmutter Cancer Center in New York. The health system has developed AI models and is testing the technology with mammograms but doesn’t yet offer it to patients, she said.
Still, Heacock said, women shouldn’t worry that they need to get an additional AI analysis if it’s offered.
“At the end of the day, you still have an expert breast imager interpreting your mammogram, and that is the standard of care,” she said.
About 1 in 8 women will be diagnosed with breast cancer during their lifetime, and regular screening mammograms are recommended to help identify cancerous tumors early. But mammograms are hardly foolproof: They miss about 20% of breast cancers, according to the National Cancer Institute.
The FDA has authorized roughly two dozen AI products to help detect and diagnose cancer from mammograms. However, there are currently no billing codes radiologists can use to charge health plans for the use of AI to interpret mammograms. Typically, the federal Centers for Medicare & Medicaid Services would introduce new billing codes and private health plans would follow their lead for payment. But that hasn’t happened in this field yet and it’s unclear when or if it will.
CMS didn’t respond to requests for comment.
Thirty-five percent of women who visit a RadNet facility for mammograms pay for the additional AI review, Sorensen said.
Radiology practices don’t handle payment for AI mammography all in the same way.
The practices affiliated with Boston-based Massachusetts General Hospital don’t charge patients for the AI analysis, said Constance Lehman, a professor of radiology at Harvard Medical School who is co-director of the Breast Imaging Research Center at Mass General.
Asking patients to pay “isn’t a model that will support equity,” Lehman said, since only patients who can afford the extra charge will get the enhanced analysis. She said she believes many radiologists would never agree to post a sign listing a charge for AI analysis because it would be off-putting to low-income patients.
Sorensen said RadNet’s goal is to stop charging patients once health plans realize the value of the screening and start paying for it.
Some large trials are underway in the United States, though much of the published research on AI and mammography to date has been done in Europe. There, the standard practice is for two radiologists to read a mammogram, whereas in the States only one radiologist typically evaluates a screening test.
Interim results from the highly regarded MASAI randomized controlled trial of 80,000 women in Sweden found that cancer detection rates were 20% higher in women whose mammograms were read by a radiologist using AI compared with women whose mammograms were read by two radiologists without any AI intervention, which is the standard of care there.
“The MASAI trial was great, but will that generalize to the U.S.? We can’t say,” Lehman said.
In addition, there is a need for “more diverse training and testing sets for AI algorithm development and refinement” across different races and ethnicities, said Christoph Lee, director of the Northwest Screening and Cancer Outcomes Research Enterprise at the University of Washington School of Medicine.
The long shadow of an earlier and largely unsuccessful type of computer-assisted mammography hangs over the adoption of newer AI tools. In the late 1980s and early 1990s, “computer-assisted detection” software promised to improve breast cancer detection. Then the studies started coming in, and the results were often far from encouraging. Using CAD at best provided no benefit, and at worst reduced the accuracy of radiologists’ interpretations, resulting in higher rates of recalls and biopsies.
“CAD was not that sophisticated,” said Robert Smith, senior vice president of early cancer detection science at the American Cancer Society. Artificial intelligence tools today are a whole different ballgame, he said. “You can train the algorithm to pick up things, or it learns on its own.”
Smith said he found it “troubling” that radiologists would charge for the AI analysis.
“There are too many women who can’t afford any out-of-pocket cost” for a mammogram, Smith said. “If we’re not going to increase the number of radiologists we use for mammograms, then these new AI tools are going to be very useful, and I don’t think we can defend charging women extra for them.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
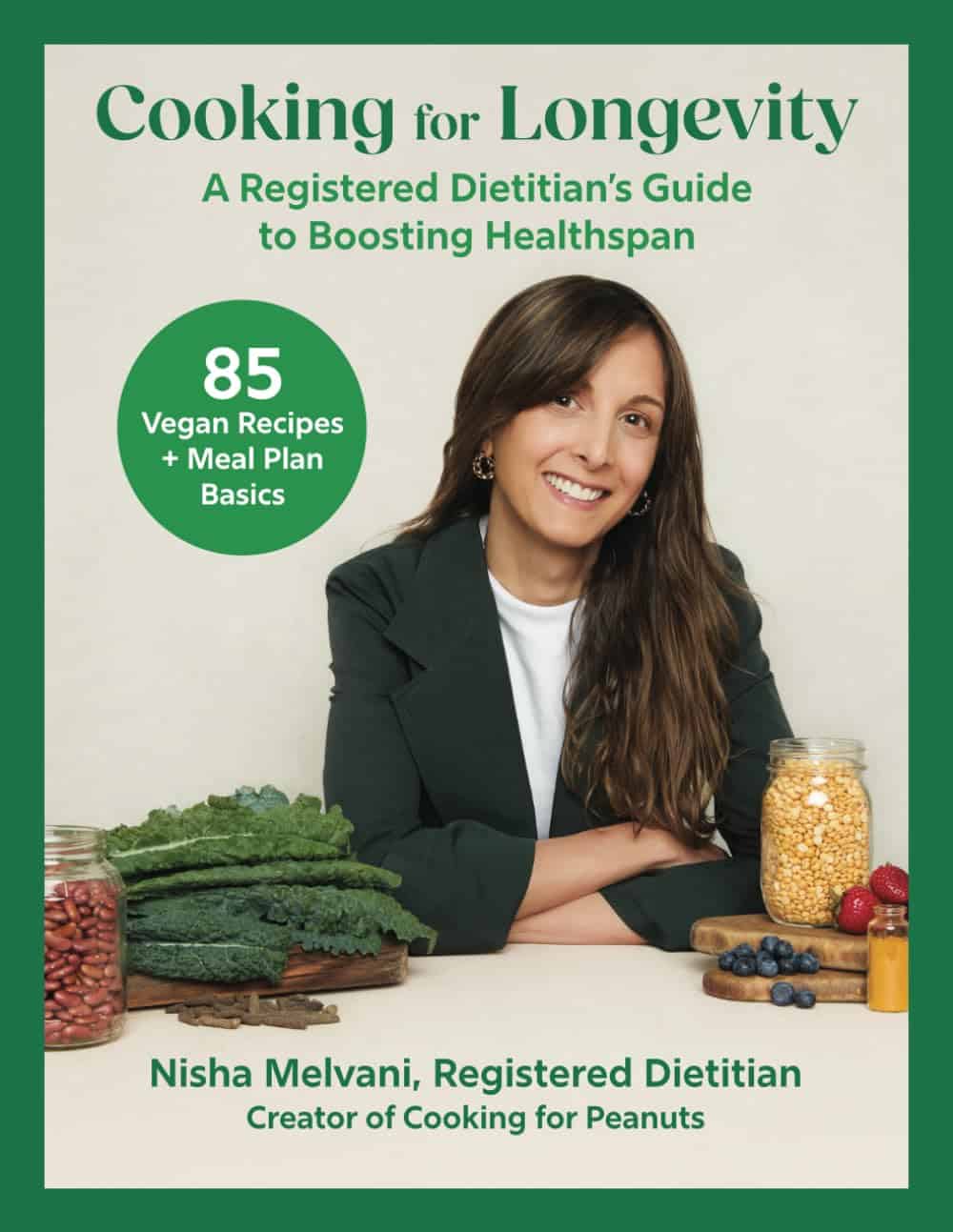
Cooking for Longevity – by Nisha Melvani
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Before it gets to the recipes, this book kicks off with a lot of science (much more than is usual for even healthy-eating recipe books), demystifying more nutrients than most people think of on a daily basis, what they do and where to get them, and even how to enhance nutrient absorption.
As well as an up-front ingredients list, we additionally get not just meal planning advice in the usual sense of the word, but also advice on timing various aspects of nutrition in order to enjoy the best metabolic benefits.
The recipes themselves are varied and good. It’s rare to find a recipe book that doesn’t include some redundant recipes, and this one’s no exception, but it’s better to have too much information than too little, so it’s perhaps no bad thing that all potentially necessary bases are covered.
In terms of how well it delivers on the title’s promised “cooking for longevity” and the subtitle’s promised “boosting healthspan”, the science is good; very consistent with what we write here at 10almonds, and well-referenced too.
Bottom line: if you’d like recipes to help you live longer and more healthily, then this book has exactly that.
Click here to check out Cooking For Longevity, and cook for longevity!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Avoid UTIs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Psst… A Word To The Wise
Urinary Tract Infections (UTIs) can strike at any age, but they get a lot more common as we get older:
- About 10% of women over 65 have had one
- About 30% of women over 85 have had one
Source: Urinary tract infection in older adults
Note: those figures are almost certainly very underreported, so the real figures are doubtlessly higher. However, we print them here as they’re still indicative of a disproportionate increase in risk over time.
What about men?
Men do get UTIs too, but at a much lower rate. The difference in average urethra length means that women are typically 30x more likely to get a UTI.
However! If a man does get one, then assuming the average longer urethra, it will likely take much more treatment to fix:
Case study: 26-Year-Old Man With Recurrent Urinary Tract Infections
Risk factors you might want to know about
While you may not be able to do much about your age or the length of your urethra, there are some risk factors that can be more useful to know:
Catheterization
You might logically think that having a catheter would be the equivalent of having a really long urethra, thus keeping you safe, but unfortunately, the opposite is true:
Read more: Review of Catheter-Associated Urinary Tract Infections
Untreated menopause
Low estrogen levels can cause vaginal tissue to dry, making it easier for pathogens to grow.
For more information on menopausal HRT, see:
What You Should Have Been Told About Menopause Beforehand
Sexual activity
Most kinds of sexual activity carry a risk of bringing germs very close to the urethra. Without wishing to be too indelicate: anything that’s going there should be clean, so it’s a case for washing your hands/partner(s)/toys etc.
For the latter, beyond soap and water, you might also consider investing in a UV sanitizer box ← This example has a 9” capacity; if you shop around though, be sure to check the size is sufficient!
Kidney stones and other kidney diseases
Anything that impedes the flow of urine can raise the risk of a UTI.
See also: Keeping Your Kidneys Healthy (Especially After 60)
Diabetes
How much you can control this one will obviously depend on which type of diabetes you have, but diabetes of any type is an immunocompromizing condition. If you can, managing it as well as possible will help many aspects of your health, including this one.
More on that:
How To Prevent And Reverse Type 2 Diabetes
Note: In the case of Type 1 Diabetes, the above advice will (alas) not help you to prevent or reverse it. However, reducing/avoiding insulin resistance is even more important in cases of T1D (because if your exogenous insulin stops working, you die), so the advice is good all the same.
How do I know if I have a UTI?
Routine screening isn’t really a thing, since the symptoms are usually quite self-evident. If it hurts/burns when you pee, the most likely reason is a UTI.
Get it checked out; the test is a (non-invasive) urinalysis test. In other words, you’ll give a urine sample and they’ll test that.
Anything else I can do to avoid it?
Yes! We wrote previously about the benefits of cranberry supplementation, which was found even to rival antibiotics:
❝…recommend cranberry ingestion to decrease the incidence of urinary tract infections, particularly in individuals with recurrent urinary tract infections. This would also reduce the [need for] administration of antibiotics❞
Read more: Health Benefits Of Cranberries
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: