Seven Steps to Managing Your Memory – by Dr. Andrew Budson & Dr. Maureen O’Connor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: a “how to improve your memory” book of the kind marketed to students and/or people who want to do memory-themed party tricks.
What this book actually is: exactly what the title and subtitle claim it to be: seven steps to managing your memory: what’s normal, what’s not, and what to do about it.
Drs. Budson & O’Connor cover:
- which memory errors can (and usually do) happen at any age
- how memory changes with normal aging, and
- what kinds of memory problems are not normal.
One thing that sets this book aside from a lot of its genre is that it also covers which kinds of memory loss are reversible—and, where appropriate, what can be undertaken to effect such a reversal.
The authors talk about what things have (and what things haven’t!) been shown to strengthen memory and reduce cognitive decline, and in the worst case scenario, what medications can help against Alzheimer’s disease and other dementias.
The style is halfway between pop-science and a science textbook. The structure of the book, with its headings, subheadings, bullet points, summaries, etc, helps the reader to process and remember the information.
Bottom line: if you’d like to get on top of managing your memory before you forget, then this book is for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

What Nobody Teaches You About Strengthening Your Knees
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strengthening unhappy knees can seem difficult, because many obvious exercises like squats may hurt, and can feel like they are doing harm (and if your knees are bad enough, maybe they are; it depends on many factors). Here’s a way to improve things:
The muscle nobody talks about
Well, not nobody. But, it’s a muscle that’s rarely talked about; namely, the tibialis anterior.
It plays a key role in decelerating knee motion—in other words, the movement that hurts if you have bad knees. It’s essential for absorbing shock during activities like walking, climbing stairs, and stepping off curbs
So, of course, strengthening this muscle supports knee health.
The exercise this video recommends for strengthening it involves leaning against a wall with feet about a foot away (closer feet make it easier, further makes it harder). Note, this is a lean, not a “Roman chair”.
The exercise involves squeezing the quadriceps, lifting toes toward the nose, and engaging the tibialis anterior muscle. If you’re wondering what to do with your hands, they can be held out with palms open to work on posture, or hanging by the sides. Do this for about 1½–2 minutes.
For more on all this, plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
When Bad Joints Stop You From Exercising (5 Things To Change)
Take care!
Share This Post

Recognize The Early Symptoms Of Parkinson’s Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Parkinson’s disease is a degenerative condition with wide-reaching implications for health. While there is currently no known cure, there are treatments, so knowing about it sooner rather than later is important.
Spot The Signs
There are two main kinds of symptoms, motor and non-motor.
Motor symptoms include:
- trembling that occurs when muscles are relaxed; often especially visible in the fingers
- handwriting changes—not just because of the above, but also often getting smaller
- blank expression, on account of fewer instruction signals getting through to the face
- frozen gait—especially difficulty starting walking, and a reduced arm swing
Non-motor symptoms include:
- loss of sense of smell—complete, or a persistent reduction of
- sleepwalking, or sleep-talking, or generally acting out dreams while asleep
- constipation—on an ongoing basis
- depression/anxiety, especially if there was no prior history of these conditions
For more detail on each of these, as well as what steps you might want to take, check out what Dr. Luis Zayas has to say:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Citicoline vs Parkinson’s (And More)
Take care!
Share This Post

The Sweet Truth About Diabetes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s A Lot Of Confusion About Diabetes!
For those readers who are not diabetic, nor have a loved one who is diabetic, nor any other pressing reason to know these things, first a quick 101 rundown of some things to understand the rest of today’s main feature:
- Blood sugar levels: how much sugar is in the blood, measured in mg/dL or mmol/L
- Hyperglycemia or “hyper” for short: too much sugar in the blood
- Hypoglycemia or “hypo” for short: too little sugar in the blood
- Insulin: a hormone that acts as a gatekeeper to allow sugar to pass, or not pass, into various parts of the body
- Type 1 diabetes (sometimes capitalized, and/or abbreviated to “T1D”) is an autoimmune disorder that prevents the pancreas from being able to supply the body with insulin. This means that taking insulin consistently is necessary for life.
- Type 2 diabetes is a matter of insulin resistance. The pancreas produces plenty of insulin, but the body has become desensitized to it, so it doesn’t work properly. Taking extra insulin may sometimes be necessary, but for many people, it can be controlled by means of a careful diet and other lifestyle factors.
With that in mind, on to some very popular myths…
Diabetes is caused by having too much sugar
While sugar is not exactly a health food, it’s not the villain of this story either.
- Type 1 diabetes has a genetic basis, triggered by epigenetic factors unrelated to sugar.
- Type 2 diabetes comes from a cluster of risk factors which, together, can cause a person to go through pre-diabetes and acquire type 2 diabetes.
- Those risk factors include:
- A genetic predisposition
- A large waist circumference
- (this is more relevant than BMI or body fat percentage)
- High blood pressure
- A sedentary lifestyle
- Age (the risk starts rising at 35, rises sharply at 45, and continues upwards with increasing age)
- Those risk factors include:
Read more: Risk Factors for Type 2 Diabetes
Diabetics can’t have sugar
While it’s true that diabetics must be careful about sugar (and carbs in general), it’s not to say that they can’t have them… just: be mindful and intentional about it.
- Type 1 diabetics will need to carb-count in order to take the appropriate insulin bolus. Otherwise, too little insulin will result in hyperglycemia, or too much insulin will result in hypoglycemia.
- Type 2 diabetics will often be able to manage their blood sugar levels with diet alone, and slow-release carbs will make this easier.
In either case, having quick release sugars will increase blood sugar levels (what a surprise), and sometimes (such as when experiencing a hypo), that’s what’s needed.
Also, when it comes to sugar, a word on fruit:
Not all fruits are equal, and some fruits can help maintain stable blood sugar levels! Read all about it:
Fruit Intake to Prevent and Control Hypertension and Diabetes
Artificial sweeteners are must-haves for diabetics
Whereas sugar is a known quantity to the careful diabetic, some artificial sweeteners can impact insulin sensitivity, causing blood sugars to behave in unexpected ways. See for example:
The Impact of Artificial Sweeteners on Body Weight Control and Glucose Homeostasis
If a diabetic person is hyper, they should exercise to bring their blood sugar levels down
Be careful with this!
- In the case of type 2 diabetes, it may (or may not) help, as the extra sugar may be used up.
- Type 1 diabetes, however, has a crucial difference. Because the pancreas isn’t making insulin, a hyper (above a certain level, anyway) means more insulin is needed. Exercising could do more harm than good, as unlike in type 2 diabetes, the body has no way to use that extra sugar, without the insulin to facilitate it. Exercising will just pump the syrupy hyperglycemic blood around the body, potentially causing damage as it goes (all without actually being able to use it).
There are other ways this can be managed that are outside of the scope of this newsletter, but “be careful” is rarely a bad approach.
Read more, from the American Diabetes Association:
Share This Post
Related Posts

Cold Medicines & Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold Medicines & Heart Health
In the wake of many decongestants disappearing from a lot of shelves after a common active ingredient being declared useless*, you may find yourself considering alternative decongestants at this time of year.
*In case you missed it:
It doesn’t seem to be dangerous, by the way, just also not effective:
FDA Panel Says Common OTC Decongestant, Phenylephrine, Is Useless
Good for your nose, bad for your heart?
With products based on phenylephrine out of the running, products based on pseudoephedrine, a competing drug, are enjoying a surge in popularity.
Good news: pseudoephedrine works!
Bad news: pseudoephedrine works because it is a vasoconstrictor, and that vasoconstriction reduces nasal swelling. That same vasoconstriction also raises overall blood pressure, potentially dangerously, depending on an assortment of other conditions you might have.
Further reading: Can decongestants spike your blood pressure? What to know about hypertension and cold medicine
Who’s at risk?
The warning label, unread by many, reads:
❝Do not use this product if you have heart disease, high blood pressure, thyroid disease, diabetes, or difficulty in urination due to enlargement of the prostate gland, unless directed by a doctor❞
Source: Harvard Health | Don’t let decongestants squeeze your heart
What are the other options?
The same source as above recommends antihistamines as an option to be considered, citing:
❝Antihistamines such as […] cetirizine (Zyrtec) and loratadine (Claritin) can help with a stuffy nose and are safe for the heart.❞
But we’d be remiss not to mention drug-free options too, for example:
- Saline rinse with a neti pot or similar
- Use of a humidifier in your house/room
- Steam inhalation, with or without eucalyptus etc
See also: Inhaled Eucalyptus’s Immunomodulatory and Antimicrobial Effects
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Eggs: Nutritional Powerhouse or Heart-Health Timebomb?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eggs: All Things In Moderation?

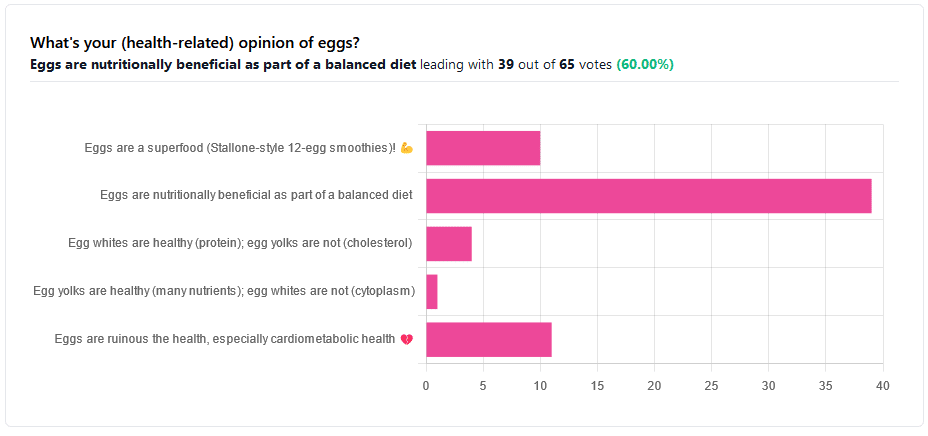
We asked you for your (health-related) opinion on eggs. We specified that, for the sake of simplicity, let’s say that they are from happy healthy backyard hens who enjoy a good diet.
Apparently this one wasn’t as controversial as it might have been! We (for myth-busting purposes) try to pick something polarizing and sometimes even contentious for our Friday editions, and pick apart what science lies underneath public perceptions.
However, more than half (in fact, 60%) of the subscribers who voted in the poll voted for “Eggs are nutritionally beneficial as part of a balanced diet”, which very moderate statement is indeed pretty much the global scientific consensus.
Still, we’ve a main feature to write, so let’s look at the science, and what the other 40% had in mind:
Eggs are ruinous to health, especially cardiometabolic health: True or False?
False, per best current science, anyway!
Scientific consensus has changed over the years. We learned about cholesterol, then we learned about different types of cholesterol, and now we’ve even learned about in some instances even elevated levels of “bad” cholesterol aren’t necessarily a cause of cardiometabolic disorders so much as a symptom—especially in women.
Not to derail this main feature about eggs (rather than just cholesterol), but for those who missed it, this is actually really interesting: basically, research (pertaining to the use of statins) has found that in women, higher LDL levels aren’t anywhere near the same kind of risk factor as they are for men, and thus may mean that statins (whose main job is reducing LDL) may be much less helpful for women than for men, and more likely to cause unwanted serious side effects in women.
Check out our previous main feature about this: Statins: His & Hers?
But, for back on topic, several large studies (totalling 177,000 people in long-term studies in 50 countries) found:
❝Results from the three cohorts and from the updated meta-analysis show that moderate egg consumption (up to one egg per day) is not associated with cardiovascular disease risk overall, and is associated with potentially lower cardiovascular disease risk in Asian populations.❞
Egg whites are healthy (protein); egg yolks are not (cholesterol): True or False?
True and False, respectively. That is to say, egg whites are healthy (protein), and egg yolks are also healthy (many nutrients).
We talked a bit already about cholesterol, so we’ll not rehash that here. As to the rest:
Eggs are one of the most nutritionally dense foods around. After all, they have everything required to allow a cluster of cells to become a whole baby chick. That’s a lot of body-building!
They’re even more nutritionally heavy-hitters if you get omega-3 enriched eggs, which means the hens were fed extra omega-3, usually in the form of flax seeds.
Also, free-range is better healthwise than others. Do bear in mind that unless they really are from your backyard, or a neighbor’s, chances are that the reality is not what the advertising depicts, though. There are industry minimum standards to be able to advertise as “free-range”, and those standards are a) quite low b) often ignored, because an occasional fine is cheaper than maintaining good conditions.
So if you can look after your own hens, or get them from somewhere that you can see for yourself how they are looked after, so much the better!
Check out the differences side-by-side, though:
Pastured vs Omega-3 vs “Conventional” Eggs: What’s the Difference?
Stallone-style 12-egg smoothies are healthy: True or False?
False, at least if taken with any regularity. One can indeed have too much of a good thing.
So, what’s the “right amount” to eat?
It may vary depending on individual factors (including age and ethnicity), but a good average, according to science, is to keep it to 3 eggs or fewer per day. There are a lot of studies, but we only have so much room here, so we’ll pick one. Its findings are representative of (and in keeping with) the many other studies we looked at, so this seems uncontroversial scientifically:
❝Intake of 1 egg/d was sufficient to increase HDL function and large-LDL particle concentration; however, intake of 2-3 eggs/d supported greater improvements in HDL function as well as increased plasma carotenoids. Overall, intake of ≤3 eggs/d favored a less atherogenic LDL particle profile, improved HDL function, and increased plasma antioxidants in young, healthy adults.❞
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Measles cases are rising—here’s how to protect your family
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The U.S. is currently experiencing a spike in measles cases across several states. Measles a highly contagious and potentially life-threatening disease caused by a virus. The measles-mumps-rubella (MMR) vaccine prevents measles; unvaccinated people put themselves and everyone around them at risk, including babies who are too young to receive the vaccine.
Read on to learn more about measles: what it is, how to stay protected, and what to do if a measles outbreak happens near you.
What are the symptoms of measles?
Measles symptoms typically begin 10 to 14 days after exposure. The disease starts with a fever followed by a cough, runny nose, and red eyes and then produces a rash of tiny red spots on the face and body. Measles can affect anyone, but is most serious for children under 5, immunocompromised people, and pregnant people, who may give birth prematurely or whose babies may have low birth weight as a result of a measles infection.
Measles isn’t just a rash—the disease can cause serious health problems and even death. About one in five unvaccinated people in the U.S. who get measles will be hospitalized and could suffer from pneumonia, dehydration, or brain swelling.
If you get measles, it can also damage your immune system, making you more vulnerable to other diseases.
How do you catch measles?
Measles spreads through the air when an infected person coughs or sneezes. It’s so contagious that unvaccinated people have a 90 percent chance of becoming infected if exposed.
An infected person can spread measles to others before they have symptoms.
Why are measles outbreaks happening now?
The pandemic caused many children to miss out on routine vaccinations, including the MMR vaccine. Delayed vaccination schedules coincided with declining confidence in vaccine safety and growing resistance to vaccine requirements.
Skepticism about the safety and effectiveness of COVID-19 vaccines has resulted in some people questioning or opposing the MMR vaccine and other routine immunizations.
How do I protect myself and my family from measles?
Getting an MMR vaccine is the best way to prevent getting sick with measles or spreading it to others. The CDC recommends that children receive the MMR vaccine at 12 to 15 months and again at 4 to 6 years, before starting kindergarten.
One dose of the MMR vaccine provides 93 percent protection and two doses provide 97 percent protection against all strains of measles. Because some children are too young to be immunized, it’s important that those around them are vaccinated to protect them.
Is the MMR vaccine safe?
The MMR vaccine has been rigorously tested and monitored over 50 years and determined to be safe. Adverse reactions to the vaccine are extremely rare.
Receiving the MMR vaccine is much safer than contracting measles.
What do I do if there’s a measles outbreak in my community?
Anyone who is not fully vaccinated for measles should be immunized with a measles vaccine as soon as possible. Measles vaccines given within 72 hours after exposure may prevent or reduce the severity of disease.
Children as young as 6 months old can receive the MMR vaccine if they are at risk during an outbreak. If your child isn’t fully vaccinated with two doses of the MMR vaccine—or three doses, if your child received the first dose before their first birthday—talk to your pediatrician.
Unvaccinated people who have been exposed to the virus should stay home from work, school, day care, and other activities for 21 days to avoid spreading the disease.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.

Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: