Running or yoga can help beat depression, research shows – even if exercise is the last thing you feel like
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At least one in ten people have depression at some point in their lives, with some estimates closer to one in four. It’s one of the worst things for someone’s wellbeing – worse than debt, divorce or diabetes.
One in seven Australians take antidepressants. Psychologists are in high demand. Still, only half of people with depression in high-income countries get treatment.
Our new research shows that exercise should be considered alongside therapy and antidepressants. It can be just as impactful in treating depression as therapy, but it matters what type of exercise you do and how you do it.
Walk, run, lift, or dance away depression
We found 218 randomised trials on exercise for depression, with 14,170 participants. We analysed them using a method called a network meta-analysis. This allowed us to see how different types of exercise compared, instead of lumping all types together.
We found walking, running, strength training, yoga and mixed aerobic exercise were about as effective as cognitive behaviour therapy – one of the gold-standard treatments for depression. The effects of dancing were also powerful. However, this came from analysing just five studies, mostly involving young women. Other exercise types had more evidence to back them.
Walking, running, strength training, yoga and mixed aerobic exercise seemed more effective than antidepressant medication alone, and were about as effective as exercise alongside antidepressants.
But of these exercises, people were most likely to stick with strength training and yoga.
Antidepressants certainly help some people. And of course, anyone getting treatment for depression should talk to their doctor before changing what they are doing.
Still, our evidence shows that if you have depression, you should get a psychologist and an exercise plan, whether or not you’re taking antidepressants.
Join a program and go hard (with support)
Before we analysed the data, we thought people with depression might need to “ease into it” with generic advice, such as “some physical activity is better than doing none.”
But we found it was far better to have a clear program that aimed to push you, at least a little. Programs with clear structure worked better, compared with those that gave people lots of freedom. Exercising by yourself might also make it hard to set the bar at the right level, given low self-esteem is a symptom of depression.
We also found it didn’t matter how much people exercised, in terms of sessions or minutes a week. It also didn’t really matter how long the exercise program lasted. What mattered was the intensity of the exercise: the higher the intensity, the better the results.
Yes, it’s hard to keep motivated
We should exercise caution in interpreting the findings. Unlike drug trials, participants in exercise trials know which “treatment” they’ve been randomised to receive, so this may skew the results.
Many people with depression have physical, psychological or social barriers to participating in formal exercise programs. And getting support to exercise isn’t free.
We also still don’t know the best way to stay motivated to exercise, which can be even harder if you have depression.
Our study tried to find out whether things like setting exercise goals helped, but we couldn’t get a clear result.
Other reviews found it’s important to have a clear action plan (for example, putting exercise in your calendar) and to track your progress (for example, using an app or smartwatch). But predicting which of these interventions work is notoriously difficult.
A 2021 mega-study of more than 60,000 gym-goers found experts struggled to predict which strategies might get people into the gym more often. Even making workouts fun didn’t seem to motivate people. However, listening to audiobooks while exercising helped a lot, which no experts predicted.
Still, we can be confident that people benefit from personalised support and accountability. The support helps overcome the hurdles they’re sure to hit. The accountability keeps people going even when their brains are telling them to avoid it.
So, when starting out, it seems wise to avoid going it alone. Instead:
- join a fitness group or yoga studio
get a trainer or an exercise physiologist
- ask a friend or family member to go for a walk with you.
Taking a few steps towards getting that support makes it more likely you’ll keep exercising.
Let’s make this official
Some countries see exercise as a backup plan for treating depression. For example, the American Psychological Association only conditionally recommends exercise as a “complementary and alternative treatment” when “psychotherapy or pharmacotherapy is either ineffective or unacceptable”.
Based on our research, this recommendation is withholding a potent treatment from many people who need it.
In contrast, The Royal Australian and New Zealand College of Psychiatrists recommends vigorous aerobic activity at least two to three times a week for all people with depression.
Given how common depression is, and the number failing to receive care, other countries should follow suit and recommend exercise alongside front-line treatments for depression.
I would like to acknowledge my colleagues Taren Sanders, Chris Lonsdale and the rest of the coauthors of the paper on which this article is based.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Michael Noetel, Senior Lecturer in Psychology, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why You Can’t Just “Get Over” Trauma
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Time does not, in fact, heal all wounds. Sometimes they even compound themselves over time. Dr. Tracey Marks explains the damage that trauma does—the physiological presentation of “the axe forgets but the tree remembers”—and how to heal from that actual damage.
The science of healing
Trauma affects the mind and body (largely because the brain is, of course, both—and affects pretty much everything else), which can ripple out into all areas of life.
On the physical level, brain areas affected by trauma include:
- Amygdalae: becomes hyperactive, keeping a person in a heightened state of vigilance.
- Hippocampi: can shrink, causing fragmented or missing memories.
- Prefrontal cortex: reduces in activity, impairing decision-making and emotional regulation.
Trauma also activates the body’s fight or flight response, releasing stress hormones like cortisol and adrenaline. These are great things to have a pinch, but having them elevated all the time is equivalent to only ever driving your car at top speed—the only question becomes whether you’ll crash and burn before you break down.
However, there is hope! Neuroplasticity (the brain’s ability to rewire itself) can make trauma recovery possible through various interventions.
Evidence-based therapies for trauma include:
- Eye Movement Desensitization and Reprocessing (EMDR): this can help reprocess traumatic memories and reduce emotional intensity.
- Trauma-focused Cognitive Behavioral Therapy (CBT): this can help change unhelpful thought patterns and includes exposure therapy.
- Somatic therapies: these focus on the body and nervous system to release stored tension.
In this latter category, embodiment is key to trauma recovery—this may sound “wishy-washy”, but the evidence shows that reconnecting with the body does help manage emotional stress responses. Mind-body practices like mindfulness, yoga, and breathwork help cultivate embodiment and reduce trauma-related stress.
In short: you can’t just “get over” it, but with the right support and interventions, it’s possible to rewire the brain and body toward resilience and healing.
For more on all of this from Dr. Marks, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- PTSD, But, Well…. Complex.
- Undoing The Damage Of Life’s Hard Knocks
- A Surprisingly Powerful Tool: Eye Movement Desensitization & Reprocessing
Take care!
Share This Post
-
The Sugary Food That Lowers Blood Sugars
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Loved the article on goji berries! I read they are good for blood sugars, is that true despite the sugar content?❞
Most berries are! Fruits that are high in polyphenols (even if they’re high in sugar), like berries, have a considerable net positive impact on glycemic health:
- Polyphenols and Glycemic Control
- Polyphenols and their effects on diabetes management: A review
- Dietary polyphenols as antidiabetic agents: Advances and opportunities
And more specifically:
Dietary berries, insulin resistance and type 2 diabetes: an overview of human feeding trials
Read more: Which Sugars Are Healthier, And Which Are Just The Same?
As for goji berries specifically, they’re very high indeed in polyphenols, and also have a hypoglycemic effect, i.e., they lower blood sugar levels (and as a bonus, increases HDL (“good” cholesterol) levels too, but that’s not the topic here):
❝The results of our study indicated a remarkable protective effect of LBP in patients with type 2 diabetes. Serum glucose was found to be significantly decreased and insulinogenic index increased during OMTT after 3 months administration of LBP. LBP also increased HDL levels in patients with type 2 diabetes. It showed more obvious hypoglycemic efficacy for those people who did not take any hypoglycemic medicine compared to patients taking hypoglycemic medicines. This study showed LBP to be a good potential treatment aided-agent for type 2 diabetes.❞
- LBP = Lycium barbarum polysaccharide, i.e. polysaccharide in/from goji berries
- OMTT = Oral metabolic tolerance test, a test of how well the blood sugars avoid spiking after a meal
For more about goji berries (and also where to get them), for reference our previous article is at:
Goji Berries: Which Benefits Do They Really Have?
Take care!
Share This Post
-
Amid Wildfire Trauma, L.A. County Dispatches Mental Health Workers to Evacuees
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PASADENA, Calif. — As Fernando Ramirez drove to work the day after the Eaton Fire erupted, smoke darkened the sky, ash and embers rained onto his windshield, and the air smelled of melting rubber and plastic.
He pulled to the side of the road and cried at the sight of residents trying to save their homes.
“I could see people standing on the roof, watering it, trying to protect it from the fire, and they just looked so hopeless,” said Ramirez, a community outreach worker with the Pasadena Public Health Department.
That evening, the 49-year-old volunteered for a 14-hour shift at the city’s evacuation center, as did colleagues who had also been activated for emergency medical duty. Running on adrenaline and little sleep after finding shelter for homeless people all day, Ramirez spent the night circulating among more than a thousand evacuees, offering wellness checks, companionship, and hope to those who looked distressed.
Local health departments, such as Ramirez’s, have become a key part of governments’ response to wildfires, floods, and other extreme weather events, which scientists say are becoming more intense and frequent due to climate change. The emotional toll of fleeing and possibly losing a home can help cause or exacerbate mental health conditions such as anxiety, depression, post-traumatic stress disorder, suicidal ideation, and substance use, according to health and climate experts.
Wildfires have become a recurring experience for many Angelenos, making it difficult for people to feel safe in their home or able to go about daily living, said Lisa Wong, director of the Los Angeles County Department of Mental Health. However, with each extreme weather event, the county has improved its support for evacuees, she said.
For instance, Wong said the county deployed a team of mental health workers trained to comfort evacuees without retraumatizing them, including by avoiding asking questions likely to bring up painful memories. The department has also learned to better track people’s health needs and redirect those who may find massive evacuation settings uncomfortable to other shelters or interim housing, Wong said. In those first days, the biggest goal is often to reduce people’s anxiety by providing them with information.
“We’ve learned that right when a crisis happens, people don’t necessarily want to talk about mental health,” said Wong, who staffed the evacuation site Jan. 8 with nine colleagues.
Instead, she and her team deliver a message of support: “This is really bad right now, but you’re not going to do this alone. We have a whole system set up for recovery too. Once you get past the initial shock of what happened — initial housing needs, medication needs, all those things — then there’s this whole pathway to recovery that we set up.”
The convention center in downtown Pasadena, which normally hosts home shows, comic cons, and trade shows, was transformed into an evacuation site with hundreds of cots. It was one of at least 13 shelters opened to serve more than 200,000 residents under evacuation orders.
The January wildfires have burned an estimated 64 square miles — an area larger than the city of Paris — and destroyed at least 12,300 buildings since they started Jan. 7. AccuWeather estimates the region will likely face more than $250 billion in economic losses from the blazes, surpassing the estimates from the state’s record-breaking 2020 wildfire season.
Lisa Patel, executive director of the Medical Society Consortium on Climate and Health, said she’s most concerned about low-income residents, who are less likely to access mental health support.
“There was a mental health crisis even before the pandemic,” said Patel, who is also a clinical associate professor of pediatrics at Stanford School of Medicine, referring to the covid-19 pandemic. “The pandemic made it worse. Now you lace in all of this climate change and these disasters into a health care system that isn’t set up to care for the people that already have mental health illness.”
Early research suggests exposure to large amounts of wildfire smoke can damage the brain and increase the risk of developing anxiety, she added.
At the Pasadena Convention Center, Elaine Santiago sat on a cot in a hallway as volunteers pulled wagons loaded with soup, sandwiches, bottled water, and other necessities.
Santiago said she drew comfort from being at the Pasadena evacuation center, knowing that she wasn’t alone in the tragedy.
“It sort of gives me a sense of peace at times,” Santiago said. “Maybe that’s weird. We’re all experiencing this together.”
She had been celebrating her 78th birthday with family when she fled her home in the small city of Sierra Madre, east of Pasadena. As she watched flames whip around her neighborhood, she, along with children and grandkids, scrambled to secure their dogs in crates and grabbed important documents before they left.
The widower had leaned on her husband in past emergencies, and now she felt lost.
“I did feel helpless,” Santiago said. “I figured I’m the head of the household; I should know what to do. But I didn’t know.”
Donny McCullough, who sat on a neighboring green cot draped in a Red Cross blanket, had fled his Pasadena home with his family early on the morning of Jan. 8. Without power at home, the 68-year-old stayed up listening for updates on a battery-powered radio. His eyes remained red from smoke irritation hours later.
“I had my wife and two daughters, and I was trying not to show fear, so I quietly, inside, was like, ‘Oh my God,’” said McCullough, a music producer and writer. “I’m driving away, looking at the house, wondering if it’s going to be the last time I’m going to see it.”
He saved his master recording from a seven-year music project, but he left behind his studio with all his other work from a four-decade career in music.
Not all evacuees arrived with family. Some came searching for loved ones. That’s one of the hardest parts of his shift, Ramirez said. The community outreach worker helped walk people around the building, cot by cot.
A week in, at least two dozen people had been killed in the wildfires.
The work takes a toll on disaster relief workers too. Ramirez said many feared losing their homes in the fires and some already had. He attends therapy weekly, which he said helps him manage his emotions.
At the evacuation center, Ramirez described being on autopilot.
“Some of us react differently. I tend to go into fight mode,” Ramirez said. “I react. I run towards the fire. I run towards personal service. Then once that passes, that’s when my trauma catches up with me.”
Need help? Los Angeles County residents in need of support can call the county’s mental health helpline at 1-800-854-7771. The national Suicide & Crisis Lifeline, 988, is also available for those who’d like to speak with someone confidentially, free of charge.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
The Kitchen Doctor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
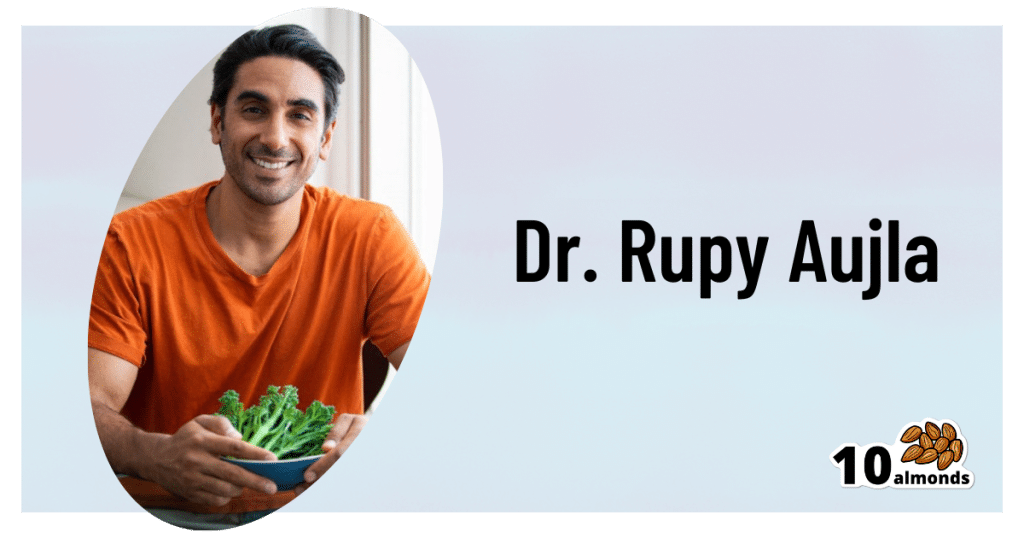
Dr. Rupy Aujla: The Kitchen Doctor
This is Dr. Rupy Aujla, and he’s a medical doctor. He didn’t set out to become a “health influencer”.
But then, a significant heart condition changed his life. Having a stronger motivation to learn more about nutritional medicine, he did a deep dive into the scientific literature, because that’s what you do when your life is on the line, especially if you’re a doctor!
Using what he learned, he was able to reverse his condition using a food and lifestyle approach. Now, he devotes himself to sharing what he learned—and what he continues to learn as he goes along.
One important thing he learned because of what happened to him, was that he hadn’t been paying enough attention to what his body was trying to tell him.
He wants us to know about interoception—which isn’t a Chris Nolan movie. Rather, interoception is the sense of what is going on inside one’s own body.
The counterpart of this is exteroception: our ability to perceive the outside world by means of our various senses.
Interoception is still using the senses, but is sensing internal body sensations. Effectively, the brain interprets and integrates what happens in our organs.
When interoception goes wrong, researchers found, it can lead to a greater likelihood of mental health problems. Having an anxiety disorder, depression, mood disorder, or an eating disorder often comes with difficulties in sensing what is going on inside the body.
Improving our awareness of body cues
Those same researchers suggested therapies and strategies aimed at improving awareness of mind-body connections. For example, mindfulness-based stress reduction, yoga, meditation and movement-based treatments. They could improve awareness of body cues by attending to sensations of breathing, cognitions and other body states.
But where Dr. Aujla puts his focus is “the heart of the home”, the kitchen.
The pleasure of food
❝Eating is not simply ingesting a mixture of nutrients. Otherwise, we would all be eating astronaut food. But food is not only a tool for health. It’s also an important pleasure in life, allowing us to connect to others, the present moment and nature.❞
Dr. Rupy Aujla
Dr. Aujla wants to help shift any idea of a separation between health and pleasure, because he believes in food as a positive route to well-being, joy and health. For him, it starts with self-awareness and acceptance of the sensory pleasures of eating and nourishing our bodies, instead of focusing externally on avoiding perceived temptations.
Most importantly:
We can use the pleasure of food as an ally to healthy eating.
Instead of spending our time and energy fighting the urge to eat unhealthy things that may present a “quick fix” to some cravings but aren’t what our body actually wants, needs, Dr. Aujla advises us to pay just a little more attention, to make sure the body’s real needs are met.
His top tips for such are:
- Create an enjoyable relaxing eating environment
To help cultivate positive emotions around food and signal to the nervous system a shift to food-processing time. Try setting the table with nothing else on it beyond what’s relevant to the dinner, putting away distractions, using your favorite plates, tablecloth, etc.
- Take 3 deep abdominal breaths before eating
To help you relax and ground yourself in the present moment, which in turn is to prepare your digestive system to receive and digest food.
- Pay attention to the way you sit
Take some time to sit comfortably with your feet grounded on the floor, not slouching, to give your stomach space to digest the food.
- Appreciate what it took to bring this food to your plate
Who was involved in the growing process and production, the weather and soil it took to grow the food, and where in the world it came from.
- Enjoy the sensations
When you’re cooking, serving, and eating your food, be attentive to color, texture, aroma and even sound. Taste the individual ingredients and seasonings along the way, when safe and convenient to do so.
- Journal
If you like journaling, you can try adding a mindful eating section to that. Ask questions such as: “how did I feel before, during, and after the meal?”
In closing…
Remember that this is a process, not only on an individual level but as a society too.
Oftentimes it’s hard to eat healthily… We can be given to wonder even “what is healthy, after all?”, and we can be limited by what is available, what is affordable, and what we have time to prepare.
But if we make a conscious commitment to make the best choices we reasonably can as we go along, then small changes can soon add up.
Interested in what kind of recipes Dr. Aujla goes for?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Never Enough – by Dr. Judith Grisel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about addiction before—specifically about alcohol, at least. This one’s more general in that it covers different addictions.
On the other hand, it’s also more specific, in that it covers them from the author’s field: neuroscience.
…and experience too. The author had a plethora of addictions (the serious kind), got sober, and then undertook to study neuroscience. Her hope was to help others avoid, or escape from the same as‚ what she went through.
Dr. Grisel (as she now is) takes a methodical approach in this book. She works her way through the addictive mechanisms of a broad selection of common drugs, explaining each.
The focus here is on neutral explanations, rather than the propagandizing scaremongering that failed at least one generation. Why each drug is alluring, what it really does do—and the neurological price it exacts, down to the molecular level.
She also covers risk factors for addiction; genetic, epigenetic, and environmental. There’s no “if you were stronger”, or “these people made bad choices”, so much as… Many addicts were, in effect, sabotaged from before birth.
That doesn’t mean that to become addicted or not is just fate, but it does mean… There but for the grace of factors completely outside of our control go we.
Why is this useful to us, be we a reader without any meaningful addiction (we’re not counting coffee etc here)? Well, as this book illustrates and explains, many of us could be one (more) mishap away from a crippling addiction and not know it. Forewarned is forearmed.
Bottom line: almost all of us are, have been, or will be touched by addiction in some way. Either directly, or a loved one, or a loved one’s loved one, or perhaps a parent who gave us an epigenetic misfortune. This book gives understanding that can help.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rapid Rise in Syphilis Hits Native Americans Hardest
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From her base in Gallup, New Mexico, Melissa Wyaco supervises about two dozen public health nurses who crisscross the sprawling Navajo Nation searching for patients who have tested positive for or been exposed to a disease once nearly eradicated in the U.S.: syphilis.
Infection rates in this region of the Southwest — the 27,000-square-mile reservation encompasses parts of Arizona, New Mexico, and Utah — are among the nation’s highest. And they’re far worse than anything Wyaco, who is from Zuni Pueblo (about 40 miles south of Gallup) and is the nurse consultant for the Navajo Area Indian Health Service, has seen in her 30-year nursing career.
Syphilis infections nationwide have climbed rapidly in recent years, reaching a 70-year high in 2022, according to the most recent data from the Centers for Disease Control and Prevention. That rise comes amid a shortage of penicillin, the most effective treatment. Simultaneously, congenital syphilis — syphilis passed from a pregnant person to a baby — has similarly spun out of control. Untreated, congenital syphilis can cause bone deformities, severe anemia, jaundice, meningitis, and even death. In 2022, the CDC recorded 231 stillbirths and 51 infant deaths caused by syphilis, out of 3,761 congenital syphilis cases reported that year.
And while infections have risen across the U.S., no demographic has been hit harder than Native Americans. The CDC data released in January shows that the rate of congenital syphilis among American Indians and Alaska Natives was triple the rate for African Americans and nearly 12 times the rate for white babies in 2022.
“This is a disease we thought we were going to eradicate not that long ago, because we have a treatment that works really well,” said Meghan Curry O’Connell, a member of the Cherokee Nation and chief public health officer at the Great Plains Tribal Leaders’ Health Board, who is based in South Dakota.
Instead, the rate of congenital syphilis infections among Native Americans (644.7 cases per 100,000 people in 2022) is now comparable to the rate for the entire U.S. population in 1941 (651.1) — before doctors began using penicillin to cure syphilis. (The rate fell to 6.6 nationally in 1983.)
O’Connell said that’s why the Great Plains Tribal Leaders’ Health Board and tribal leaders from North Dakota, South Dakota, Nebraska, and Iowa have asked federal Health and Human Services Secretary Xavier Becerra to declare a public health emergency in their states. A declaration would expand staffing, funding, and access to contact tracing data across their region.
“Syphilis is deadly to babies. It’s highly infectious, and it causes very severe outcomes,” O’Connell said. “We need to have people doing boots-on-the-ground work” right now.
In 2022, New Mexico reported the highest rate of congenital syphilis among states. Primary and secondary syphilis infections, which are not passed to infants, were highest in South Dakota, which had the second-highest rate of congenital syphilis in 2022. In 2021, the most recent year for which demographic data is available, South Dakota had the second-worst rate nationwide (after the District of Columbia) — and numbers were highest among the state’s large Native population.
In an October news release, the New Mexico Department of Health noted that the state had “reported a 660% increase in cases of congenital syphilis over the past five years.” A year earlier, in 2017, New Mexico reported only one case — but by 2020, that number had risen to 43, then to 76 in 2022.
Starting in 2020, the covid-19 pandemic made things worse. “Public health across the country got almost 95% diverted to doing covid care,” said Jonathan Iralu, the Indian Health Service chief clinical consultant for infectious diseases, who is based at the Gallup Indian Medical Center. “This was a really hard-hit area.”
At one point early in the pandemic, the Navajo Nation reported the highest covid rate in the U.S. Iralu suspects patients with syphilis symptoms may have avoided seeing a doctor for fear of catching covid. That said, he doesn’t think it’s fair to blame the pandemic for the high rates of syphilis, or the high rates of women passing infections to their babies during pregnancy, that continue four years later.
Native Americans are more likely to live in rural areas, far from hospital obstetric units, than any other racial or ethnic group. As a result, many do not receive prenatal care until later in pregnancy, if at all. That often means providers cannot test and treat patients for syphilis before delivery.
In New Mexico, 23% of patients did not receive prenatal care until the fifth month of pregnancy or later, or received fewer than half the appropriate number of visits for the infant’s gestational age in 2023 (the national average is less than 16%).
Inadequate prenatal care is especially risky for Native Americans, who have a greater chance than other ethnic groups of passing on a syphilis infection if they become pregnant. That’s because, among Native communities, syphilis infections are just as common in women as in men. In every other ethnic group, men are at least twice as likely to contract syphilis, largely because men who have sex with men are more susceptible to infection. O’Connell said it’s not clear why women in Native communities are disproportionately affected by syphilis.
“The Navajo Nation is a maternal health desert,” said Amanda Singer, a Diné (Navajo) doula and lactation counselor in Arizona who is also executive director of the Navajo Breastfeeding Coalition/Diné Doula Collective. On some parts of the reservation, patients have to drive more than 100 miles to reach obstetric services. “There’s a really high number of pregnant women who don’t get prenatal care throughout the whole pregnancy.”
She said that’s due not only to a lack of services but also to a mistrust of health care providers who don’t understand Native culture. Some also worry that providers might report patients who use illicit substances during their pregnancies to the police or child welfare. But it’s also because of a shrinking network of facilities: Two of the Navajo area’s labor and delivery wards have closed in the past decade. According to a recent report, more than half of U.S. rural hospitals no longer offer labor and delivery services.
Singer and the other doulas in her network believe New Mexico and Arizona could combat the syphilis epidemic by expanding access to prenatal care in rural Indigenous communities. Singer imagines a system in which midwives, doulas, and lactation counselors are able to travel to families and offer prenatal care “in their own home.”
O’Connell added that data-sharing arrangements between tribes and state, federal, and IHS offices vary widely across the country, but have posed an additional challenge to tackling the epidemic in some Native communities, including her own. Her Tribal Epidemiology Center is fighting to access South Dakota’s state data.
In the Navajo Nation and surrounding area, Iralu said, IHS infectious disease doctors meet with tribal officials every month, and he recommends that all IHS service areas have regular meetings of state, tribal, and IHS providers and public health nurses to ensure every pregnant person in those areas has been tested and treated.
IHS now recommends all patients be tested for syphilis yearly, and tests pregnant patients three times. It also expanded rapid and express testing and started offering DoxyPEP, an antibiotic that transgender women and men who have sex with men can take up to 72 hours after sex and that has been shown to reduce syphilis transmission by 87%. But perhaps the most significant change IHS has made is offering testing and treatment in the field.
Today, the public health nurses Wyaco supervises can test and treat patients for syphilis at home — something she couldn’t do when she was one of them just three years ago.
“Why not bring the penicillin to the patient instead of trying to drag the patient in to the penicillin?” said Iralu.
It’s not a tactic IHS uses for every patient, but it’s been effective in treating those who might pass an infection on to a partner or baby.
Iralu expects to see an expansion in street medicine in urban areas and van outreach in rural areas, in coming years, bringing more testing to communities — as well as an effort to put tests in patients’ hands through vending machines and the mail.
“This is a radical departure from our past,” he said. “But I think that’s the wave of the future.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: