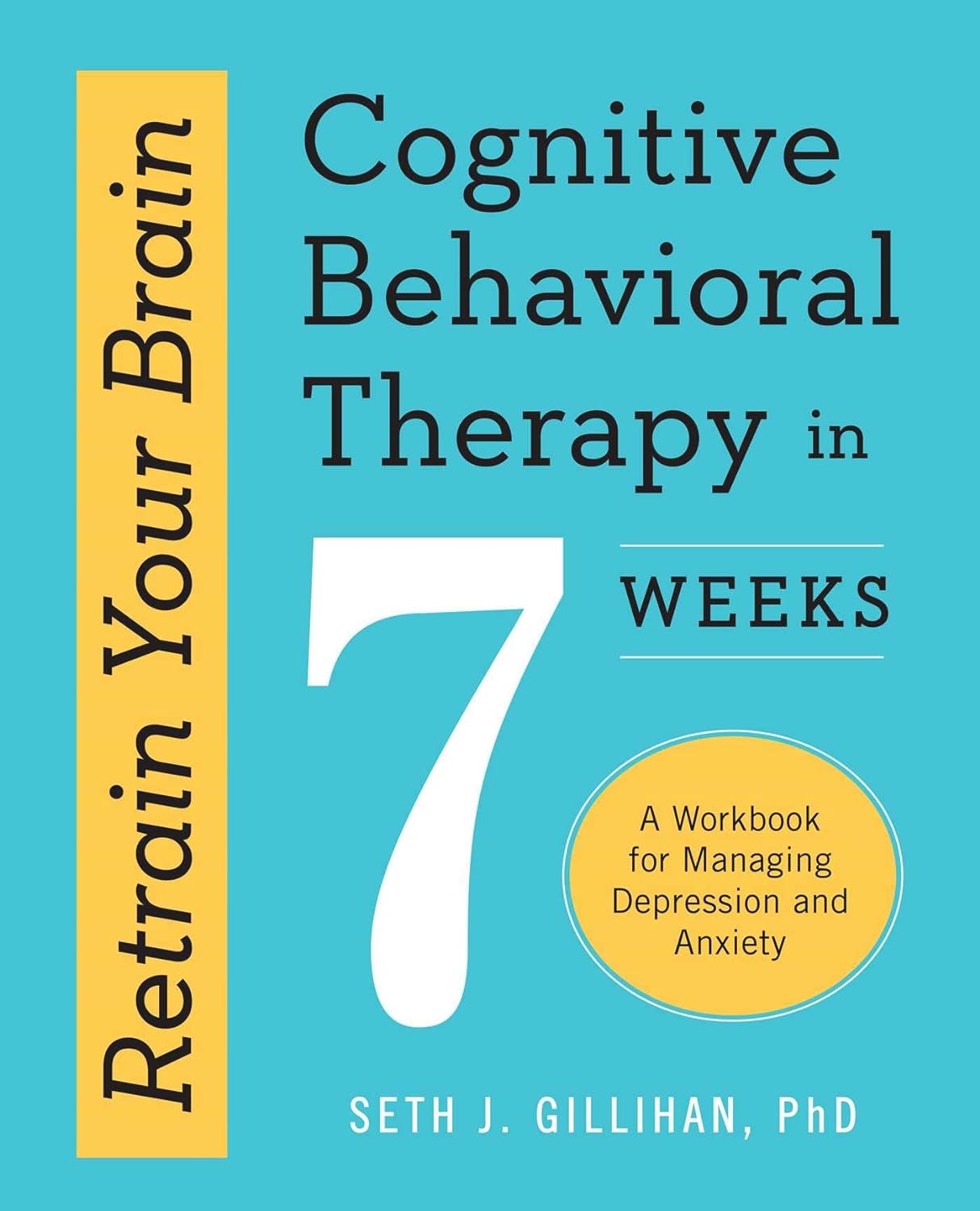
Retrain Your Brain – by Dr. Seth Gillihan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
15-Minute Arabic”, “Sharpen Your Chess Tactics in 24 Hours”, “Change Your Life in 7 Days”, “Cognitive Behavioral Therapy in 7 weeks”—all real books from this reviewer’s shelves.
The thing with books with these sorts of time periods in the titles is that the time period in the title often bears little relation to how long it takes to get through the book. So what’s the case here?
You’ll probably get through it in more like 7 days, but the pacing is more important than the pace. By that we mean:
Dr. Gillihan starts by assuming the reader is at best “in a rut”, and needs to first pick a direction to head in (the first “week”) and then start getting one’s life on track (the second “week”).
He then gives us, one by one, an array of tools and power-ups to do increasingly better. These tools aren’t just CBT, though of course that features prominently. There’s also mindfulness exercises, and holistic / somatic therapy too, for a real “bringing it all together” feel.
And that’s where this book excels—at no point is the reader left adrift with potential stumbling-blocks left unexamined. It’s a “whole course”.
Bottom line: whether it takes you 7 hours or 7 months, “Cognitive Behavioral Therapy in 7 Weeks” is a CBT-and-more course for people who like courses to work through. It’ll get you where you’re going… Wherever you want that to be for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
50 Ways To Rewire Your Anxious Brain – by Dr. Catherine Pittman & Dr. Maha Zayed-Hoffman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book is divided into sections:
- Calming the amygdala
- Rewiring the amygdala
- Calming the cortex
- Resisting cortex traps
…each with a dozen or so ways to do exactly what it says in the title: rewire your anxious brain.
The authors take the stance that since our brain is changing all the time, we might as well choose the direction we prefer. They then set out to provide the tools for the lay reader to do that, and (in that fourth section we mentioned) how to avoid accidentally doing the opposite, no matter how tempting doing the opposite may be.
For a book written by two PhD scientists where a large portion of it is about neuroscience, the style is very light pop science (just a few in-line citations every few pages, where they couldn’t resist the urge), and the focus is on being useful to the reader throughout. This all makes for reassuringly science-based but accessibly readable book.
The fact that the main material comes in the form of 50 very short chapters also makes it a lot more readable for those for whom sitting down to read a lot at a time can be off-putting.
Bottom line: if you experience anxiety and would like to experience it less, this book will guide you through how to get there.
Click here to check out 50 Ways To Rewire Your Anxious Brain, and rewire your anxious brain!
Share This Post
-
Mammography AI Can Cost Patients Extra. Is It Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As I checked in at a Manhattan radiology clinic for my annual mammogram in November, the front desk staffer reviewing my paperwork asked an unexpected question: Would I like to spend $40 for an artificial intelligence analysis of my mammogram? It’s not covered by insurance, she added.
I had no idea how to evaluate that offer. Feeling upsold, I said no. But it got me thinking: Is this something I should add to my regular screening routine? Is my regular mammogram not accurate enough? If this AI analysis is so great, why doesn’t insurance cover it?
I’m not the only person posing such questions. The mother of a colleague had a similar experience when she went for a mammogram recently at a suburban Baltimore clinic. She was given a pink pamphlet that said: “You Deserve More. More Accuracy. More Confidence. More power with artificial intelligence behind your mammogram.” The price tag was the same: $40. She also declined.
In recent years, AI software that helps radiologists detect problems or diagnose cancer using mammography has been moving into clinical use. The software can store and evaluate large datasets of images and identify patterns and abnormalities that human radiologists might miss. It typically highlights potential problem areas in an image and assesses any likely malignancies. This extra review has enormous potential to improve the detection of suspicious breast masses and lead to earlier diagnoses of breast cancer.
While studies showing better detection rates are extremely encouraging, some radiologists say, more research and evaluation are needed before drawing conclusions about the value of the routine use of these tools in regular clinical practice.
“I see the promise and I hope it will help us,” said Etta Pisano, a radiologist who is chief research officer at the American College of Radiology, a professional group for radiologists. However, “it really is ambiguous at this point whether it will benefit an individual woman,” she said. “We do need more information.”
The radiology clinics that my colleague’s mother and I visited are both part of RadNet, a company with a network of more than 350 imaging centers around the country. RadNet introduced its AI product for mammography in New York and New Jersey last February and has since rolled it out in several other states, according to Gregory Sorensen, the company’s chief science officer.
Sorensen pointed to research the company conducted with 18 radiologists, some of whom were specialists in breast mammography and some of whom were generalists who spent less than 75% of their time reading mammograms. The doctors were asked to find the cancers in 240 images, with and without AI. Every doctor’s performance improved using AI, Sorensen said.
Among all radiologists, “not every doctor is equally good,” Sorensen said. With RadNet’s AI tool, “it’s as if all patients get the benefit of our very top performer.”
But is the tech analysis worth the extra cost to patients? There’s no easy answer.
“Some people are always going to be more anxious about their mammograms, and using AI may give them more reassurance,” said Laura Heacock, a breast imaging specialist at NYU Langone Health’s Perlmutter Cancer Center in New York. The health system has developed AI models and is testing the technology with mammograms but doesn’t yet offer it to patients, she said.
Still, Heacock said, women shouldn’t worry that they need to get an additional AI analysis if it’s offered.
“At the end of the day, you still have an expert breast imager interpreting your mammogram, and that is the standard of care,” she said.
About 1 in 8 women will be diagnosed with breast cancer during their lifetime, and regular screening mammograms are recommended to help identify cancerous tumors early. But mammograms are hardly foolproof: They miss about 20% of breast cancers, according to the National Cancer Institute.
The FDA has authorized roughly two dozen AI products to help detect and diagnose cancer from mammograms. However, there are currently no billing codes radiologists can use to charge health plans for the use of AI to interpret mammograms. Typically, the federal Centers for Medicare & Medicaid Services would introduce new billing codes and private health plans would follow their lead for payment. But that hasn’t happened in this field yet and it’s unclear when or if it will.
CMS didn’t respond to requests for comment.
Thirty-five percent of women who visit a RadNet facility for mammograms pay for the additional AI review, Sorensen said.
Radiology practices don’t handle payment for AI mammography all in the same way.
The practices affiliated with Boston-based Massachusetts General Hospital don’t charge patients for the AI analysis, said Constance Lehman, a professor of radiology at Harvard Medical School who is co-director of the Breast Imaging Research Center at Mass General.
Asking patients to pay “isn’t a model that will support equity,” Lehman said, since only patients who can afford the extra charge will get the enhanced analysis. She said she believes many radiologists would never agree to post a sign listing a charge for AI analysis because it would be off-putting to low-income patients.
Sorensen said RadNet’s goal is to stop charging patients once health plans realize the value of the screening and start paying for it.
Some large trials are underway in the United States, though much of the published research on AI and mammography to date has been done in Europe. There, the standard practice is for two radiologists to read a mammogram, whereas in the States only one radiologist typically evaluates a screening test.
Interim results from the highly regarded MASAI randomized controlled trial of 80,000 women in Sweden found that cancer detection rates were 20% higher in women whose mammograms were read by a radiologist using AI compared with women whose mammograms were read by two radiologists without any AI intervention, which is the standard of care there.
“The MASAI trial was great, but will that generalize to the U.S.? We can’t say,” Lehman said.
In addition, there is a need for “more diverse training and testing sets for AI algorithm development and refinement” across different races and ethnicities, said Christoph Lee, director of the Northwest Screening and Cancer Outcomes Research Enterprise at the University of Washington School of Medicine.
The long shadow of an earlier and largely unsuccessful type of computer-assisted mammography hangs over the adoption of newer AI tools. In the late 1980s and early 1990s, “computer-assisted detection” software promised to improve breast cancer detection. Then the studies started coming in, and the results were often far from encouraging. Using CAD at best provided no benefit, and at worst reduced the accuracy of radiologists’ interpretations, resulting in higher rates of recalls and biopsies.
“CAD was not that sophisticated,” said Robert Smith, senior vice president of early cancer detection science at the American Cancer Society. Artificial intelligence tools today are a whole different ballgame, he said. “You can train the algorithm to pick up things, or it learns on its own.”
Smith said he found it “troubling” that radiologists would charge for the AI analysis.
“There are too many women who can’t afford any out-of-pocket cost” for a mammogram, Smith said. “If we’re not going to increase the number of radiologists we use for mammograms, then these new AI tools are going to be very useful, and I don’t think we can defend charging women extra for them.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Apple Cider Vinegar vs Balsamic Vinegar – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apple cider vinegar to balsamic vinegar, we picked the apple cider vinegar.
Why?
It’s close! And it’s a simple one today and they’re both great. Taking either for blood-sugar-balancing benefits is fine, as it’s the acidity that has this effect. But:
- Of the two, balsamic vinegar is the one more likely to contain more sugars, especially if it’s been treated in any fashion, and not by you, e.g. made into a glaze or even a reduction (the latter has no need to add sugar, but sometimes companies do because it is cheaper—so we recommend making your own balsamic vinegar reduction at home)
- Of the two, apple cider vinegar is the one more likely to contain “the mother”, that is to say, the part with extra probiotic benefits (but if the vinegar has been filtered, it won’t have this—it’s just more common to be able to find unfiltered apple cider vinegar, since it has more popular attention for its health benefits than balsamic vinegar does)
So, two wins for apple cider vinegar there.
Want to learn more?
You might like to read:
- 10 Ways To Balance Your Blood Sugars
- An Apple (Cider Vinegar) A Day…
- Apple Cider Vinegar vs Apple Cider Vinegar Gummies – Which is Healthier?
Take care!
Share This Post
Related Posts
-
Overcome Front-Of-Hip Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Alyssa Kuhn, physiotherapist, demonstrates how:
One, two, three…
One kind of pain affects a lot of related things: hip pain has an impact on everything that’s connected to the pelvis, which is basically the rest of the body, but especially the spine itself. For this reason, it’s critical to keep it in as good condition as possible.
Two primary causes of hip stiffness and pain:
- Anterior pelvic tilt due to posture, weight distribution, or pain. This tightens the front muscles and weakens the back muscles.
- Prolonged sitting, which tightens the hip muscles due to inactivity.
Three exercises are recommended by Dr. Kuhn to relieve pain and stiffness:
- Bridge exercise:
- Lie on a firm surface with your knees bent.
- Push through your feet, engage your hamstrings, and flatten your lower back.
- Hold for 3–5 seconds, relax, and repeat (10–20 reps).
- Wall exercise with arms:
- Stand with your lower back against the wall, feet a step away.
- Tilt your hips backwards, keeping your lower back in contact with the wall.
- Alternate lifting one arm at a time while maintaining back contact with the wall (10–20 reps).
- Wall exercise with legs:
- Same stance as the previous exercise but wider now.
- Lift one heel at a time while keeping your hips stable and your back against the wall.
- Practice for 30–60 seconds, maintaining good form.
As ever, consistency is key for long-term relief. Dr. Kuhn recommends doing these regularly, especially before any expected periods of prolonged sitting (e.g. at desk, or driving, etc). And of course, do try to reduce, or at least break up, those sitting marathons if you can.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
As Nuns Disappear, Many Catholic Hospitals Look More Like Megacorporations
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ST. LOUIS — Inside the more than 600 Catholic hospitals across the country, not a single nun can be found occupying a chief executive suite, according to the Catholic Health Association.
Nuns founded and led those hospitals in a mission to treat sick and poor people, but some were also shrewd business leaders. Sister Irene Kraus, a former chief executive of Daughters of Charity National Health System, was famous for coining the phrase “no margin, no mission.” It means hospitals must succeed — generating enough revenue to exceed expenses — to fulfill their original mission.
The Catholic Church still governs the care that can be delivered to millions in those hospitals each year, using religious directives to ban abortions and limit contraceptives, in vitro fertilization, and medical aid in dying.
But over time, that focus on margins led the hospitals to transform into behemoths that operate for-profit subsidiaries and pay their executives millions, according to hospital tax filings. These institutions, some of which are for-profit companies, now look more like other megacorporations than like the charities for the destitute of yesteryear.
The absence of nuns in the top roles raises the question, said M. Therese Lysaught, a Catholic moral theologist and professor at Loyola University Chicago: “What does it mean to be a Catholic hospital when the enterprise has been so deeply commodified?”
The St. Louis area serves as the de facto capital of Catholic hospital systems. Three of the largest are headquartered here, along with the Catholic hospital lobbying arm. Catholicism is deeply rooted in the region’s culture. During Pope John Paul II’s only U.S. stop in 1999, he led Mass downtown in a packed stadium of more than 100,000 people.
For a quarter century, Sister Mary Jean Ryan led SSM Health, one of those giant systems centered on St. Louis. Now retired, the 86-year-old said she was one of the last nuns in the nation to lead a Catholic hospital system.
Ryan grew up Catholic in Wisconsin and joined a convent while in nursing school in the 1960s, surprising her family. She admired the nuns she worked alongside and felt they were living out a higher purpose.
“They were very impressive,” she said. “Not that I necessarily liked all of them.”
Indeed, the nuns running hospitals defied the simplistic image often ascribed to them, wrote John Fialka in his book “Sisters: Catholic Nuns and the Making of America.”
“Their contributions to American culture are not small,” he wrote. “Ambitious women who had the skills and the stamina to build and run large institutions found the convent to be the first and, for a long time, the only outlet for their talents.”
This was certainly true for Ryan, who climbed the ranks, working her way from nurse to chief executive of SSM Health, which today has hospitals in Illinois, Missouri, Oklahoma, and Wisconsin.
The system was founded more than a century ago when five German nuns arrived in St. Louis with $5. Smallpox swept through the city and the Sisters of St. Mary walked the streets offering free care to the sick.
Their early foray grew into one of the largest Catholic health systems in the country, with annual revenue exceeding $10 billion, according to its 2023 audited financial report. SSM Health treats patients in 23 hospitals and co-owns a for-profit pharmacy benefit manager, Navitus, that coordinates prescriptions for 14 million people.
But Ryan, like many nuns in leadership roles in recent decades, found herself confronted with an existential crisis. As fewer women became nuns, she had to ensure the system’s future without them.
When Ron Levy, who is Jewish, started at SSM as an administrator, he declined to lead a prayer in a meeting, Ryan recounted in her book, “On Becoming Exceptional.”
“Ron, I’m not asking you to be Catholic,” she recalled telling him. “And I know you’ve only been here two weeks. So, if you’d like to make it three, I suggest you be prepared to pray the next time you’re asked.”
Levy went on to serve SSM for more than 30 years — praying from then on, Ryan wrote.
In Catholic hospitals, meetings are still likely to start with a prayer. Crucifixes often adorn buildings and patient rooms. Mission statements on the walls of SSM facilities remind patients: “We reveal the healing presence of God.”
Above all else, the Catholic faith calls on its hospitals to treat everyone regardless of race, religion, or ability to pay, said Diarmuid Rooney, a vice president of the Catholic Health Association. No nuns run the trade group’s member hospitals, according to the lobbying group. But the mission that compelled the nuns is “what compels us now,” Rooney said. “It’s not just words on a wall.”
The Catholic Health Association urges its hospitals to evaluate themselves every three years on whether they’re living up to Catholic teachings. It created a tool that weighs seven criteria, including how a hospital acts as an extension of the church and cares for poor and marginalized patients.
“We’re not relying on hearsay that the Catholic identity is alive and well in our facilities and hospitals,” Rooney said. “We can actually see on a scale where they are at.”
The association does not share the results with the public.
At SSM Health, “our Catholic identity is deeply and structurally ingrained” even with no nun at the helm, spokesperson Patrick Kampert said. The system reports to two boards. One functions as a typical business board of directors while the other ensures the system abides by the rules of the Catholic Church. The church requires the majority of that nine-member board to be Catholic. Three nuns currently serve on it; one is the chair.
Separately, SSM also is required to file an annual report with the Vatican detailing the ways, Kampert said, “we deepen our Catholic identity and further the healing ministry of Jesus.” SSM declined to provide copies of those reports.
From a business perspective, though, it’s hard to distinguish a Catholic hospital system like SSM from a secular one, said Ruth Hollenbeck, a former Anthem insurance executive who retired in 2018 after negotiating Missouri hospital contracts. In the contracts, she said, the difference amounted to a single paragraph stating that Catholic hospitals wouldn’t do anything contrary to the church’s directives.
To retain tax-exempt status under Internal Revenue Service rules, all nonprofit hospitals must provide a “benefit” to their communities such as free or reduced-price care for patients with low incomes. But the IRS provides a broad definition of what constitutes a community benefit, which gives hospitals wide latitude to justify not needing to pay taxes.
On average, the nation’s nonprofit hospitals reported that 15.5% of their total annual expenses were for community benefits in 2020, the latest figure available from the American Hospital Association.
SSM Health, including all of its subsidiaries, spent proportionately far less than the association’s average for individual hospitals, allocating roughly the same share of its annual expenses to community efforts over three years: 5.1% in 2020, 4.5% in 2021, and 4.9% in 2022, according to a KFF Health News analysis of its most recent publicly available IRS filings and audited financial statements.
A separate analysis from the Lown Institute think tank placed five Catholic systems — including the St. Louis region’s Ascension — on its list of the 10 health systems with the largest “fair share” deficits, which means receiving more in tax breaks than what they spent on the community. And Lown said three St. Louis-area Catholic health systems — Ascension, SSM Health, and Mercy — had fair share deficits of $614 million, $235 million, and $92 million, respectively, in the 2021 fiscal year.
Ascension, Mercy, and SSM disputed Lown’s methodology, arguing it doesn’t take into account the gap between the payments they receive for Medicaid patients and the cost of delivering their care. The IRS filings do.
But, Kampert said, many of the benefits SSM provides aren’t reflected in its IRS filings either. The forms reflect “very simplistic calculations” and do not accurately represent the health system’s true impact on the community, he said.
Today, SSM Health is led by longtime business executive Laura Kaiser. Her compensation in 2022 totaled $8.4 million, including deferred payments, according to its IRS filing. Kampert defended the amount as necessary “to retain and attract the most qualified” candidate.
By contrast, SSM never paid Ryan a salary, giving instead an annual contribution to her convent of less than $2 million a year, according to some tax filings from her long tenure. “I didn’t join the convent to earn money,” Ryan said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Magic of L-theanine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
All The Benefits Of Caffeine And More, Without The Drawbacks? What’s The Catch?
It just takes one extra supplement.
For many of us, our morning brew is practically a ritual, but caffeine can also cause all kinds of problems ranging from caffeine jitters to caffeine crashes to caffeine addiction and withdrawal. Surely, something could be better?
Well, yes it could! You doubtlessly know about green tea’s antioxidant properties, but its amino acid, l-theanine (which can be taken as a supplement with coffee, if you don’t enjoy green tea) has so much more to offer:
- L-theanine has been found to reduce stress responses—and let’s face it, when we most want/need a coffee is often when facing stress
- It also reduces anxiety, making it a very safe “downer” without the problems of, for example, alcohol—or other potentially addictive substances
- It’s far more than just that, though! Paradoxically, l-theanine also improves alertness (what other calming things promote alertness? Not so many)
- Part of its trick is that it also improves accuracy—whereas stimulants like caffeine may produce a twitchy, jumpy, responsiveness, l-theanine’s signature effect is a calm state of sharp readiness. Caffeine works by stimulating the adrenal gland and increasing blood pressure, while simultaneously blocking adenosine receptors so that your body doesn’t notice its own tiredness—which is why you’re likely to crash later, when the tiredness that had been masked, all hits at once. Instead, l-theanine taken with caffeine acts as a moderator of that, making for a longer, gentler curve. In terms of subjective experience, what this can mean for many people is: no more caffeine jitters!
- All this means that while l-theanine can boost all kinds of cognitive function, including alertness and accuracy, many like to take in the evening as it can also promote a good night’s sleep, ready to be at your best the next day.
- How much to take? 200mg is a commonly used dosage, which in supplement terms is usually a single capsule. A lot easier to take than the 40 cups of green tea that this dosage would otherwise be!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: