More research shows COVID-19 vaccines are safe for young adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Myocarditis, or inflammation of the heart muscle, is most commonly caused by a viral infection like COVID-19, not by vaccination.
- In line with previous research, a recent CDC study found no association between COVID-19 vaccination and sudden cardiac death in previously healthy young people.
- A COVID-19 infection is much more likely to cause inflammation of the heart muscle than a COVID-19 vaccine, and those cases are typically more severe.
Since the approval of the first COVID-19 vaccines, anti-vaccine advocates have raised concerns about heart muscle inflammation, also called myocarditis, after vaccination to suggest that vaccines are unsafe. They’ve also used concerns about myocarditis to spread false claims that vaccines cause sudden deaths, which is not true.
Research has consistently shown that cases of myocarditis after vaccination are extremely rare and usually mild, and a new study from the CDC found no association between sudden cardiac death and COVID-19 vaccination in young adults.
Read on to learn more about myocarditis and what the latest research says about COVID-19 vaccine safety.
What is myocarditis?
Myocarditis is inflammation of the myocardium, or the middle muscular layer of the heart wall. This inflammation weakens the heart’s ability to pump blood. Symptoms may include fatigue, shortness of breath, chest pain, rapid or irregular heartbeat, and flu-like symptoms.
Myocarditis may resolve on its own. In rare cases, it may lead to stroke, heart failure, heart attack, or death.
What causes myocarditis?
Myocarditis is typically caused by a viral infection like COVID-19. Bacteria, parasites, fungi, chemicals, and certain medications can also cause myocarditis.
In very rare cases, some people develop myocarditis after receiving a COVID-19 vaccine, but these cases are usually mild and resolve on their own. In contrast, a COVID-19 infection is much more likely to cause myocarditis, and those cases are typically more severe.
Staying up to date on vaccines reduces your risk of developing myocarditis from a COVID-19 infection.
Are COVID-19 vaccines safe for young people?
Yes. COVID-19 vaccines have been rigorously tested and monitored over the past three years and have been determined to be safe for everyone 6 months and older. A recent CDC study found no association between COVID-19 vaccination and sudden cardiac death in previously healthy young adults.
The benefits of vaccination outweigh any potential risks. Staying up to date on COVID-19 vaccines reduces your risk of severe illness, hospitalization, death, long COVID, and COVID-19-related complications, such as myocarditis.
The CDC recommends people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Growing Inequality in Life Expectancy Among Americans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The life expectancy among Native Americans in the western United States has dropped below 64 years, close to life expectancies in the Democratic Republic of the Congo and Haiti. For many Asian Americans, it’s around 84 — on par with life expectancies in Japan and Switzerland.
Americans’ health has long been unequal, but a new study shows that the disparity between the life expectancies of different populations has nearly doubled since 2000. “This is like comparing very different countries,” said Tom Bollyky, director of the global health program at the Council on Foreign Relations and an author of the study.
Called “Ten Americas,” the analysis published late last year in The Lancet found that “one’s life expectancy varies dramatically depending on where one lives, the economic conditions in that location, and one’s racial and ethnic identity.” The worsening health of specific populations is a key reason the country’s overall life expectancy — at 75 years for men and 80 for women — is the shortest among wealthy nations.
To deliver on pledges from the new Trump administration to make America healthy again, policymakers will need to fix problems undermining life expectancy across all populations.
“As long as we have these really severe disparities, we’re going to have this very low life expectancy,” said Kathleen Harris, a sociologist at the University of North Carolina. “It should not be that way for a country as rich as the U.S.”
Since 2000, the average life expectancy of many American Indians and Alaska Natives has been steadily shrinking. The same has been true since 2014 for Black people in low-income counties in the southeastern U.S.
“Some groups in the United States are facing a health crisis,” Bollyky said, “and we need to respond to that because it’s worsening.”
Heart disease, car fatalities, diabetes, covid-19, and other common causes of death are directly to blame. But research shows that the conditions of people’s lives, their behaviors, and their environments heavily influence why some populations are at higher risk than others.
Native Americans in the West — defined in the “Ten Americas” study as more than a dozen states excluding California, Washington, and Oregon — were among the poorest in the analysis, living in counties where a person’s annual income averages below about $20,000. Economists have shown that people with low incomes generally live shorter lives.
Studies have also linked the stress of poverty, trauma, and discrimination to detrimental coping behaviors like smoking and substance use disorders. And reservations often lack grocery stores and clean, piped water, which makes it hard to buy and cook healthy food.
About 1 in 5 Native Americans in the Southwest don’t have health insurance, according to a KFF report. Although the Indian Health Service provides coverage, the report says the program is weak due to chronic underfunding. This means people may delay or skip treatments for chronic illnesses. Postponed medical care contributed to the outsize toll of covid among Native Americans: About 1 of every 188 Navajo people died of the disease at the peak of the pandemic.
“The combination of limited access to health care and higher health risks has been devastating,” Bollyky said.
At the other end of the spectrum, the study’s category of Asian Americans maintained the longest life expectancies since 2000. As of 2021, it was 84 years.
Education may partly underlie the reasons certain groups live longer. “People with more education are more likely to seek out and adhere to health advice,” said Ali Mokdad, an epidemiologist at the Institute for Health Metrics and Evaluation at the University of Washington, and an author of the paper. Education also offers more opportunities for full-time jobs with health benefits. “Money allows you to take steps to take care of yourself,” Mokdad said.
The group with the highest incomes in most years of the analysis was predominantly composed of white people, followed by the mainly Asian group. The latter, however, maintained the highest rates of college graduation, by far. About half finished college, compared with fewer than a third of other populations.
The study suggests that education partly accounts for differences among white people living in low-income counties, where the individual income averaged less than $32,363. Since 2000, white people in low-income counties in southeastern states — defined as those in Appalachia and the Lower Mississippi Valley — had far lower life expectancies than those in upper midwestern states including Montana, Nebraska, and Iowa. (The authors provide details on how the groups were defined and delineated in their report.)
Opioid use and HIV rates didn’t account for the disparity between these white, low-income groups, Bollyky said. But since 2010, more than 90% of white people in the northern group were high school graduates, compared with around 80% in the southeastern U.S.
The education effect didn’t hold true for Latino groups compared with others. Latinos saw lower rates of high school graduation than white people but lived longer on average. This long-standing trend recently changed among Latinos in the Southwest because of covid. Hispanic or Latino and Black people were nearly twice as likely to die from the disease.
On average, Black people in the U.S. have long experienced worse health than other races and ethnicities in the United States, except for Native Americans. But this analysis reveals a steady improvement in Black people’s life expectancy from 2000 to about 2012. During this period, the gap between Black and white life expectancies shrank.
This is true for all three groups of Black people in the analysis: Those in low-income counties in southeastern states like Mississippi, Louisiana, and Alabama; those in highly segregated and metropolitan counties, such as Queens, New York, and Wayne, Michigan, where many neighborhoods are almost entirely Black or entirely white; and Black people everywhere else.
Better drugs to treat high blood pressure and HIV help account for the improvements for many Americans between 2000 to 2010. And Black people, in particular, saw steep rises in high school graduation and gains in college education in that period.
However, progress stagnated for Black populations by 2016. Disparities in wealth grew. By 2021, Asian and many white Americans had the highest incomes in the study, living in counties with per capita incomes around $50,000. All three groups of Black people in the analysis remained below $30,000.
A wealth gap between Black and white people has historical roots, stretching back to the days of slavery, Jim Crow laws, and policies that prevented Black people from owning property in neighborhoods that are better served by public schools and other services. For Native Americans, a historical wealth gap can be traced to a near annihilation of the population and mass displacement in the 19th and 20th centuries.
Inequality has continued to rise for several reasons, such as a widening pay gap between predominantly white corporate leaders and low-wage workers, who are disproportionately people of color. And reporting from KFF Health News shows that decisions not to expand Medicaid have jeopardized the health of hundreds of thousands of people living in poverty.
Researchers have studied the potential health benefits of reparation payments to address historical injustices that led to racial wealth gaps. One new study estimates that such payments could reduce premature death among Black Americans by 29%.
Less controversial are interventions tailored to communities. Obesity often begins in childhood, for example, so policymakers could invest in after-school programs that give children a place to socialize, be active, and eat healthy food, Harris said. Such programs would need to be free for children whose parents can’t afford them and provide transportation.
But without policy changes that boost low wages, decrease medical costs, put safe housing and strong public education within reach, and ensure access to reproductive health care including abortion, Harris said, the country’s overall life expectancy may grow worse.
“If the federal government is really interested in America’s health,” she said, “they could grade states on their health metrics and give them incentives to improve.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Long-acting contraceptives seem to be as safe as the pill when it comes to cancer risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many women worry hormonal contraceptives have dangerous side-effects including increased cancer risk. But this perception is often out of proportion with the actual risks.
So, what does the research actually say about cancer risk for contraceptive users?
And is your cancer risk different if, instead of the pill, you use long-acting reversible contraceptives? These include intrauterine devices or IUDs (such as Mirena), implants under the skin (such as Implanon), and injections (such as Depo Provera).
Our new study, conducted by the University of Queensland and QIMR Berghofer Medical Research Institute and published by the Journal of the National Cancer Institute, looked at this question.
We found long-acting contraceptives seem to be as safe as the pill when it comes to cancer risk (which is good news) but not necessarily any safer than the pill.
Peakstock/Shutterstock Some hormonal contraceptives take the form of implants under the skin. WiP-Studio/Shutterstock How does the contraceptive pill affect cancer risk?
The International Agency for Research on Cancer, which compiles evidence on cancer causes, has concluded that oral contraceptives have mixed effects on cancer risk.
Using the oral contraceptive pill:
- slightly increases your risk of breast and cervical cancer in the short term, but
- substantially reduces your risk of cancers of the uterus and ovaries in the longer term.
Our earlier work showed the pill was responsible for preventing far more cancers overall than it contributed to.
In previous research we estimated that in 2010, oral contraceptive pill use prevented over 1,300 cases of endometrial and ovarian cancers in Australian women.
It also prevented almost 500 deaths from these cancers in 2013. This is a reduction of around 25% in the deaths that could have occurred that year if women hadn’t taken the pill.
In contrast, we calculated the pill may have contributed to around 15 deaths from breast cancer in 2013, which is less than 0.5% of all breast cancer deaths in that year.
Previous work showed the pill was responsible for preventing far more cancers overall than it contributed to. Image Point Fr What about long-acting reversible contraceptives and cancer risk?
Long-acting reversible contraceptives – which include intrauterine devices or IUDs, implants under the skin, and injections – release progesterone-like hormones.
These are very effective contraceptives that can last from a few months (injections) up to seven years (intrauterine devices).
Notably, they don’t contain the hormone oestrogen, which may be responsible for some of the side-effects of the pill (including perhaps contributing to a higher risk of breast cancer).
Use of these long-acting contraceptives has doubled over the past decade, while the use of the pill has declined. So it’s important to know whether this change could affect cancer risk for Australian women.
Our new study of more than 1 million Australian women investigated whether long-acting, reversible contraceptives affect risk of invasive cancers. We compared the results to the oral contraceptive pill.
We used de-identified health records for Australian women aged 55 and under in 2002.
Among this group, about 176,000 were diagnosed with cancer between 2004 and 2013 when the oldest women were aged 67. We compared hormonal contraceptive use among these women who got cancer to women without cancer.
We found that long-term users of all types of hormonal contraception had around a 70% lower risk of developing endometrial cancer in the years after use. In other words, the risk of developing endometrial cancer is substantially lower among women who took hormonal contraception compared to those who didn’t.
For ovarian cancer, we saw a 50% reduced risk (compared to those who took no hormonal contraception) for women who were long-term users of the hormone-containing IUD.
The risk reduction was not as marked for the implants or injections, however few long-term users of these products developed these cancers in our study.
As the risk of endometrial and ovarian cancers increases with age, it will be important to look at cancer risk in these women as they get older.
What about breast cancer risk?
Our findings suggest that the risk of breast cancer for current users of long-acting contraceptives is similar to users of the pill.
However, the contraceptive injection was only associated with an increase in breast cancer risk after five years of use and there was no longer a higher risk once women stopped using them.
Our results suggested that the risk of breast cancer also reduces after stopping use of the contraceptive implants.
We will need to follow-up the women for longer to determine whether this is also the case for the IUD.
It is worth emphasising that the breast cancer risk associated with all hormonal contraceptives is very small.
About 30 in every 100,000 women aged 20 to 39 years develop breast cancer each year, and any hormonal contraceptive use would only increase this to around 36 cases per 100,000.
What about other cancers?
Our study did not show any consistent relationships between contraceptive use and other cancers types. However, we only at looked at invasive cancers (meaning those that start at a primary site but have the potential to spread to other parts of the body).
A recent French study found that prolonged use of the contraceptive injection increased the risk of meningioma (a type of benign brain tumour).
However, meningiomas are rare, especially in young women. There are around two cases in every 100,000 in women aged 20–39, so the extra number of cases linked to contraceptive injection use was small.
The French study found the hormonal IUD did not increase meningioma risk (and they did not investigate contraceptive implants).
Benefits and side-effects
There are benefits and side-effects for all medicines, including contraceptives, but it is important to know most very serious side-effects are rare.
A conversation with your doctor about the balance of benefits and side-effects for you is always a good place to start.
Susan Jordan, Professor of Epidemiology, The University of Queensland; Karen Tuesley, Postdoctoral Research Fellow, School of Public Health, The University of Queensland, and Penny Webb, Distinguished Scientist, Gynaecological Cancers Group, QIMR Berghofer Medical Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
7 Invisible Eating Disorders
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to assume that anyone with an eating disorder can be easily recognized by the resultantly atypical body composition, but it’s often not so.
Beyond the obvious
We’ll not keep them a mystery; the 7 invisible eating disorders discussed by therapist Kati Morton in this video are:
- OSFED (Other Specified Feeding or Eating Disorder): a catch-all diagnosis for those who don’t meet the criteria for more specific eating disorders but still have significant eating disorder behaviors.
- Atypical Anorexia: characterized by all the symptoms of anorexia nervosa (especially: intense fear of gaining weight, and body image distortion) except that the individual’s weight remains in a normal range.
- Atypical Bulimia: similar to bulimia nervosa, but the frequency or duration of binge-purge behaviors does not meet the usual diagnostic criteria and thus can fly under the radar.
- Atypical Binge-Eating Disorder: has episodes of consuming large amounts of food without compensatory behaviors (e.g. purging), but the episodes are less frequent and/or intense than typical binge-eating disorder.
- Purging Disorder: purging behaviors such as self-induced vomiting or laxative abuse without having binge-eating episodes (thus, this not being binging, and nothing obvious is happening outside of the bathroom).
- Night Eating Syndrome: consuming excessive amounts of food during the night while being fully aware of the nature of the eating episodes, which disrupts sleep and leads to guilt.
- Rumination Disorder: repeatedly regurgitating food, which may be rechewed, reswallowed, or spat out, without nausea or involuntary retching, often as a self-soothing mechanism.
For more on each of these, along with a case study-style example of each, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Eating Disorders: More Varied (And Prevalent) Than People Think
Take care!
Share This Post
Related Posts
-
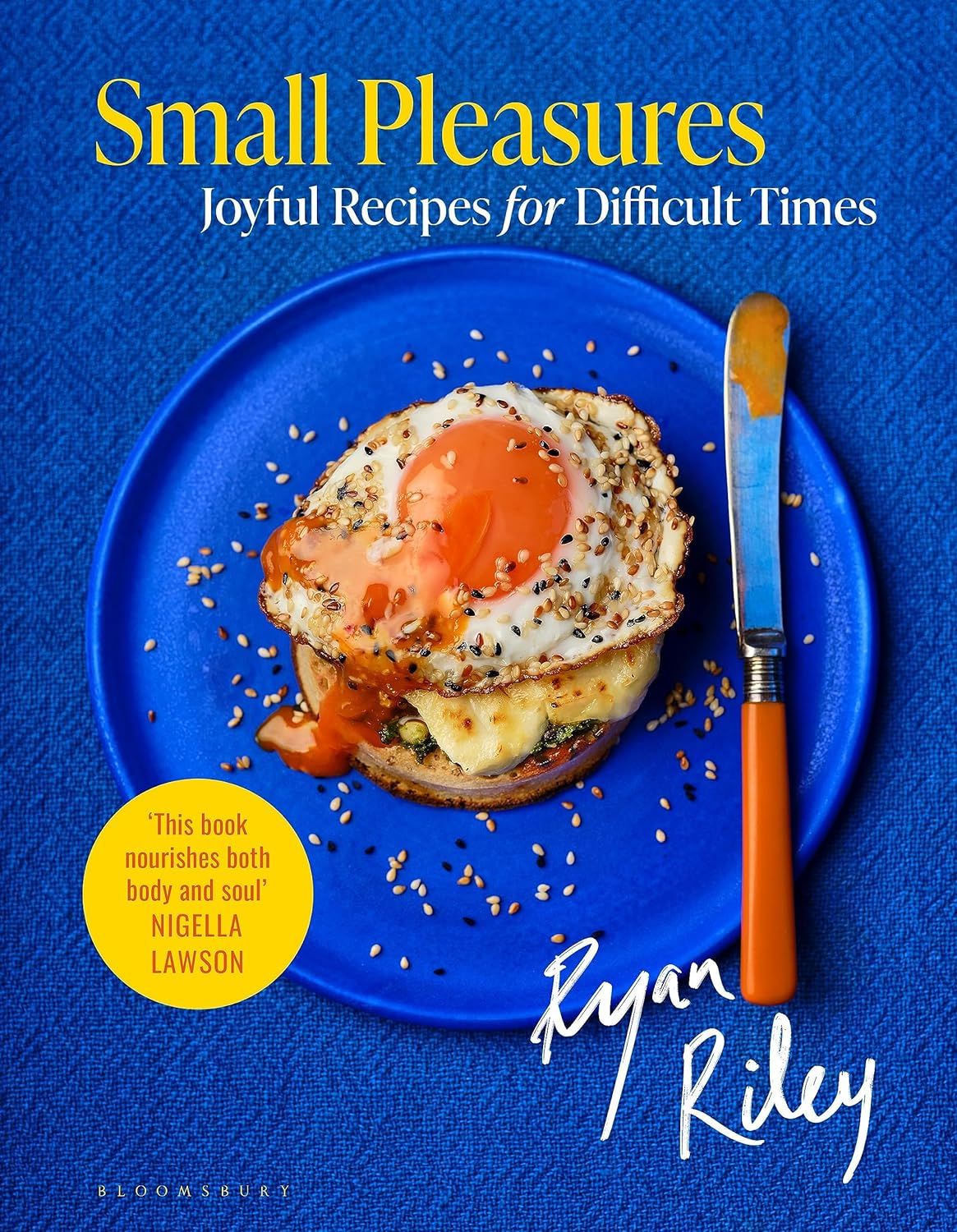
Small Pleasures – by Ryan Riley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Hippocrates said “let food be thy medicine, and let medicine be thy food”, he may or may not have had this book in mind.
In terms of healthiness, this one’s not the very most nutritionist-approved recipe book we’ve ever reviewed. It’s not bad, to be clear!
But the physical health aspect is secondary to the mental health aspects, in this one, as you’ll see. And as we say, “mental health is also just health”.
The book is divided into three sections:
- Comfort—for when you feel at your worst, for when eating is a chore, for when something familiar and reassuring will bring you solace. Here we find flavor and simplicity; pastas, eggs, stews, potato dishes, and the like.
- Restoration—for when your energy needs reawakening. Here we find flavors fresh and tangy, enlivening and bright. Things to make you feel alive.
- Pleasure—while there’s little in the way of health-food here, the author describes the dishes in this section as “a love letter to yourself; they tell you that you’re special as you ready yourself to return to the world”.
And sometimes, just sometimes, we probably all need a little of that.
Bottom line: if you’d like to bring a little more joie de vivre to your cuisine, this book can do that.
Click here to check out Small Pleasures, and rekindle joy in your kitchen!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
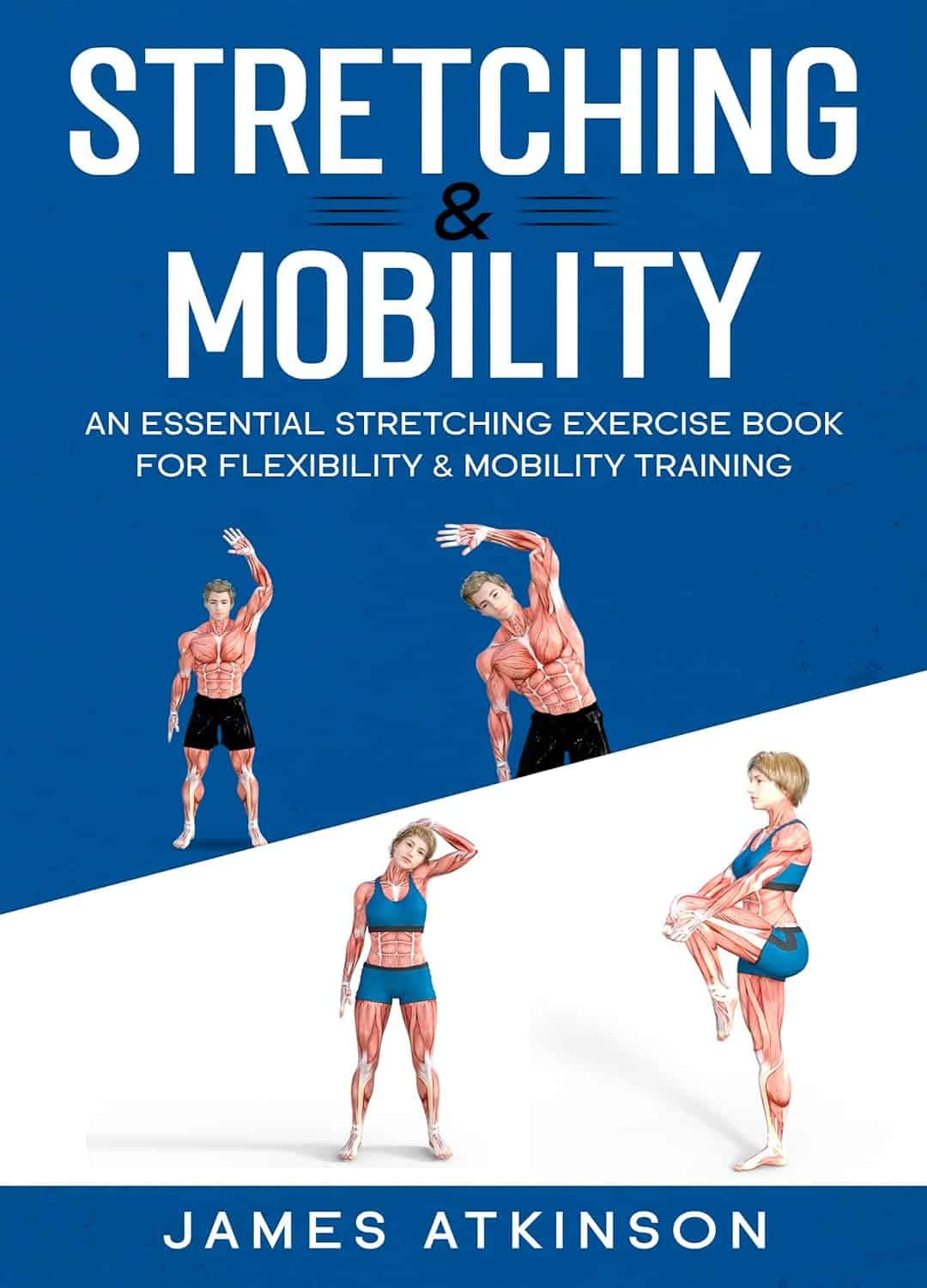
Stretching & Mobility – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“I will stretch for just 10 minutes per day”, we think, and do our best. Then there are a plethora of videos saying “Stretching mistakes that you are making!” and it turns out we haven’t been doing them in a way that actually helps.
This book fixes that. Unlike some books of the genre, it’s not full of jargon and you won’t need an anatomy and physiology degree to understand it. It is, however, dense in terms of the information it gives—it’s not padded out at all; it contains a lot of value.
The stretches are all well-explained and well-illustrated; the cover art will give you an idea of the anatomical illustration style contained with in.
Atkinson also gives workout plans, so that we know we’re not over- or under-training or trying to do too much or missing important things out.
Bottom line: if you’re looking to start a New Year routine to develop better suppleness, this book is a great primer for that.
Click here to check out Stretching and Mobility, and improve yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Delicious Daily Daal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’re not obliged to eat this every day, but you might want to. The reason we called this one this, is because it’s a super simple recipe (don’t be put off by the long ingredients list; it’s mostly spices making it look long) which, after you’ve done it a couple of times, you could practically do it in your sleep quickly and easily.
The name “lentil daal” is a bit like “naan bread”—a redundant tautology repeated more than once unnecessarily, but it helps for international clarity. The dish is usually served with naan, by the way, and rice. We don’t have room for those today, maybe we’ll do them another day; for now, you can just cook rice how you normally do, and buy naan if necessary.
Writer’s note: I love strong flavors; many people don’t. For this reason I’m going to give a “basic” version. Please feel free to multiply the spices if you feel so inclined. Where I give “one teaspoon” of a spice below, I’d use a tablespoon at home. Chili peppers can vary in heat a lot even within the same type, so what I do for any given batch is taste one (raw), judge the heat, and use an appropriate number of peppers accordingly. If you don’t want to do that, I suggest just guessing low (as per the instructions below) and if you find at the end you want more heat, you can always stir in a little hot sauce. I know that sounds heretical, but at the end of the day, the primary goal of cooking is to have the meal you want at the end of it.
You will need
- 1 1/2 cups red lentils
- 1 large onion, chopped
- 1 large bulb garlic, minced
- 1 oz ginger, grated
- 2 hot peppers (e.g. serrano), chopped
- 1 tsp ground cumin
- 1 tsp ground coriander
- 1 tsp ground turmeric
- 1 tsp garam masala (this is also ground, but it doesn’t come any other way)
- 1 tsp chili flakes (omit if you’re not a fan of heat)
- 2 tsp cracked black pepper
- 1 tsp salt ← I wouldn’t recommend multiplying this one unless later, to taste. In fact, instead of 1 tsp salt I use 2 tsp MSG, which has less sodium than 1 tsp salt. But “1 tsp salt” is the “easy to find in the store” version.
- 2 large or 3 small tomatoes, chopped (or 1 can chopped tomatoes)
- 2 shallots, thinly sliced
- 1 tsp cumin seeds
- 1 tsp mustard seeds
- 1 tsp coriander seeds
- 1 tsp black peppercorns
- 1 lime
- 1/2 cup fresh cilantro, or if you have the “that tastes like soap” gene, parsley, chopped
- Coconut oil for cooking (if you don’t like coconut, consider springing for avocado oil—if you use olive oil, it’ll add an olivey taste which changes the dish a lot; not inherently bad, but it feels a lot less like traditional daal; seed oils are less healthy and we don’t recommend them; ghee is a traditional option and not bad in moderation, but not as healthy as the oils we mentioned first)
- Water for cooking the lentils
Method
(we suggest you read everything at least once before doing anything)
1) In a saucepan, boil water and add the lentils; let them simmer while doing the next things.
2) Sauté the onions until translucent. This should only take a few minutes.
3) Add the garlic, ginger, and hot peppers, and keep stirring for another couple of minutes.
4) Add the ground spices (cumin, coriander, turmeric, garam masala) chili flakes, and cracked black pepper, as well as the salt or MSG if using (not both), and stir them in quickly but thoroughly.
For the next step, you may need to transfer to larger pan if your sauté pan isn’t big enough to take the volume; if so, that’s fine, the sauté has done its job and can have a rest now. If your sauté pan is big enough, just carry on in the same pan; this is perfect.
5) Add the lentils with the water you cooked them in (there might not be much water left now, as the lentils will have absorbed a lot of it; this is fine) as well as the chopped tomatoes.
6) Simmer until it has the consistency of a very thick sauce (you can add a splash more water here and there if it seems to need more). In the West it’s common to serve lentils “al dente”, but in the East it’s usual to (for dishes like this) cook them until they start to
7) Add the juice of at least 1/2 of your lime, or the whole lime if you feel so inclined.
8) In a pre-heated skillet, flash-fry the sliced shallots and the seeds (cumin, coriander, mustard, black peppercorns) at the hottest temperature you can muster. Don’t worry if the oil smokes; we’re only going to be at this tadka-making stage for a moment and nothing will stick provided you keep it moving. When the seeds start popping, it’s ready. Add it all to the big pan and stir in.
9) Add the cilantro-or-parsley garnish once you’re ready to serve.
Enjoy!
Learn more
For those interested in some of the science of what we have going on today:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- How Much Spice Is Right?
- Tasty Polyphenols
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: