Quick Healthy Recipe Ideas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
“It was superb !! Just loved that healthy recipe !!! I would love to see one of those every day, if possible !! Keep up the fabulous work !!! ”
We’re glad you enjoyed! We can’t promise a recipe every day, but here’s one just for you:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Your Eyes Say About Your Health (If You Have A Mirror, You Can Do This Now!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In an age when doctors are increasingly pressed to get you out of their office quickly and not take the time to do thorough tests, having a good basic knowledge of signs and symptoms of disease has become more important than ever for all of us:
The eyes have it:
Dr. Siobhan Deshauer is back, this time working with Dr. Maria Howard, a Canadian optometrist, who advised behind-the-scenes to ensure the best information about these signs and symptoms and what they tell us:
- Color blindness test: Ishihara color test identifies color blindness; in the version in the video, seeing “74” is normal, “12” indicates red-green color blindness, and no numbers suggest complete color blindness due to genetics or retinal/optic nerve issues.
- Yellow sclera (scleral icterus): yellow sclera indicates high bilirubin from excessive red blood cell breakdown, liver damage, bile duct blockage, or Gilbert syndrome.
- Blue sclera: indicates thin collagen in the sclera, which can be linked to osteogenesis imperfecta, Ehlers-Danlos syndrome, and Marfan syndrome.
- Pink eye: caused by infections, autoimmune diseases, or trauma; persistent symptoms or associated pain/vision changes need medical evaluation.
- Physiologic diplopia (double vision): normal test where fingers appear doubled when focusing on different planes; absence may indicate amblyopia.
- Pinhole test (visual acuity): looking through a small pinhole can determine if glasses are needed for clearer vision.
- Nearsighted vs farsighted: nearsightedness risks retinal tears and night vision issues, while farsightedness increases the risk of glaucoma.
- Eye color and health: brown eyes lower cancer risk but higher cataract risk; light eyes higher cancer risk but lower cataract risk; sudden changes may indicate a condition.
- Kayser-Fleischer rings: golden-brown rings around the iris suggest copper buildup from Wilson disease, treatable with chelation therapy.
- Corneal arcus: gray/white ring around the iris indicates cholesterol buildup, normal with aging but concerning in younger individuals, signaling hypercholesterolemia or artery narrowing.
- Limbal rings: dark rings around the iris are generally aesthetic and not health-related.
- Red desaturation test: a difference in red color perception between eyes may indicate optic nerve or retinal issues.
- Eye twitching: often linked to stress, sleep deprivation, or caffeine; persistent twitching or muscle involvement requires medical attention.
- Pupillary reflex: pupil constriction in light; abnormal responses suggest trauma, overdose, or poisoning.
- Cataracts: lens cloudiness due to age, UV exposure, smoking, diabetes, or prednisone; also occurs sometimes in youth due to conditions like diabetes.
- Yellow spots (pinguecula and pterygium): sun damage, wind, and dust exposure cause yellow spots; protect with sunglasses to prevent progression impacting vision.
- Dark spots in the eye: includes freckles, moles (nevi), and melanoma; changes require medical evaluation.
- Hypnotic induction profile: eye roll test assesses susceptibility to hypnosis.
- Floaters: normal clumps in the eye; sudden increases, flashes, or curtain-like effects may signal retinal detachment.
- Retinal detachment: caused by aging-related vitreous shrinkage; treated with lasers, gas bubbles, or retinal buckles.
- Macular degeneration (Amsler grid test): wavy, fuzzy lines or missing vision spots may indicate this condition.
- Giant cell arteritis: no, that’s not a typo: rather it is about blood vessel inflammation that can cause blindness; treated with prednisone, symptoms include headaches and vision changes.
- Near point of convergence: focus test to detect convergence issues common with excessive screen time.
- Blepharitis: eyelid inflammation causing itchiness, burning, or flaky skin; treated with hygiene, antibiotics, or tea tree oil.
- Proptosis (Graves’ disease): bulging eyes due to hyperthyroidism; treatable with medications, radiation, or surgery.
- Ptosis (droopy eyelids): indicates myasthenia gravis, temporarily improved with the ice pack test.
- Night vision issues: caused by retinal problems or high myopia, not typically vitamin A deficiency in developed countries.
- Dry eyes: caused by screen time, smoking, medications, or autoimmune diseases; managed with lubricating drops, reduced screen time, and adjustments.
- Watery eyes: caused by irritation or blocked tear ducts; treated with lubricating drops or surgery.
- Retinoblastoma: rare childhood cancer detectable through flash photography showing one white pupil; early detection enables treatment.
For more on all of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
What Your Hands Can Tell You About Your Health
Take care!
Share This Post
-
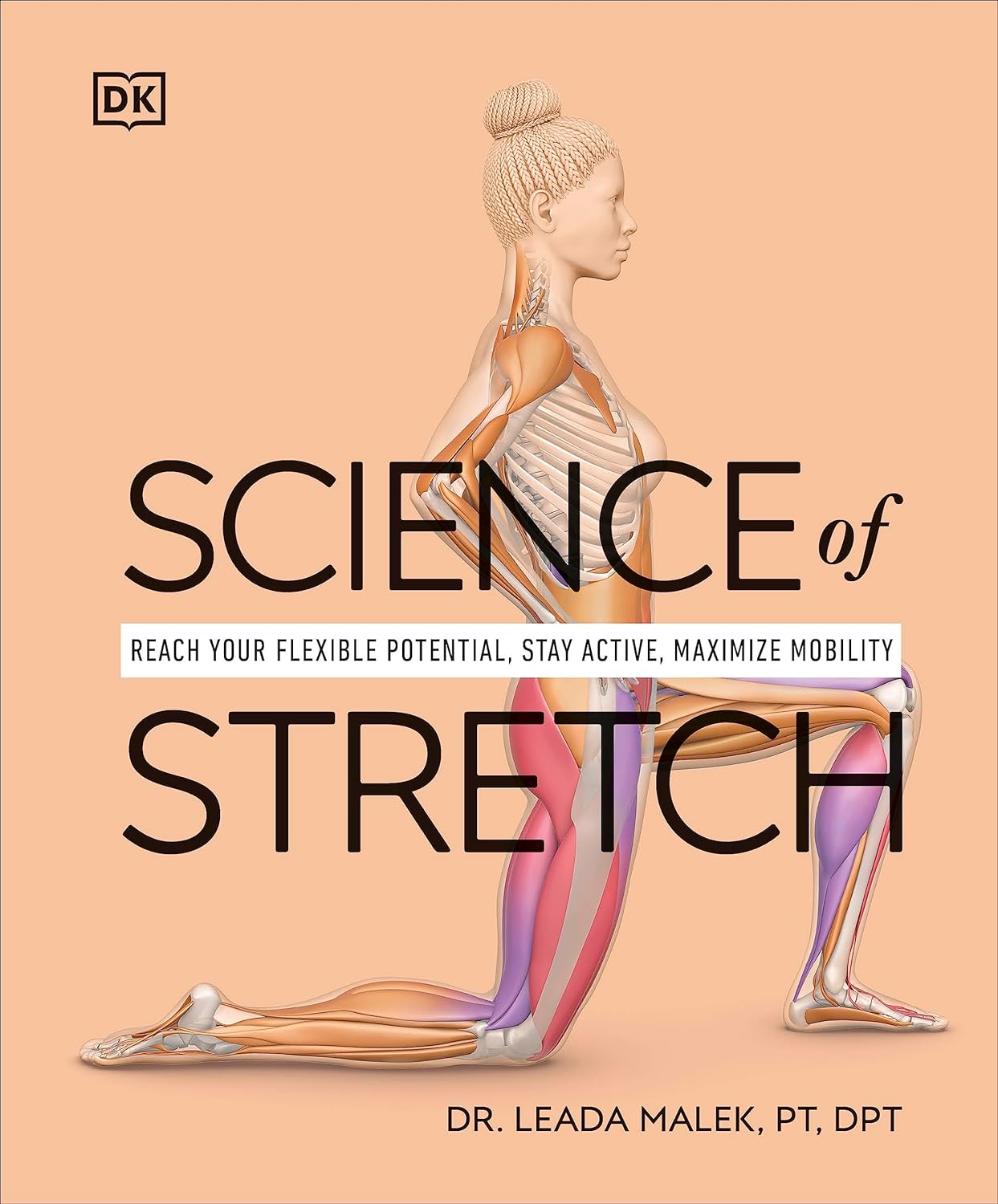
Science of Stretch – by Dr. Leada Malek
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is part of a “Science of…” series, of which we’ve reviewed some others before (Yoga | HIIT | Pilates), and needless to say, we like them.
You may be wondering: is this just that thing where a brand releases the same content under multiple names to get more sales, and no, it’s not (long-time 10almonds readers will know: if it were, we’d say so!).
While flexibility and mobility are indeed key benefits in yoga and Pilates, they looked into the science of what was going on in yoga asanas and Pilates exercises, stretchy or otherwise, so the stretching element was not nearly so deep as in this book.
In this one, Dr. Malek takes us on a wonderful tour of (relevant) human anatomy and physiology, far deeper than most pop-science books go into when it comes to stretching, so that the reader can really understand every aspect of what’s going on in there.
This is important, because it means busting a lot of myths (instead of busting tendons and ligaments and things), understanding why certain things work and (critically!) why certain things don’t, how certain stretching practices will sabotage our progress, things like that.
It’s also beautifully clearly illustrated! The cover art is a fair representation of the illustrations inside.
Bottom line: if you want to get serious about stretching, this is a top-tier book and you won’t regret it.
Click here to check out Science of Stretching, and learn what you can do and how!
Share This Post
-
Stop Cancer 20 Years Ago
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Get Abreast And Keep Abreast
This is Dr. Jenn Simmons. Her specialization is integrative oncology, as she—then a breast cancer surgeon—got breast cancer, decided the system wasn’t nearly as good from the patients’ side of things as from the doctors’ side, and took to educate herself, and now others, on how things can be better.
What does she want us to know?
Start now
If you have breast cancer, the best time to start adjusting your lifestyle might be 20 years ago, but the second-best time is now. We realize our readers with breast cancer (or a history thereof) probably have indeed started already—all strength to you.
What this means for those of us without breast cancer (or a history therof) is: start now
Even if you don’t have a genetic risk factor, even if there’s no history of it in your family, there’s just no reason not to start now.
Start what, you ask? Taking away its roots. And how?
Inflammation as the root of cancer
To oversimplify: cancer occurs because an accidentally immortal cell replicates and replicates and replicates and takes any nearby resources to keep on going. While science doesn’t know all the details of how this happens, it is a factor of genetic mutation (itself a normal process, without which evolution would be impossible), something which in turn is accelerated by damage to the DNA. The damage to the DNA? That occurs (often as not) as a result of cellular oxidation. Cellular oxidation is far from the only genotoxic thing out there, and a lot of non-food “this thing causes cancer” warnings are usually about other kinds of genotoxicity. But cellular oxidation is a big one, and it’s one that we can fight vigorously with our lifestyle.
Because cellular oxidation and inflammation go hand-in-hand, reducing one tends to reduce the other. That’s why so often you’ll see in our Research Review Monday features, a line that goes something like:
“and now for those things that usually come together: antioxidant, anti-inflammatory, anticancer, and anti-aging”
So, fight inflammation now, and have a reduced risk of a lot of other woes later.
See: How to Prevent (or Reduce) Inflammation
Don’t settle for “normal”
People are told, correctly but not always helpfully, such things as:
- It’s normal to have less energy at your age
- It’s normal to have a weaker immune system at your age
- It’s normal to be at a higher risk of diabetes, heart disease, etc
…and many more. And these things are true! But that doesn’t mean we have to settle for them.
We can be all the way over on the healthy end of the distribution curve. We can do that!
(so can everyone else, given sufficient opportunity and resources, because health is not a zero-sum game)
If we’re going to get a cancer diagnosis, then our 60s are the decade where we’re most likely to get it. Earlier than that and the risk is extant but lower; later than that and technically the risk increases, but we probably got it already in our 60s.
So, if we be younger than 60, then now’s a good time to prepare to hit the ground running when we get there. And if we missed that chance, then again, the second-best time is now:
See: Focusing On Health In Our Sixties
Fast to live
Of course, anything can happen to anyone at any age (alas), but this is about the benefits of living a fasting lifestyle—that is to say, not just fasting for a 4-week health kick or something, but making it one’s “new normal” and just continuing it for life.
This doesn’t mean “never eat”, of course, but it does mean “practice intermittent fasting, if you can”—something that Dr. Simmons strongly advocates.
See: Intermittent Fasting: We Sort The Science From The Hype
While this calls back to the previous “fight inflammation”, it deserves its own mention here as a very specific way of fighting it.
It’s never too late
All of the advices that go before a cancer diagnosis, continue to stand afterwards too. There is no point of “well, I already have cancer, so what’s the harm in…?”
The harm in it after a diagnosis will be the same as the harm before. When it comes to lifestyle, preventing a cancer and preventing it from spreading are very much the same thing, which is also the same as shrinking it. Basically, if it’s anticancer, it’s anticancer, no matter whether it’s before, during, or after.
Dr. Simmons has seen too many patients get a diagnosis, and place their lives squarely in the hands of doctors, when doctors can only do so much.
Instead, Dr. Simmons recommends taking charge of your health as best you are able, today and onwards, no matter what. And that means two things:
- Knowing stuff
- Doing stuff
So it becomes our responsibility (and our lifeline) to educate ourselves, and take action accordingly.
Want to know more?
We recently reviewed her book, and heartily recommend it:
The Smart Woman’s Guide to Breast Cancer – by Dr. Jenn Simmons
Enjoy!
Share This Post
Related Posts
-
The Oh She Glows Cookbook – by Angela Liddon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s get the criticism out of the way first: notwithstanding the subtitle promising over 100 recipes, there are about 80-odd here, if we discount recipes that are no-brainer things like smoothies, sides such as for example “roasted garlic”, or meta-ingredients such as oat flour (instructions: blend the oats and you get oat flour).
The other criticism is more subjective: if you are like this reviewer, you will want to add more seasonings than recommended to most of the recipes. But that’s easy enough to do.
As for the rest: this is a very healthy cookbook, and quite wide-ranging and versatile, with recipes that are homely, with a lot of emphasis on comfort foods (but still, healthy), though certainly some are perfectly worthy of entertaining too.
A nice bonus of this book is that it offers a lot of available substitutions (much like we do at 10almonds), and also ways of turning the recipe into something else entirely with just a small change. This trait more than makes up for the slight swindle in terms of number of recipes, since some of the recipes have bonus recipes snuck in.
Bottom line: if you’d like to broaden your plant-based cooking range, this book is a fine option for expanding your repertoire.
Click here to check out The Oh She Glows Cookbook, and indeed glow!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fast. Feast. Repeat – by Dr. Gin Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed intermittent fasting books before, so what makes this one different?
The title “Fast. Feast. Repeat.” doesn’t give much away; after all, we already know that that’s what intermittent fasting is.
After taking the reader though the basics of how intermittent fasting works and what it does for the body, much of the rest of the book is given over to improvements.
That’s what the real strength of this book is: ways to make intermittent fasting more efficient, including how to avoid plateaus. After all, sometimes it can seem like the only way to push further with intermittent fasting is to restrict the eating window further. Not so!
Instead, Dr. Stephens gives us ways to keep confusing our metabolism (in a good way) if, for example, we had a weight loss goal we haven’t met yet.
Best of all, this comes without actually having to eat less.
Bottom line: if you want to be in good physical health, and/but also believe that life is for living and you enjoy eating food, then this book can resolve that age-old dilemma!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
In the Realm of Hungry Ghosts – by Dr. Gabor Maté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books by Dr. Maté before, and this one’s about addiction. We’ve reviewed books about addiction before too, so what makes this one different?
Wow, is this one so different. Most books about addiction are about “beating” it. Stop drinking, quit sugar, etc. And, that’s all well and good. It is definitely good to do those things. But this one’s about understanding it, deeply. Because, as Dr. Maté makes very clear, “there, but for the grace of epigenetics and environmental factors, go we”.
Indeed, most of us will have addictions; they’re (happily) just not too problematic for most of us, being either substances that are not too harmful (e.g. coffee), or behavioral addictions that aren’t terribly impacting our lives (e.g. Dr. Maté’s compulsion to keep buying more classical music, which he then tries to hide from his wife).
The book does also cover a lot of much more serious addictions, the kind that have ruined lives, and the kind that definitely didn’t need to, if people had been given the right kind of help—instead of, all too often, they got the opposite.
Perhaps the greatest value of this book is that; understanding what creates addiction in the first place, what maintains it, and what help people actually need.
Bottom line: if you’d like more insight into the human aspect of addiction without getting remotely wishy-washy, this book is probably the best one out there.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: