Statistical Models vs. Front-Line Workers: Who Knows Best How to Spend Opioid Settlement Cash?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
MOBILE, Ala. — In this Gulf Coast city, addiction medicine doctor Stephen Loyd announced at a January event what he called “a game-changer” for state and local governments spending billions of dollars in opioid settlement funds.
The money, which comes from companies accused of aggressively marketing and distributing prescription painkillers, is meant to tackle the addiction crisis.
But “how do you know that the money you’re spending is going to get you the result that you need?” asked Loyd, who was once hooked on prescription opioids himself and has become a nationally known figure since Michael Keaton played a character partially based on him in the Hulu series “Dopesick.”
Loyd provided an answer: Use statistical modeling and artificial intelligence to simulate the opioid crisis, predict which programs will save the most lives, and help local officials decide the best use of settlement dollars.
Loyd serves as the unpaid co-chair of the Helios Alliance, a group that hosted the event and is seeking $1.5 million to create such a simulation for Alabama.
The state is set to receive more than $500 million from opioid settlements over nearly two decades. It announced $8.5 million in grants to various community groups in early February.
Loyd’s audience that gray January morning included big players in Mobile, many of whom have known one another since their school days: the speaker pro tempore of Alabama’s legislature, representatives from the city and the local sheriff’s office, leaders from the nearby Poarch Band of Creek Indians, and dozens of addiction treatment providers and advocates for preventing youth addiction.
Many of them were excited by the proposal, saying this type of data and statistics-driven approach could reduce personal and political biases and ensure settlement dollars are directed efficiently over the next decade.
But some advocates and treatment providers say they don’t need a simulation to tell them where the needs are. They see it daily, when they try — and often fail — to get people medications, housing, and other basic services. They worry allocating $1.5 million for Helios prioritizes Big Tech promises for future success while shortchanging the urgent needs of people on the front lines today.
“Data does not save lives. Numbers on a computer do not save lives,” said Lisa Teggart, who is in recovery and runs two sober living homes in Mobile. “I’m a person in the trenches,” she said after attending the Helios event. “We don’t have a clean-needle program. We don’t have enough treatment. … And it’s like, when is the money going to get to them?”
The debate over whether to invest in technology or boots on the ground is likely to reverberate widely, as the Helios Alliance is in discussions to build similar models for other states, including West Virginia and Tennessee, where Loyd lives and leads the Opioid Abatement Council.
New Predictive Promise?
The Helios Alliance comprises nine nonprofit and for-profit organizations, with missions ranging from addiction treatment and mathematical modeling to artificial intelligence and marketing. As of mid-February, the alliance had received $750,000 to build its model for Alabama.
The largest chunk — $500,000 — came from the Poarch Band of Creek Indians, whose tribal council voted unanimously to spend most of its opioid settlement dollars to date on the Helios initiative. A state agency chipped in an additional $250,000. Ten Alabama cities and some private foundations are considering investing as well.
Stephen McNair, director of external affairs for Mobile, said the city has an obligation to use its settlement funds “in a way that is going to do the most good.” He hopes Helios will indicate how to do that, “instead of simply guessing.”
Rayford Etherton, a former attorney and consultant from Mobile who created the Helios Alliance, said he is confident his team can “predict the likely success or failure of programs before a dollar is spent.”
The Helios website features a similarly bold tagline: “Going Beyond Results to Predict Them.”
To do this, the alliance uses system dynamics, a mathematical modeling technique developed at the Massachusetts Institute of Technology in the 1950s. The Helios model takes in local and national data about addiction services and the drug supply. Then it simulates the effects different policies or spending decisions can have on overdose deaths and addiction rates. New data can be added regularly and new simulations run anytime. The alliance uses that information to produce reports and recommendations.
Etherton said it can help officials compare the impact of various approaches and identify unintended consequences. For example, would it save more lives to invest in housing or treatment? Will increasing police seizures of fentanyl decrease the number of people using it or will people switch to different substances?
And yet, Etherton cautioned, the model is “not a crystal ball.” Data is often incomplete, and the real world can throw curveballs.
Another limitation is that while Helios can suggest general strategies that might be most fruitful, it typically can’t predict, for instance, which of two rehab centers will be more effective. That decision would ultimately come down to individuals in charge of awarding contracts.
Mathematical Models vs. On-the-Ground Experts
To some people, what Helios is proposing sounds similar to a cheaper approach that 39 states — including Alabama — already have in place: opioid settlement councils that provide insights on how to best use the money. These are groups of people with expertise ranging from addiction medicine and law enforcement to social services and personal experience using drugs.
Even in places without formal councils, treatment providers and recovery advocates say they can perform a similar function. Half a dozen advocates in Mobile told KFF Health News the city’s top need is low-cost housing for people who want to stop using drugs.
“I wonder how much the results” from the Helios model “are going to look like what people on the ground doing this work have been saying for years,” said Chance Shaw, director of prevention for AIDS Alabama South and a person in recovery from opioid use disorder.
But Loyd, the co-chair of the Helios board, sees the simulation platform as augmenting the work of opioid settlement councils, like the one he leads in Tennessee.
Members of his council have been trying to decide how much money to invest in prevention efforts versus treatment, “but we just kind of look at it, and we guessed,” he said — the way it’s been done for decades. “I want to know specifically where to put the money and what I can expect from outcomes.”
Jagpreet Chhatwal, an expert in mathematical modeling who directs the Institute for Technology Assessment at Massachusetts General Hospital, said models can reduce the risk of individual biases and blind spots shaping decisions.
If the inputs and assumptions used to build the model are transparent, there’s an opportunity to instill greater trust in the distribution of this money, said Chhatwal, who is not affiliated with Helios. Yet if the model is proprietary — as Helios’ marketing materials suggest its product will be — that could erode public trust, he said.
Etherton, of the Helios Alliance, told KFF Health News, “Everything we do will be available publicly for anyone who wants to look at it.”
Urgent Needs vs. Long-Term Goals
Helios’ pitch sounds simple: a small upfront cost to ensure sound future decision-making. “Spend 5% so you get the biggest impact with the other 95%,” Etherton said.
To some people working in treatment and recovery, however, the upfront cost represents not just dollars, but opportunities lost for immediate help, be it someone who couldn’t find an open bed or get a ride to the pharmacy.
“The urgency of being able to address those individual needs is vital,” said Pamela Sagness, executive director of the North Dakota Behavioral Health Division.
Her department recently awarded $7 million in opioid settlement funds to programs that provide mental health and addiction treatment, housing, and syringe service programs because that’s what residents have been demanding, she said. An additional $52 million in grant requests — including an application from the Helios Alliance — went unfunded.
Back in Mobile, advocates say they see the need for investment in direct services daily. More than 1,000 people visit the office of the nonprofit People Engaged in Recovery each month for recovery meetings, social events, and help connecting to social services. Yet the facility can’t afford to stock naloxone, a medication that can rapidly reverse overdoses.
At the two recovery homes that Mobile resident Teggart runs, people can live in a drug-free space at a low cost. She manages 18 beds but said there’s enough demand to fill 100.
Hannah Seale felt lucky to land one of those spots after leaving Mobile County jail last November.
“All I had with me was one bag of clothes and some laundry detergent and one pair of shoes,” Seale said.
Since arriving, she’s gotten her driver’s license, applied for food stamps, and attended intensive treatment. In late January, she was working two jobs and reconnecting with her 4- and 7-year-old daughters.
After 17 years of drug use, the recovery home “is the one that’s worked for me,” she said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blood-Brain Barrier Breach Blamed For Brain-Fog
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Move Over, Leaky Gut. Now It’s A Leaky Brain.
…which is not a headline that promises good news, and indeed, the only good news about this currently is “now we know another thing that’s happening, and thus can work towards a treatment for it”.
Back in February (most popular media outlets did not rush to publish this, as it rather goes against the narrative of “remember when COVID was a thing?” as though the numbers haven’t risen since the state of emergency was declared over), a team of Irish researchers made a discovery:
❝For the first time, we have been able to show that leaky blood vessels in the human brain, in tandem with a hyperactive immune system may be the key drivers of brain fog associated with long covid❞
~ Dr. Matthew Campbell (one of the researchers)
Let’s break that down a little, borrowing some context from the paper itself:
- the leaky blood vessels are breaching the blood-brain-barrier
- that’s a big deal, because that barrier is our only filter between our brain and Things That Definitely Should Not Go In The Brain™
- a hyperactive immune system can also be described as chronic inflammation
- in this case, that includes chronic neuroinflammation which, yes, is also a major driver of dementia
You may be wondering what COVID has to do with this, and well:
- these blood-brain-barrier breaches were very significantly associated (in lay terms: correlated, but correlated is only really used as an absolute in write-ups) with either acute COVID infection, or Long Covid.
- checking this in vitro, exposure of brain endothelial cells to serum from patients with Long Covid induced the same expression of inflammatory markers.
How important is this?
As another researcher (not to mention: professor of neurology and head of the school of medicine at Trinity) put it:
❝The findings will now likely change the landscape of how we understand and treat post-viral neurological conditions.
It also confirms that the neurological symptoms of long covid are measurable with real and demonstrable metabolic and vascular changes in the brain.❞
~ Dr. Colin Doherty (see mini-bio above)
You can read a pop-science article about this here:
Irish researchers discover underlying cause of “brain fog” linked with long covid
…and you can read the paper in full here:
Want to stay safe?
Beyond the obvious “get protected when offered boosters/updates” (see also: The Truth About Vaccines), other good practices include the same things most people were doing when the pandemic was big news, especially avoiding enclosed densely-populated places, washing hands frequently, and looking after your immune system. For that latter, see also:
Beyond Supplements: The Real Immune-Boosters!
Take care!
Share This Post
- the leaky blood vessels are breaching the blood-brain-barrier
-
Kiwi vs Passion Fruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
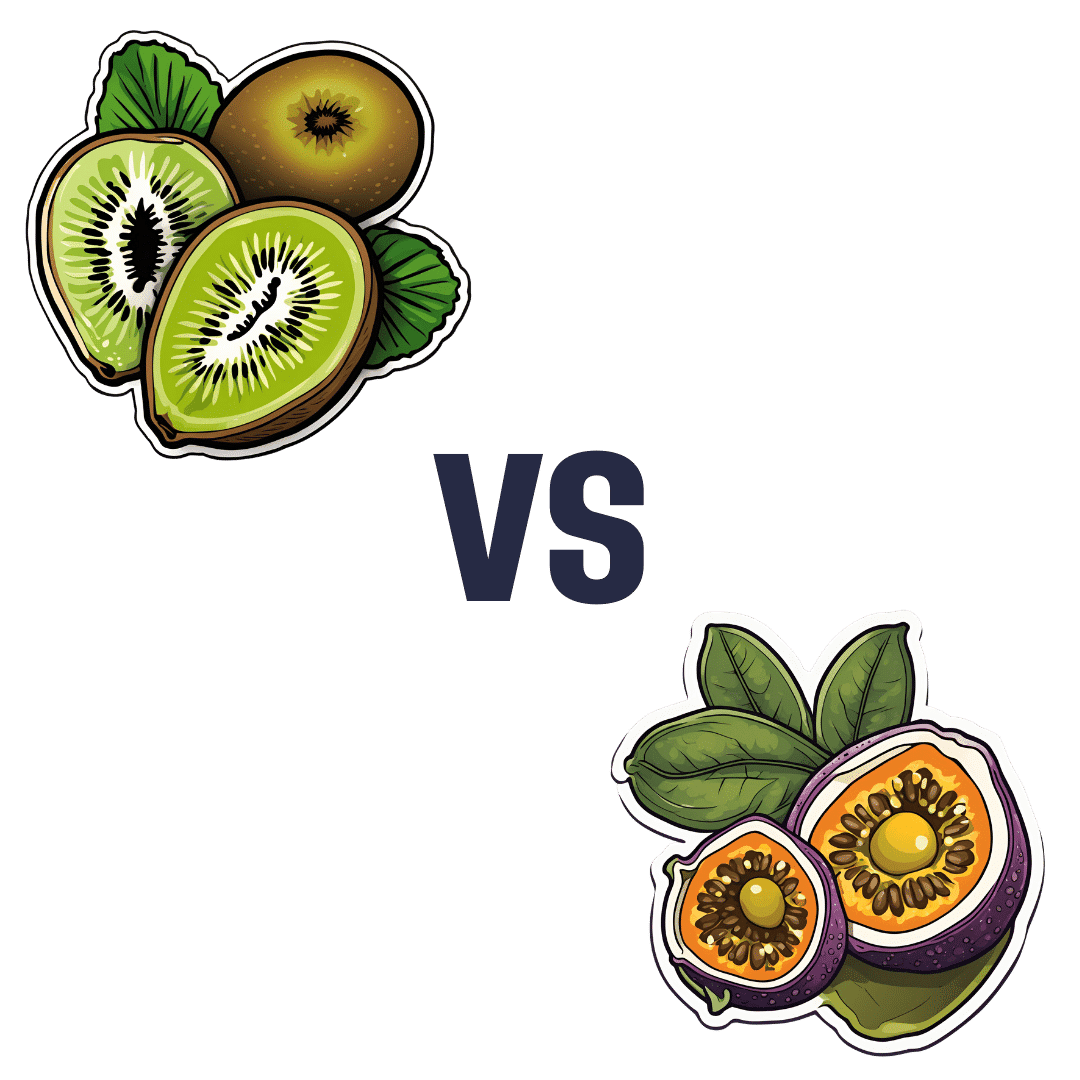
When comparing kiwi to passion fruit, we picked the passion fruit.
Why?
This fruit is so passionate about delivery nutrient-dense goodness, that at time of writing, nothing has beaten it yet!
In terms of macros, passion fruit has a little more protein, as well as 50% more carbs, and/but more than 3x the fiber. That last stat is particularly impressive, and also results in passion fruit having a much lower glycemic index, too. In short, a clear win for passion fruit in the macros category.
In the category of vitamins, kiwi has more of vitamins B9, C, E, and K, while passion fruit has more of vitamins A, B2, B3, and B6, making for a tie this time.
As for minerals, kiwi has more calcium, copper, manganese, and zinc, while passion fruit has more iron, magnesium, phosphorus, potassium, and selenium, resulting in a modest, marginal win for passion fruit in this category.
Adding up the categories gives a convincing win for passion fruit, but by all means enjoy either or both; diversity is good! And kiwi has its merits too (for example, it’s particularly high in vitamin K, appropriately enough).
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Share This Post
-
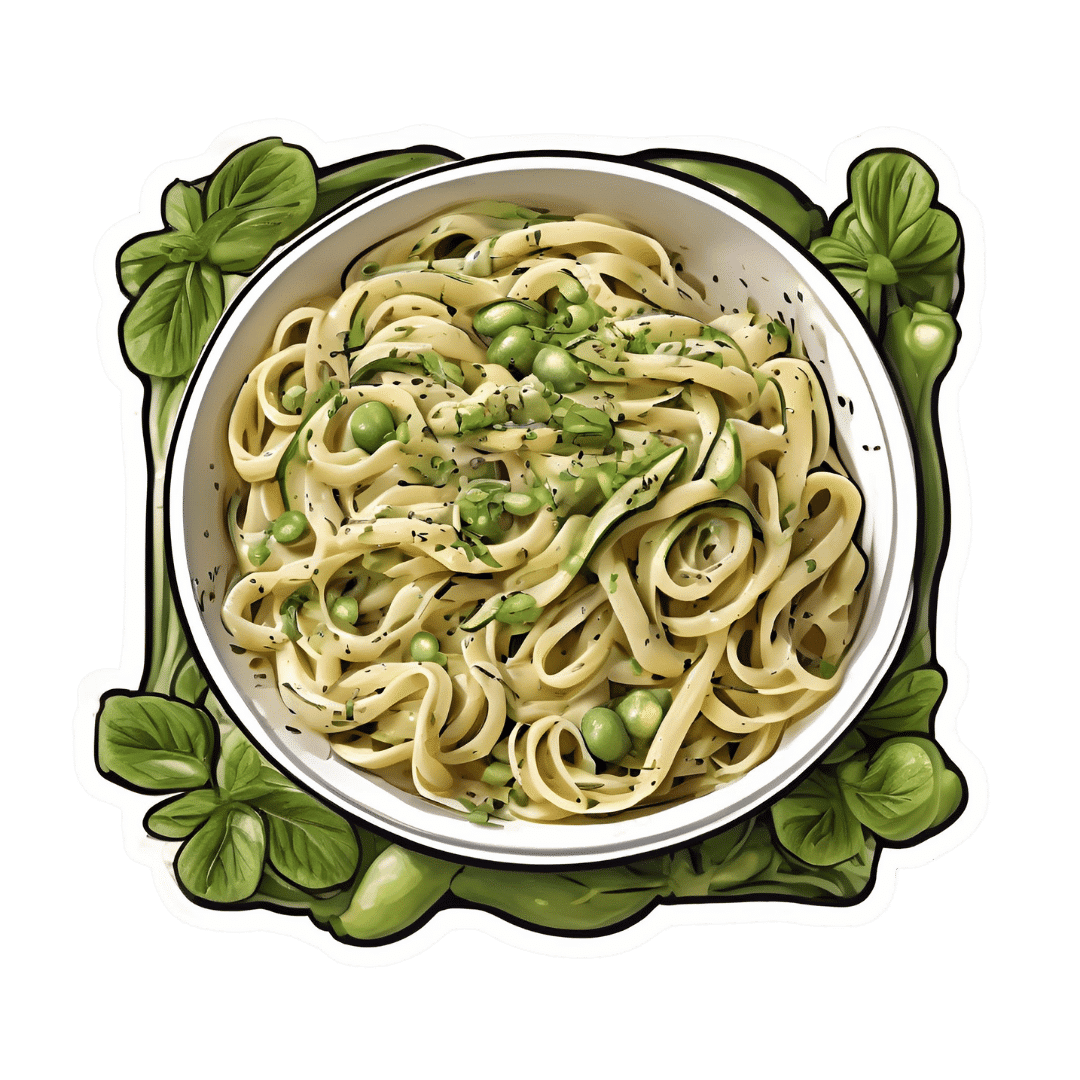
Creamy Zucchini, Edamame, & Asparagus Linguine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protein, fiber, and polyphenols are the dish of the day here:
You will need
- 1½ cups milk (your choice what kind; we recommend soy for its neutral taste, though hazelnut’s nutty flavor would also work in this recipe)
- 6 oz wholegrain linguine (or your pasta of choice)
- 2 zucchini, thinly sliced
- 5 oz edamame beans (frozen is fine)
- 5 oz asparagus tips, cut into 2″ lengths
- ½ bulb garlic, crushed
- 1 tbsp chia seeds
- 1 small handful arugula
- 1 small handful parsley, chopped
- A few mint leaves, chopped
- Juice of ½ lemon
- 2 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan or similar, over a low to medium heat. Add the zucchini and cook for 5 minutes until they start to soften.
2) Add the garlic and continue cooking for 1 minute, stirring gently.
3) Add the milk, bring to the boil, and add the past, chia seeds (the resistant starch from the pasta will help thicken the sauce, as will the chia seeds), and MSG or salt.
4) Reduce the heat, cover, and simmer for 8 minutes.
5) Add the edamame beans and asparagus, and cook for a further 2 minutes, or until the pasta is cooked but still firm to the bite. The sauce should be quite thick now.
6) Stir in the remaining ingredients and serve, adding a garnish if you wish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Share This Post
Related Posts
-
Limitless Expanded Edition – by Jim Kwik
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a little flashier in presentation than we usually go for here, but the content is actually very good. Indeed, we’ve featured Jim Kwik before, with different, but also good content—in that case, physical exercises that strengthen the brain.
This time, Kwik (interspersed with motivational speeches that you may or may not benefit from, but they are there) offers a step-by-step course in improving various metrics of cognitive ability. His methods were produced by trial and error, and now have been refined and enjoyed by man. If it sounds like a sales gimmick, it is a bit, but the good news is that everything you need to benefit is in the book; it’s not about upselling to a course or “advanced” books or whatnot.
The style is enthusiastically conversational, and instructions when given (which is often) are direct and clear.
Bottom line: one of the most critical abilities a brain can have is the ability to improve itself, so whatever level your various cognitive abilities are at right now, if you apply this book, you will almost certainly improve in one or more areas, which will make it worth the price of the book.
Click here to check out Limitless, and find out what you can do!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Celeriac vs Celery – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celeriac to celery, we picked the celeriac.
Why?
Yes, these are essentially the same plant, but there are important nutritional differences:
In terms of macros, celeriac has more than 2x the protein, and slightly more carbs and fiber. Both are very low glycemic index, so the higher protein and fiber makes celeriac the winner in this category.
In the category of vitamins, celeriac has more of vitamins B1, B3, B5, B6, C, E, K, and choline, while celery has more of vitamins A and B9. An easy win for celeriac.
When it comes to minerals, celeriac has more copper, calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while celery is not higher in any minerals. Another obvious win for celeriac.
Adding these sections up makes for a clear overall win for celeriac, but by all means enjoy either or both!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Staying Strong: Tips To Prevent Muscle Loss With Age
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Andrea Furlan, specialist in physical medicine and rehabilitation with 30 years of experience, has advice:
Fighting sarcopenia
Sarcopenia is so common as to be considered “natural”, but “natural” does not mean “obligatory” and it certainly doesn’t mean “healthy”. As for how to fight it?
You may be thinking “let us guess, is it eat protein and do resistance exercises? And yes it is, but that’s only part of it…
Firstly, she recommends remembering why you are doing this, or because understanding is key to compliance (i.e. your perfect diet and exercise program will mean nothing if you don’t actually do it, and you won’t do it enough to make it a habit, let alone keep it up, if the reasons aren’t clear in your mind).
Sarcopenia comes with an increased risk of falls, reduced physical capacity in general, resultant disability, social isolation, and depression. Of course, this is not a one-to-one equation; you will not necessarily become depressed the moment your muscle mass is below a certain percentage, but statistically speaking, the road to ruin is laid out clearly.
Secondly, she recommends being on the lookout for it. If you check your body composition regularly with a gadget, that’s great and laudable; if you don’t, then a) consider getting one (here’s an example product on Amazon), and b) watch out for decreased muscle strength, fatigue, reduced stamina, noticeable body shape changes with muscle loss and (likely) fat gain.
Thirdly, she recommends more than just regular resistance training and good protein intake. Yes, she recommends those things too, but also getting enough water (can’t rebuild the body without it), avoiding a sedentary lifestyle (sitting leads to atrophy of many supporting and stabilizing muscles, you know, the kind of muscles that don’t look flashy but stop you falling down), and getting good sleep—vital for all kinds of body maintenance, and muscle maintenance is no exception (there’s a reason bodybuilders sleep 9–12 hours daily when in a gaining phase; you don’t need to do that, but don’t skimp on your 7–9 hours, yes, really, even you, yes, at any age).
Lastly, she recommends continuing to learn about the topic, as otherwise it’s easy to go off-track.
For more information on all of the above and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Protein: How Much Do We Need, Really?
- Resistance Is Useful! (Especially As We Get Older)
- Resistance Beyond Weights
- HIIT, But Make It HIRT ← this is about high-intensity resistance training (HIRT); confusing the muscles like one confuses the heart in HIIT, which thus yields improved results
- Sleep: Yes, You Really Do Still Need It
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: