New Year, New Health Habits?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of the year, and many of us hope to make this our healthiest year yet—or at least significantly improve it in some particular area that’s important to us! So, what news from the health world?
The rise of GLP-1 agonists continues
GLP-1 agonists have surged in popularity in the past year, and it looks like that trend is set to continue in the new one. The title of the below-linked pop-science article is slightly misleading, it’s not “almost three quarters of UK women”, but rather, “72% of the women using the digital weight loss platform Juniper”, which means the sample is confined to people interested in weight loss. Still, of those interested in weight loss, 72% is a lot, and the sample size was over 1000:
Read in full: New Year, new approach to weight loss: Almost three quarters of UK women are considering using GLP-1s in 2025
Related: 5 ways to naturally boost the “Ozempic Effect” ← these natural methods “hack” the same metabolic pathways as GLP-1 agonists do (it has to do with incretin levels), causing similar results
The lesser of two evils
Smoking is terrible, for everything. Vaping is… Not great, honestly, but as the below-discussed study shows, at the very least it results in much less severe respiratory symptoms than actual smoking. For many, vaping is a halfway-house to actually quitting; for some, it’s just harm reduction, and that too can be worthwhile.
We imagine that probably very few 10almonds readers smoke cigarettes, but we know quite a few use cannabis, which is discussed also:
Read in full: Switching to e-cigarettes may ease respiratory symptoms, offering hope for smokers
Related: Vaping: A Lot Of Hot Air? ← we look at the pros, cons, and popular beliefs that were true a little while ago but now they’re largely not (because of regulatory changes re what’s allowed in vapes)
Sometimes, more is more
The below-linked pop-science article has a potentially confusingly-worded title that makes it sound like increased exercise duration results in decreasing marginal returns (i.e., after a certain point, you’re getting very limited extra benefits), but in fact the study says the opposite.
Rather, increased moderate exercise (so, walking etc) results in a commensurately decreasing weight and a decreasing waistline.
In short: walk more, lose more (pounds and inches). The study examined those who moved their bodies for 150–300 minutes per week:
Read in full: Increased exercise duration linked to decreasing results in weight and waistline
Related: The Doctor Who Wants Us To Exercise Less, & Move More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Make Time – by Jake Knapp and John Zeratzky
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We live in an information-saturated world, and we have done for so long now that it’s easy to forget: we did not evolve for this!
It’s easy to say “unplug”, but the reality is:
We also have to actually function in this fast-paced info-dense world whether we want to or not, and we are expected to be able to handle it.
So… How?
Appropriately enough, authors Knapp and Zeratsky present the answer in a skimmer-friendly fashion, with summaries and bullet points and diagrams and emboldened text forease of speed-reading. Who uses such tricks?!
In short, less living life in “default mode scramble” and more about making an impact in the ways you actually want to, for you.
Share This Post
-
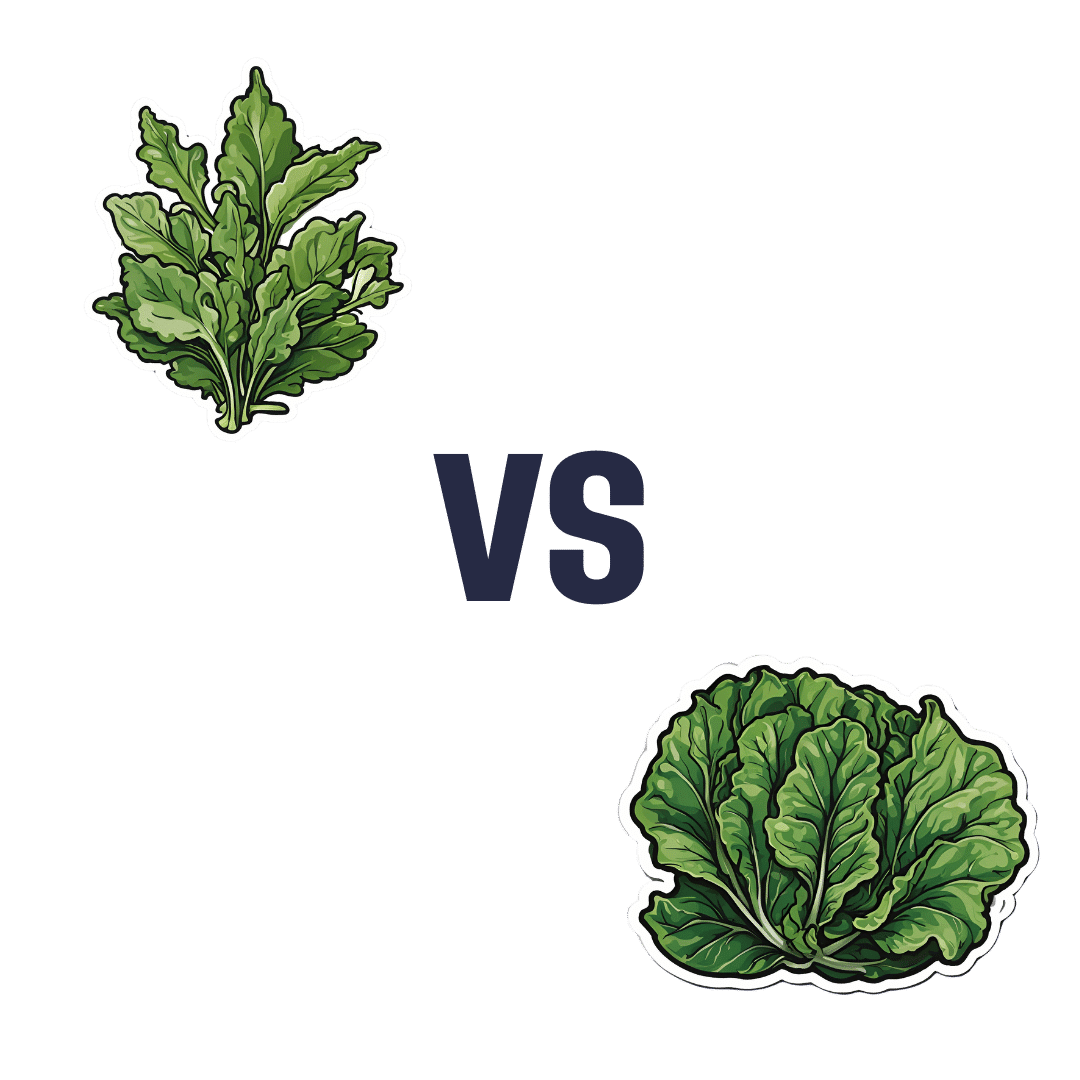
Dandelion Greens vs Collard Greens – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dandelion greens to collard greens, we picked the dandelion greens.
Why?
Collard greens are great—they even beat kale in one of our previous “This or That” articles!—but dandelion greens simply pack more of a nutritional punch:
In terms of macros, dandelions have slightly more carbs (+3g/100g) for the same protein and fiber, and/but the glycemic index is equal (zero), so those carbs aren’t anything to worry about. Nobody is getting metabolic disease by getting their carbs from dandelion leaves. In short, we’re calling it a tie on macros, though it could nominally swing either way if you have an opinion (one way or the other) about the extra 3g of carbs.
In the category of vitamins, things are more exciting: dandelion greens have more of vitamins A, B1, B2, B3, B6, B7, B9, C, E, and K, while collard greens have more vitamin B5. An easy and clear win for dandelions.
Looking at the minerals tells a similar story; dandelion greens have much more calcium, copper, iron, magnesium, phosphorus, potassium, and zinc, while collard greens have slightly more manganese. Another overwhelming win for dandelions.
One more category, polyphenols. We’d be here until next week if we listed all the polyphenols that dandelion greens have, but suffice it to say, dandelion greens have a total of 385.55mg/100g polyphenols, while collard greens have a total of 0.08mg/100g polyphenols. Grabbing a calculator, we see that this means dandelions have more than 4819x the polyphenol content that collard greens do.
So, “eat leafy greens” is great advice, but they are definitely not all created equal!
Let us take this moment to exhort: if you have any space at home where you can grow dandelions, grow them!
Not only are they great for pollinators, but also they beat the collard greens that beat kale. And you can have as much as you want, for free, right there.
Want to learn more?
You might like to read:
Collard Greens vs Kale – Which is Healthier?
Enjoy!
Share This Post
-
Long-Covid Patients Are Frustrated That Federal Research Hasn’t Found New Treatments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Erica Hayes, 40, has not felt healthy since November 2020 when she first fell ill with covid.
Hayes is too sick to work, so she has spent much of the last four years sitting on her beige couch, often curled up under an electric blanket.
“My blood flow now sucks, so my hands and my feet are freezing. Even if I’m sweating, my toes are cold,” said Hayes, who lives in Western Pennsylvania. She misses feeling well enough to play with her 9-year-old son or attend her 17-year-old son’s baseball games.
Along with claiming the lives of 1.2 million Americans, the covid-19 pandemic has been described as a mass disabling event. Hayes is one of millions of Americans who suffer from long covid. Depending on the patient, the condition can rob someone of energy, scramble the autonomic nervous system, or fog their memory, among many other http://symptoms.in/ addition to the brain fog and chronic fatigue, Hayes’ constellation of symptoms includes frequent hives and migraines. Also, her tongue is constantly swollen and dry.
“I’ve had multiple doctors look at it and tell me they don’t know what’s going on,” Hayes said about her tongue.
Estimates of prevalence range considerably, depending on how researchers define long covid in a given study, but the Centers for Disease Control and Prevention puts it at 17 million adults.
Despite long covid’s vast reach, the federal government’s investment in researching the disease — to the tune of $1.15 billion as of December — has so far failed to bring any new treatments to market.
This disappoints and angers the patient community, who say the National Institutes of Health should focus on ways to stop their suffering instead of simply trying to understand why they’re suffering.
“It’s unconscionable that more than four years since this began, we still don’t have one FDA-approved drug,” said Meighan Stone, executive director of the Long COVID Campaign, a patient-led advocacy organization. Stone was among several people with long covid who spoke at a workshop hosted by the NIH in September where patients, clinicians, and researchers discussed their priorities and frustrations around the agency’s approach to long-covid research.
Some doctors and researchers are also critical of the agency’s research initiative, called RECOVER, or Researching COVID to Enhance Recovery. Without clinical trials, physicians specializing in treating long covid must rely on hunches to guide their clinical decisions, said Ziyad Al-Aly, chief of research and development with the VA St Louis Healthcare System.
“What [RECOVER] lacks, really, is clarity of vision and clarity of purpose,” said Al-Aly, saying he agrees that the NIH has had enough time and money to produce more meaningful progress.
Now the NIH is starting to determine how to allocate an additional $662 million of funding for long-covid research, $300 million of which is earmarked for clinical trials. These funds will be allocated over the next four http://years.at/ the end of October, RECOVER issued a request for clinical trial ideas that look at potential therapies, including medications, saying its goal is “to work rapidly, collaboratively, and transparently to advance treatments for Long COVID.”
This turn suggests the NIH has begun to respond to patients. This has stirred cautious optimism among those who say that the agency’s approach to long covid has lacked urgency in the search for effective treatments.Stone calls this $300 million a down payment. She warns it’s going to take a lot more money to help people like Hayes regain some degree of health.“There really is a burden to make up this lost time now,” Stone said.
The NIH told KFF Health News and NPR via email that it recognizes the urgency in finding treatments. But to do that, there needs to be an understanding of the biological mechanisms that are making people sick, which is difficult to do with post-infectious conditions.
That’s why it has funded research into how long covid affects lung function, or trying to understand why only some people are afflicted with the condition.
Good Science Takes Time
In December 2020, Congress appropriated $1.15 billion for the NIH to launch RECOVER, raising hopes in the long-covid patient community.
Then-NIH Director Francis Collins explained that RECOVER’s goal was to better understand long covid as a disease and that clinical trials of potential treatments would come later.
According to RECOVER’s website, it has funded eight clinical trials to test the safety and effectiveness of an experimental treatment or intervention. Just one of those trials has published results.
On the other hand, RECOVER has supported more than 200 observational studies, such as research on how long covid affects pulmonary function and on which symptoms are most common. And the initiative has funded more than 40 pathobiology studies, which focus on the basic cellular and molecular mechanisms of long covid.
RECOVER’s website says this research has led to crucial insights on the risk factors for developing long covid and on understanding how the disease interacts with preexisting conditions.
It notes that observational studies are important in helping scientists to design and launch evidence-based clinical trials.
Good science takes time, said Leora Horwitz, the co-principal investigator for the RECOVER-Adult Observational Cohort at New York University. And long covid is an “exceedingly complicated” illness that appears to affect nearly every organ system, she said.
This makes it more difficult to study than many other diseases. Because long covid harms the body in so many ways, with widely variable symptoms, it’s harder to identify precise targets for treatment.
“I also will remind you that we’re only three, four years into this pandemic for most people,” Horwitz said. “We’ve been spending much more money than this, yearly, for 30, 40 years on other conditions.”
NYU received nearly $470 million of RECOVER funds in 2021, which the institution is using to spearhead the collection of data and biospecimens from up to 40,000 patients. Horwitz said nearly 30,000 are enrolled so far.
This vast repository, Horwitz said, supports ongoing observational research, allowing scientists to understand what is happening biologically to people who don’t recover after an initial infection — and that will help determine which clinical trials for treatments are worth undertaking.
“Simply trying treatments because they are available without any evidence about whether or why they may be effective reduces the likelihood of successful trials and may put patients at risk of harm,” she said.
Delayed Hopes or Incremental Progress?
The NIH told KFF Health News and NPR that patients and caregivers have been central to RECOVER from the beginning, “playing critical roles in designing studies and clinical trials, responding to surveys, serving on governance and publication groups, and guiding the initiative.”But the consensus from patient advocacy groups is that RECOVER should have done more to prioritize clinical trials from the outset. Patients also say RECOVER leadership ignored their priorities and experiences when determining which studies to fund.
RECOVER has scored some gains, said JD Davids, co-director of Long COVID Justice. This includes findings on differences in long covid between adults and kids.But Davids said the NIH shouldn’t have named the initiative “RECOVER,” since it wasn’t designed as a streamlined effort to develop treatments.
“The name’s a little cruel and misleading,” he said.
RECOVER’s initial allocation of $1.15 billion probably wasn’t enough to develop a new medication to treat long covid, said Ezekiel J. Emanuel, co-director of the University of Pennsylvania’s Healthcare Transformation Institute.
But, he said, the results of preliminary clinical trials could have spurred pharmaceutical companies to fund more studies on drug development and test how existing drugs influence a patient’s immune response.
Emanuel is one of the authors of a March 2022 covid roadmap report. He notes that RECOVER’s lack of focus on new treatments was a problem. “Only 15% of the budget is for clinical studies. That is a failure in itself — a failure of having the right priorities,” he told KFF Health News and NPR via email.
And though the NYU biobank has been impactful, Emanuel said there needs to be more focus on how existing drugs influence immune response.
He said some clinical trials that RECOVER has funded are “ridiculous,” because they’ve focused on symptom amelioration, for example to study the benefits of over-the-counter medication to improve sleep. Other studies looked at non-pharmacological interventions, such as exercise and “brain training” to help with cognitive fog.
People with long covid say this type of clinical research contributes to what many describe as the “gaslighting” they experience from doctors, who sometimes blame a patient’s symptoms on anxiety or depression, rather than acknowledging long covid as a real illness with a physiological basis.
“I’m just disgusted,” said long-covid patient Hayes. “You wouldn’t tell somebody with diabetes to breathe through it.”
Chimére L. Sweeney, director and founder of the Black Long Covid Experience, said she’s even taken breaks from seeking treatment after getting fed up with being told that her symptoms were due to her diet or mental health.
“You’re at the whim of somebody who may not even understand the spectrum of long covid,” Sweeney said.
Insurance Battles Over Experimental Treatments
Since there are still no long-covid treatments approved by the Food and Drug Administration, anything a physician prescribes is classified as either experimental — for unproven treatments — or an off-label use of a drug approved for other conditions. This means patients can struggle to get insurance to cover prescriptions.
Michael Brode, medical director for UT Health Austin’s Post-COVID-19 Program — said he writes many appeal letters. And some people pay for their own treatment.
For example, intravenous immunoglobulin therapy, low-dose naltrexone, and hyperbaric oxygen therapy are all promising treatments, he said.
For hyperbaric oxygen, two small, randomized controlled studies show improvements for the chronic fatigue and brain fog that often plague long-covid patients. The theory is that higher oxygen concentration and increased air pressure can help heal tissues that were damaged during a covid infection.
However, the out-of-pocket cost for a series of sessions in a hyperbaric chamber can run as much as $8,000, Brode said.
“Am I going to look a patient in the eye and say, ‘You need to spend that money for an unproven treatment’?” he said. “I don’t want to hype up a treatment that is still experimental. But I also don’t want to hide it.”
There’s a host of pharmaceuticals that have promising off-label uses for long covid, said microbiologist Amy Proal, president and chief scientific officer at the Massachusetts-based PolyBio Research Foundation. For instance, she’s collaborating on a clinical study that repurposes two HIV drugs to treat long covid.
Proal said research on treatments can move forward based on what’s already understood about the disease. For instance, she said that scientists have evidence — partly due to RECOVER research — that some patients continue to harbor small amounts of viral material after a covid infection. She has not received RECOVER funds but is researching antivirals.
But to vet a range of possible treatments for the millions suffering now — and to develop new drugs specifically targeting long covid — clinical trials are needed. And that requires money.
Hayes said she would definitely volunteer for an experimental drug trial. For now, though, “in order to not be absolutely miserable,” she said she focuses on what she can do, like having dinner with her http://family.at/ the same time, Hayes doesn’t want to spend the rest of her life on a beige couch.
RECOVER’s deadline to submit research proposals for potential long-covid treatments is Feb. 1.
This article is from a partnership that includes NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Goji Berries vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing goji berries to blueberries, we picked the goji berries.
Why?
As you might have guessed, both are very good options:
- Both have plenty of vitamins and minerals, and/but goji berries have more. How much more? It varies, but for example about 5x more vitamin C, about 25x more iron, about 30x more calcium, about 50x more vitamin A.
- Blueberries beat goji berries with some vitamins (B, E, K), but only in quite small amounts.
- Both are great sources of antioxidants, and/but goji berries have 2–4 times the antioxidants that blueberries do.
- Goji berries do have more sugar, but since they have about 4x more sugar and 5x more fiber, we’re still calling this a win for goji berries on the glycemic index front (and indeed, the GI of goji berries is lower).
In short: blueberries are great, but goji berries beat them in most metrics.
Want to read more?
Check out our previous main features, detailing some of the science, and also where to get them:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How extreme heat can affect you—and how you can protect yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Because of climate change, last summer was the hottest in the Northern Hemisphere in 2,000 years—and this summer is expected to be even hotter. The record may continue to be broken: Extreme heat is expected to become even more frequent.
The scorching heat has led to an increase in heat-related deaths in the United States, according to the Department of Health and Human Services, with approximately 2,300 deaths in the summer of 2023. Extreme heat, defined as a period of two to three days with high heat and humidity with temperatures above 90 degrees Fahrenheit, can have serious health consequences, including symptoms like headache, dizziness, loss of consciousness, nausea, and confusion.
As we face more extreme heat, you may be wondering how you can protect yourself and your loved ones. Read on to learn about heat-related illness, who’s most at risk, and more.
What happens when our bodies are exposed to extreme heat?
As our body temperature rises, our bodies attempt to cool down by opening up more blood vessels near the skin to begin sweating. The evaporation of our sweat regulates our body temperature, but it also leads to losing fluids and minerals.
When it’s too humid, sweating alone doesn’t do the trick. The heart must work harder to bring blood around the body. It starts beating faster, which can cause light-headedness, nausea, and headache.
This process can affect our health in different ways, including increasing our risk of hospitalization for heart disease, worsening asthma, and injuring kidneys due to dehydration. It can also result in heat-related illness. Below are some effects of heat on our bodies:
- Heat cramps: Occur when a person loses salt through sweating, which causes painful cramps. Symptoms begin as painful spasms after heavy sweating, usually in the legs or the stomach. Heat cramps can lead to heat exhaustion or heat stroke.
- Heat exhaustion: This occurs when the body loses an excessive amount of water and salt, usually during intense physical activity. Symptoms include irritability, heavy sweating, and weakness, including muscle cramps. Heat exhaustion can lead to heat stroke.
- Heat stroke: This is the most severe heat-related illness. It happens when the body can’t cool down and reaches a temperature of 106 Fahrenheit or higher within 10 to 15 minutes. If the person doesn’t receive emergency treatment, it can cause permanent disability or death. Symptoms include confusion, loss of consciousness, and seizures.
What should I do if someone experiences a heat-related illness?
If you or someone you’re with begins to show signs of heat illness, the Centers for Disease Control and Prevention recommends the following:
- Heat cramps: Stop all physical activity, drink water or a sports drink, move to a cool place, and wait for cramps to go away before resuming activity. If the cramps last more than an hour, you’re on a low-sodium diet, or you have heart problems, get medical help.
- Heat exhaustion: Move the person to a cool place, loosen their clothes, use a cool bath or cloths to try to lower their body temperature, and give them a sip of water. If the person throws up, or if their symptoms last longer than an hour or worsen, get medical help.
- Heat stroke: Call 911 immediately. Then, move the person to a cooler place, use cool cloths or a cool bath to help lower their temperature, and don’t give them anything to drink.
Read more about heat-related illness and what to do in each case.
Who’s more vulnerable to extreme heat?
While everyone can be affected by extreme heat, some people are more at risk, including people of color.
A 2023 KFF report outlined that because of historical residential segregation in the U.S. (known as “redlining”), people of color are more likely to live in areas that experience higher temperatures from rooftops, asphalt, and sidewalks that retain the sun’s heat (known as the “urban heat island effect”). Additionally, communities of color are more likely to live in areas with fewer trees, which act as a canopy and provide shade, making the heat worse and more direct.
Children under 5, adults 65 or over, and pregnant people are also more vulnerable to extreme heat. If you have a chronic health condition like diabetes, heart problems, or a mental health condition, you’re also at higher risk. (Some psychiatric medications, like antidepressants, can also make people more susceptible to heat).
Lastly, anyone exposed to the sun and extreme heat for long periods is also at higher risk. This includes athletes, people who work outdoors, and unhoused people.
What can I do to prevent heat-related illness during a heat wave?
During a heat wave, follow these tips to stay cool and protect yourself from heat-related illness:
- Never leave your pets or children inside a car.
- Wear loose, light-colored clothing (dark colors absorb more heat).
- Find shade if you’re outside.
- If you don’t have air conditioning in your home, go to a place where you can cool down, such as a local library, community center, local pool or splash pad, or mall. Check to see if your city has designated cooling centers. (Cities like New York have a list of places.)
- Wear a hat.
- Drink (non-alcoholic) fluids often to stay hydrated—and if you have pets, give them water frequently as well.
- Check on your family members or older neighbors who may be more sensitive to extreme heat.
- Avoid using your stove or oven too often or during the hottest parts of the day.
- Cover your windows with shades to keep the heat out.
What are some resources to prevent heat-related illness?
If you need financial assistance to cool down your home, such as to purchase an air conditioner, apply to the federal government’s Low Income Home Energy Assistance Program.
Before you head outside during a heat wave, use the CDC’s HeatRisk tool: Enter your zip code to find the current heat risk in your area and get tips on what to do to stay safe with each risk level.
During a heat wave, also look for a cooling center in your state using the National Center for Healthy Housing’s list.
Check out the National Weather Service’s for more tips and resources.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Doctors From 15 Specialties Tell The Worst Common Mistakes People Make
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whatever your professional background, you probably know many things about it that are very obvious to you, but that most people don’t know. So it is for doctors too; here are the things that doctors from 15 specialties would never do, and thus advise people against doing:
Better safe than sorry
We’ll leap straight into it:
- General Surgery: avoid rushing into musculoskeletal or spinal surgery unless absolutely necessary; conservative treatments like physical therapy are often effective.
- Interventional Gastroenterology: avoid long-term, around-the-clock use of anti-inflammatory pain medications (e.g. Ibuprofen and friends) to prevent stomach ulcers.
- Podiatry: never place feet on the car dashboard due to the risk of severe injuries from airbag deployment.
- Rheumatology: avoid daily use of high heels to prevent joint and foot deformities, bunions, and pain.
- Otorhinolaryngology: never smoke, as it can lead to severe consequences like laryngectomy and other life-altering conditions.
- Pediatrics: avoid dangerous activities for children, such as swimming alone, eating choking hazards, biking or skiing without a helmet, or consuming raw meat/fish/dairy. Also, be cautious with firearms in homes.
- Orthopedic Surgery: avoid riding motorcycles and handling fireworks due to high risks of accidents.
- Emergency Medicine: never drink and drive or ride ATVs. Always use eye protection during activities like woodworking.
- Ophthalmology: always wear safety glasses during activities like grinding metal or woodworking. Sunglasses are essential to prevent UV damage even on cloudy days.
- Urology: avoid shaving pubic hair if diabetic or immunocompromised to prevent severe infections like Fournier’s gangrene.
- Gastroenterology: do not use gut health supplements as they lack proven efficacy and are often a waste of money*
- Plastic Surgery: avoid contour threads (barbed sutures for facial rejuvenation) and butt implants due to risks like infection, complications, and poor outcomes.
- Psychiatry: never take recreational drugs from unknown sources to avoid accidental overdoses, especially from substances laced with fentanyl. Carry Narcan for emergencies.
- Dermatology: use sunscreen daily to prevent skin cancer, aging, pigmentation issues, and texture problems caused by UV exposure.
- Cardiology: avoid the carnivore diet as it increases heart disease risks due to its negligible fiber content and high saturated fat intake.
*We had an article about this a while back; part of the problem is that taking probiotics without prebiotics can mean your new bacteria just die in about 20 minutes, which is their approximate lifespan in which to multiply or else die out. Similar problems arise if taking them with sugar that feeds their competitors instead. See: Stop Sabotaging Your Gut!
For more on each of these, in the words of the respective doctors, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: