Moore’s Clinically Oriented Anatomy – by Dr. Anne Argur & Dr. Arthur Dalley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Imagine, if you will, Grey’s Anatomy but beautifully illustrated in color and formatted in a way that’s easy to read—both in terms of layout and searchability, and also in terms of how this book presents anatomy described in a practical, functional context, with summary boxes for each area, so that the primary concepts don’t get lost in the very many details.
(In contrast, if you have a copy of the famous Grey’s Anatomy, you’ll know it’s full of many pages of nothing but tiny dense text, a large amount of which is Latin, with occasional etchings by way of illustration)
Another way in which this does a lot better than the aforementioned seminal work is that it also describes and discusses very many common variations and abnormalities, both congenital and acquired, so that it’s not just a text of “what a theoretical person looks like inside”, but rather also reflects the diverse reality of the human form (we weren’t made identically in a production line, and so we can vary quite a bit).
The book is, of course, intended for students and practitioners of medicine and related fields, so what good is it to the lay person? Well, if you ask the average person where the gallbladder is and why we have one, they will gesture in the general direction of the abdomen, and sort of shrug sheepishly. You don’t have to be that person 🙂
Bottom line: if you’d like to know your acetabulum from your zygomatic arch, this is the best anatomy book this reviewer has yet seen.
Click here to check out Moore’s Clinically Oriented Anatomy, and prepare to be amazed!
PS: this one is expensive, but consider it a fair investment in your personal education, if you’re serious about it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Reflexology: What The Science Says
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Does Reflexology Work, Really?
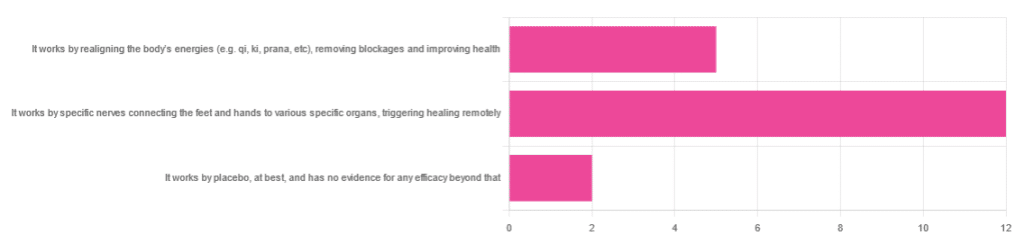
In Wednesday’s newsletter, we asked you for your opinion of reflexology, and got the above-depicted, below-described set of responses:
- About 63% said “It works by specific nerves connecting the feet and hands to various specific organs, triggering healing remotely”
- About 26% said “It works by realigning the body’s energies (e.g. qi, ki, prana, etc), removing blockages and improving health“
- About 11% said “It works by placebo, at best, and has no evidence for any efficacy beyond that”
So, what does the science say?
It works by realigning the body’s energies (e.g. qi, ki, prana, etc), removing blockages and improving health: True or False?
False, or since we can’t prove a negative: there is no reliable scientific evidence for this.
Further, there is no reliable scientific evidence for the existence of qi, ki, prana, soma, mana, or whatever we want to call it.
To save doubling up, we did discuss this in some more detail, exploring the notion of qi as bioelectrical energy, including a look at some unreliable clinical evidence for it (a study that used shoddy methodology, but it’s important to understand what they did wrong, to watch out for such), when we looked at [the legitimately very healthful practice of] qigong, a couple of weeks ago:
Qigong: A Breath Of Fresh Air?
As for reflexology specifically: in terms of blockages of qi causing disease (and thus being a putative therapeutic mechanism of action for attenuating disease), it’s an interesting hypothesis but in terms of scientific merit, it was pre-emptively supplanted by germ theory and other similarly observable-and-measurable phenomena.
We say “pre-emptively”, because despite orientalist marketing, unless we want to count some ancient pictures of people getting a foot massage and say it is reflexology, there is no record of reflexology being a thing before 1913 (and that was in the US, by a laryngologist working with a spiritualist to produce a book that they published in 1917).
It works by specific nerves connecting the feet and hands to various specific organs, triggering healing remotely: True or False?
False, or since we can’t prove a negative: there is no reliable scientific evidence for this.
A very large independent review of available scientific literature found the current medical consensus on reflexology is that:
- Reflexology is effective for: anxiety (but short lasting), edema, mild insomnia, quality of sleep, and relieving pain (short term: 2–3 hours)
- Reflexology is not effective for: inflammatory bowel disease, fertility treatment, neuropathy and polyneuropathy, acute low back pain, sub acute low back pain, chronic low back pain, radicular pain syndromes (including sciatica), post-operative low back pain, spinal stenosis, spinal fractures, sacroiliitis, spondylolisthesis, complex regional pain syndrome, trigger points / myofascial pain, chronic persistent pain, chronic low back pain, depression, work related injuries of the hip and pelvis
Source: Reflexology – a scientific literary review compilation
(the above is a fascinating read, by the way, and its 50 pages go into a lot more detail than we have room to here)
Now, those items that they found it effective for, looks suspiciously like a short list of things that placebo is often good for, and/or any relaxing activity.
Another review was not so generous:
❝The best evidence available to date does not demonstrate convincingly that reflexology is an effective treatment for any medical condition❞
~ Dr. Edzard Ernst (MD, PhD, FMedSci)
Source: Is reflexology an effective intervention? A systematic review of randomised controlled trials
In short, from the available scientific literature, we can surmise:
- Some researchers have found it to have some usefulness against chiefly psychosomatic conditions
- Other researchers have found the evidence for even that much to be uncompelling
It works by placebo, at best, and has no evidence for any efficacy beyond that: True or False?
Mostly True; of course reflexology runs into similar problems as acupuncture when it comes to testing against placebo:
How Does One Test Acupuncture Against Placebo Anyway?
…but not quite as bad, since it is easier to give a random foot massage while pretending it is a clinical treatment, than to fake putting needles into key locations.
However, as the paper we cited just above (in answer to the previous True/False question) shows, reflexology does not appear to meaningfully outperform placebo—which points to the possibility that it does work by placebo, and is just a placebo treatment on the high end of placebo (because the placebo effect is real, does work, isn’t “nothing”, and some placebos work better than others).
For more on the fascinating science and useful (applicable in daily life!) practicalities of how placebo does work, check out:
How To Leverage Placebo Effect For Yourself
Take care!
Share This Post
-
Exercise with Type 1 Diabetes – by Ginger Vieira
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you or a loved one has Type 1 Diabetes, you’ll know that exercise can be especially frustrating…
- If you don’t do it, you risk weight gain and eventual insulin resistance.
- If you do it, you risk dangerous hypos, or perhaps hypers if you took off your pump or skipped a bolus.
Unfortunately, the popular medical advice is “well, just do your best”.
Ginger Vieira is Type 1 Diabetic, and writes with 20+ experience of managing her diabetes while being a keen exerciser. As T1D folks out there will also know, comorbidities are very common; in her case, fibromyalgia was the biggest additional blow to her ability to exercise, along with an underactive thyroid. So when it comes to dealing with the practical nuts and bolts of things, she (while herself observing she’s not a doctor, let alone your doctor) has a lot more practical knowledge than an endocrinologist (without diabetes) behind a desk.
Speaking of nuts and bolts, this book isn’t a pep talk.
It has a bit of that in, but most of it is really practical information, e.g: using fasted exercise (4 hours from last meal+bolus) to prevent hypos, counterintuitive as that may seem—the key is that timing a workout for when you have the least amount of fast-acting insulin in your body means your body can’t easily use your blood sugars for energy, and draws from your fat reserves instead… Win/Win!
That’s just one quick tip because this is a 1-minute review, but Vieira gives:
- whole chapters, with example datasets (real numbers)
- tech-specific advice, e.g. pump, injection, etc
- insulin-specific advice, e.g. fast vs slow, and adjustments to each in the context of exercise
- timing advice re meal/bolus/exercise for different insulins and techs
- blood-sugar management advice for different exercise types (aerobic/anaerobic, sprint/endurance, etc)
…and lots more that we don’t have room to mention here
Basically… If you or a loved one has T1D, we really recommend this book!
Order a copy of “Exercise with Type 1 Diabetes” from Amazon today!
Share This Post
-
Only walking for exercise? Here’s how to get the most out of it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re living longer than in previous generations, with one in eight elderly Australians now aged over 85. But the current gap between life expectancy (“lifespan”) and health-adjusted life expectancy (“healthspan”) is about ten years. This means many of us live with significant health problems in our later years.
To increase our healthspan, we need planned, structured and regular physical activity (or exercise). The World Health Organization recommends 150–300 minutes of moderate-intensity exercise – such as brisk walking, cycling and swimming – per week and muscle strengthening twice a week.
Yet few of us meet these recommendations. Only 10% meet the strength-training recommendations. Lack of time is one of the most common reasons.
Walking is cost-effective, doesn’t require any special equipment or training, and can be done with small pockets of time. Our preliminary research, published this week, shows there are ways to incorporate strength-training components into walking to improve your muscle strength and balance.
Why walking isn’t usually enough
Regular walking does not appear to work as muscle-strengthening exercise.
In contrast, exercises consisting of “eccentric” or muscle-lengthening contractions improve muscle strength, prevent muscle wasting and improve other functions such as balance and flexibility.
Typical eccentric contractions are seen, for example, when we sit on a chair slowly. The front thigh muscles lengthen with force generation.
When you sit down slowly on a chair, the front thigh muscles lengthen.
buritora/ShutterstockOur research
Our previous research found body-weight-based eccentric exercise training, such as sitting down on a chair slowly, improved lower limb muscle strength and balance in healthy older adults.
We also showed walking down stairs, with the front thigh muscles undergoing eccentric contractions, increased leg muscle strength and balance in older women more than walking up stairs. When climbing stairs, the front thigh muscles undergo “concentric” contractions, with the muscles shortening.
It can be difficult to find stairs or slopes suitable for eccentric exercises. But if they could be incorporated into daily walking, lower limb muscle strength and balance function could be improved.
This is where the idea of “eccentric walking” comes into play. This means inserting lunges in conventional walking, in addition to downstairs and downhill walking.
In our new research, published in the European Journal of Applied Physiology, we investigated the effects of eccentric walking on lower limb muscle strength and balance in 11 regular walkers aged 54 to 88 years.
The intervention period was 12 weeks. It consisted of four weeks of normal walking followed by eight weeks of eccentric walking.
The number of eccentric steps in the eccentric walking period gradually increased over eight weeks from 100 to 1,000 steps (including lunges, downhill and downstairs steps). Participants took a total of 3,900 eccentric steps over the eight-week eccentric walking period while the total number of steps was the same as the previous four weeks.
We measured the thickness of the participants’ front thigh muscles, muscle strength in their knee, their balance and endurance, including how many times they could go from a sitting position to standing in 30 seconds without using their arms. We took these measurements before the study started, at four weeks, after the conventional walking period, and at four and eight weeks into the eccentric walking period.
We also tested their cognitive function using a digit symbol-substitution test at the same time points of other tests. And we asked participants to complete a questionnaire relating to their activities of daily living, such as dressing and moving around at home.
Finally, we tested participants’ blood sugar, cholesterol levels and complement component 1q (C1q) concentrations, a potential marker of sarcopenia (muscle wasting with ageing).
Regular walking won’t contract your muscles in the same way as eccentric walking.
alexei_tm/ShutterstockWhat did we find?
We found no significant changes in any of the outcomes in the first four weeks when participants walked conventionally.
From week four to 12, we found significant improvements in muscle strength (19%), chair-stand ability (24%), balance (45%) and a cognitive function test (21%).
Serum C1q concentration decreased by 10% after the eccentric walking intervention, indicating participants’ muscles were effectively stimulated.
The sample size of the study was small, so we need larger and more comprehensive studies to verify our findings and investigate whether eccentric walking is effective for sedentary people, older people, how the different types of eccentric exercise compare and the potential cognitive and mental health benefits.
But, in the meantime, “eccentric walking” appears to be a beneficial exercise that will extend your healthspan. It may look a bit eccentric if we insert lunges while walking on the street, but the more people do it and benefit from it, the less eccentric it will become.
Ken Nosaka, Professor of Exercise and Sports Science, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Take This Two-Minute Executive Dysfunction Test
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Roll For Initiative
Some of us struggle with executive dysfunction a lot; others, a little.
What Is Executive Dysfunction?
• Executive function is a broad group of mental skills that enable people to complete tasks and interact with others.
• Executive dysfunction can impair a person’s ability to organize and manage behavior
• Executive dysfunction is not a specific stand-alone diagnosis or condition.
• Instead, conditions such as depression and ADHD (amongst others) can affect a person’s executive function.
Take This Two-Minute Executive Dysfunction Test
How did you score? (8/16 here!)
Did you do it? (it honestly is really two minutes and is quite informative)
If not, here’s your cue to go back up and do it
For almost all of us, we sometimes find ourselves torn between several competing tasks, and end up doing… none of them.
For such times, compile yourself a “productivity buffet”, print it, and pin it above your desk or similar space.
What’s a productivity buffet?
It’s a numbered list of 6, 8, 10, 12 or 20 common tasks that pretty much always need doing (to at least some extent!). Doesn’t matter how important they are, just that they are frequently recurring tasks. For example:
- Tidy desk (including that drawer!)
- Reply to emails/messages
- Drink water
- Collect stray one-off to-dos into a list
- Stretch (or at least correct your posture!)
- Extend that Duolingo streak
- Read one chapter of a book
- Etc
Why 6, 8, 10, 12, or 20?
Because those are common denominations of polyhedral dice that are very cheap to buy!
Keep the relevant die to hand (perhaps in your pocket or on your desk), and when you know you should be doing something but can’t decide what exactly, roll the die and do the item corresponding to the number you roll.
And if you find yourself thinking “damn, I got 12, I wanted 7!” then go ahead and do item 7—the dice aren’t the boss of you, they’re just there to break the ice between you and your to-do list!
The Housekeeper In Your Pocket?
If you found the tidying tips (up top) helpful, but don’t like cleaning schedules because you just can’t stick to them, this one’s for you.
It’s easy to slip into just doing the same few easy tasks while neglecting others for far too long.
The answer? Outsource!
Not “get a cleaner” (though if you want to and can, great, go for it, this one won’t be for you after all), but rather, try this nifty little app that helps you keep on top of daily cleaning—which we all know is better than binge-cleaning every few months.
Sweepy keeps track of:
- What jobs there are that might need doing in each room (or type of room) in the house
- How often those jobs generally need doing
- How much of your energy (a finite resource, which it also takes into account!) those jobs will take
- How much energy you are prepared to spend per day (you can “lighter/heavier” days, or even “off-days”, too)
…and then it populates a small daily task list according to what needs cleaning and how much energy it’ll take.
For example, today Sweepy gives me (your trusty writer, hi! ) the tasks:
- Bathroom: clean sink (every 3 days, 1pt of energy)
- Dining room: clean and tidy table (every day, 1pt of energy)
- Bedroom: vacuum floor (every 7 days, 2pts of energy)
- Kitchen: clean coffee machine (every 30 days, 2pts of energy)
And that’s my 6pts of energy I’ve told Sweepy I’m happy to spend per day cleaning. There are “3 pts” tasks too—cleaning the oven, for example—but none came up today.
Importantly: it does not bother me about any other tasks today (even if something’s overdue), and I don’t have to worry my pretty head about it.
I don’t have to feel guilty for not doing other cleaning tasks; if they need doing, Sweepy will tell me tomorrow, and it will make sure I don’t get behind or leave anything neglected for too long.
Check it out (available for both iOS and Android)
PS: to premium or not to premium? We think the premium is worth it (unlocks some extra customization features) but the free version is sufficient to get your house in order, so don’t be afraid to give it a try first.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Celery vs Chard – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing celery to chard, we picked the chard.
Why?
In terms of macros, chard has more fiber, carbs, and protein, making it the more nutrient-dense option and thus the winner of the macros category.
In the category of vitamins, celery has more of vitamins B5 and B9, while chard has more of vitamins A, B1, B2, B3, B6, C, E, K, and choline—another win for chard.
When it comes to minerals, celery is not higher in any minerals, while chard has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. One more very clear win for chard!
Looking at polyphenols, celery has very little to boast, about 3mg/100g furanocoumarins and nothing else, while chard has an impressive array of polyphenols, with 9mg/100g kaempferol and 7.5mg/100g quercetin atop the list of 12 polyphenols. Yet another win for chard.
Adding up the sections is not difficult arithmetic today: chard sweeps every category. But by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Dr. Greger’s Daily Dozen ← the “dozen” in question includes getting a good amount of of leafy greens per day
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Skincare – by Caroline Hirons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our skin is our largest organ, and it affects (and is affected by) most of what it contains. In other words, us.
So how do we look after this organ? Caroline Hirons lays it bare for us, in this very clear (and well-illustrated with many photos) book that gives a ground-upwards explanation of:
- Our skin’s layers and features and what they do
- The many ways our skin can be different from others
- What lifestyle factors to worry about (or not)
- What exactly the many kinds of skincare products do
- How to understand which ones are actually for our skin
- How to craft the ideal skincare routine for any individual
- What should go into a personalized skincare kit
Because, as it turns out, shockingly we can’t trust advertising. Not only is it advertising, but also, they don’t know us. What will be perfect for one person’s skin may ruin another’s, and labels can be very misleading.
A strength of this book is how Hirons demystifies all that, so we can ignore the claims and just know what a product will actually do, from its ingredients.
She also covers the changes that occur in various life processes, including puberty, pregnancy, menopause, and just plain aging. In other words, what to do when what’s been working suddenly doesn’t anymore.
Bottom line: this is a great book for anyone (though: especially those of us with female hormones) who wants to understand the skin you’re in and how to keep it well-nourished and glowingly healthy.
Click here to check out “Skincare” and take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: