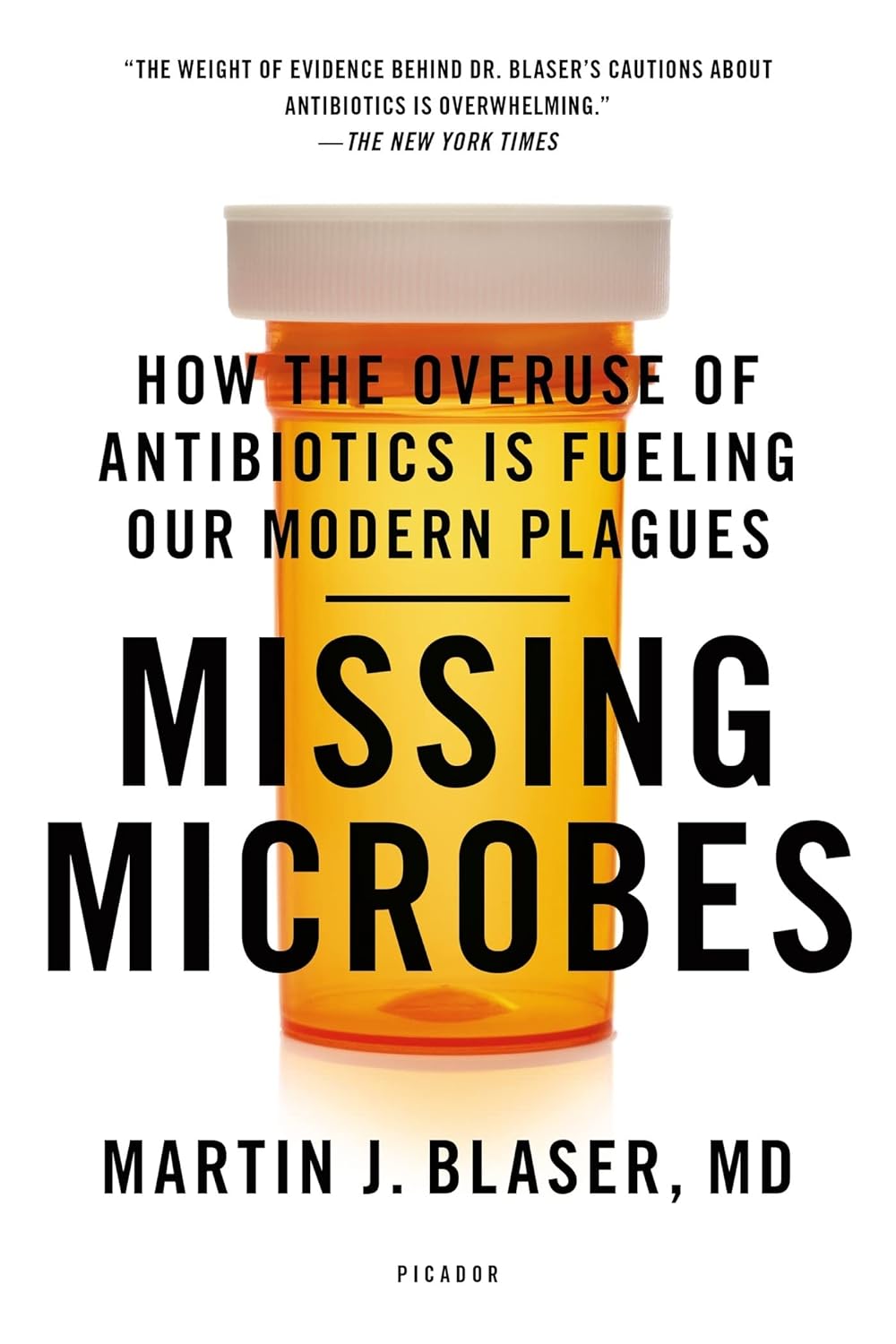
Missing Microbes – by Dr. Martin Blaser
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You probably know that antibiotic resistance is a problem, but you might not realize just what a many-headed beast antibiotic overuse is.
From growing antibiotic superbugs, to killing the friendly bacteria that normally keep pathogens down to harmless numbers (resulting in death of the host, as the pathogens multiply unopposed), to multiple levels of dangers in antibiotic overuse in the farming of animals, this book is scary enough that you might want to save it for Halloween.
But, Dr. Blaser does not argue against antibiotic use when it’s necessary; many people are alive because of antibiotics—he himself recovered from typhoid because of such.
The style of the book is narrative, but information-dense. It does not succumb to undue sensationalization, but it’s also far from being a dry textbook.
Bottom line: if you’d like to understand the real problems caused by antibiotics, and how we can combat that beyond merely “try not to take them unnecessarily”, this book is very worthy reading.
Click here to check out Missing Microbes, and learn more about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
No More Aches/Tripping When Walking: Strengthen This Oft-Neglected Muscle
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aches and pains while walking (in the feet, shins, and/or knees), as well as fatigue, are actually mostly about the oft-neglected tibialis anterior muscle.
Fortunately, it’s quite easy to strengthen if you know how:
All about the tib
The tibialis anterior is located at the front of the shin. It lifts the toes when walking, preventing trips and stumbles. Weakness in this muscle can cause fatigue as other muscles compensate, tripping as feet catch the floor, and/or general instability while walking.
Happily, there is an easy exercise to do that gives results quite quickly:
Steps:
- Stand with back and shoulders against a wall, feet 12 inches away.
- Slightly bend knees and keep posture relaxed.
- Lift toes off the ground, hold for a few seconds, then lower.
- Repeat for 10–15 reps.
To increase difficulty:
- Step further away from the wall for more ankle movement.
- Perform a “Tib Plank” by lifting hips off the wall and keeping knees straight.
It’s recommended to do 3 sets per day, with 1-minute rests between.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
The Secret to Better Squats: Foot, Knee, & Ankle Mobility
Take care!
Share This Post
-
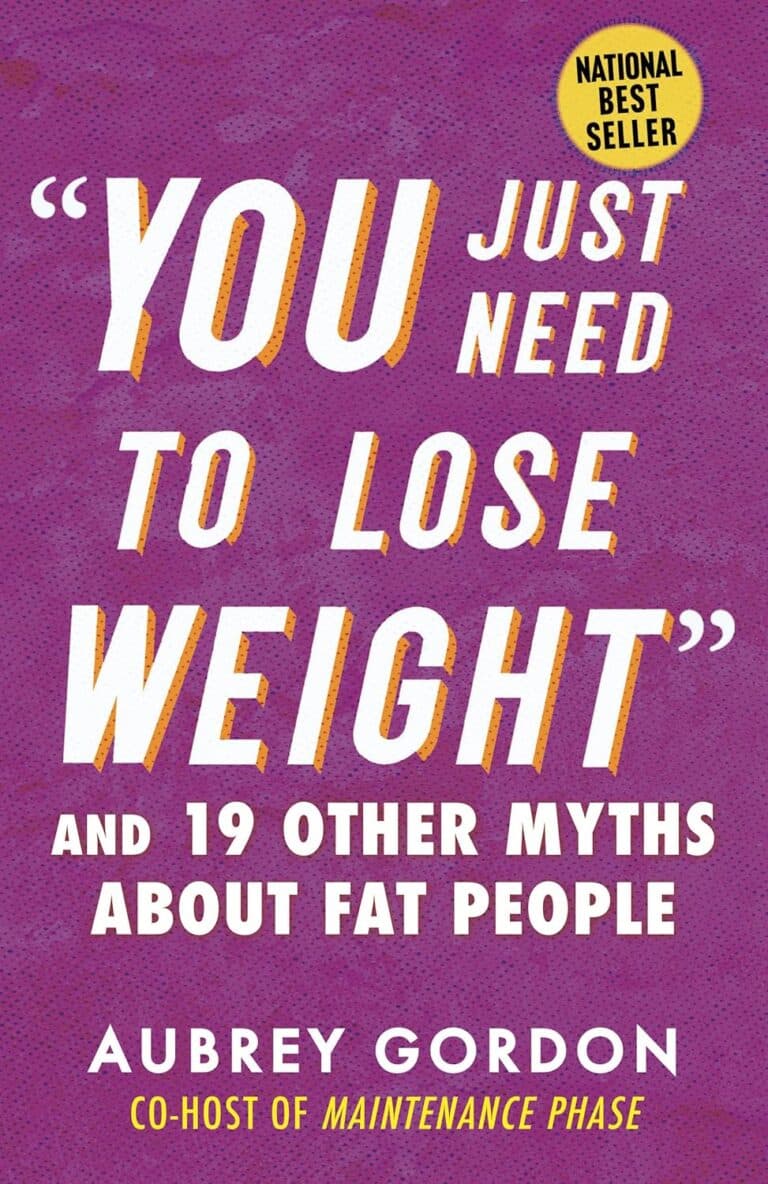
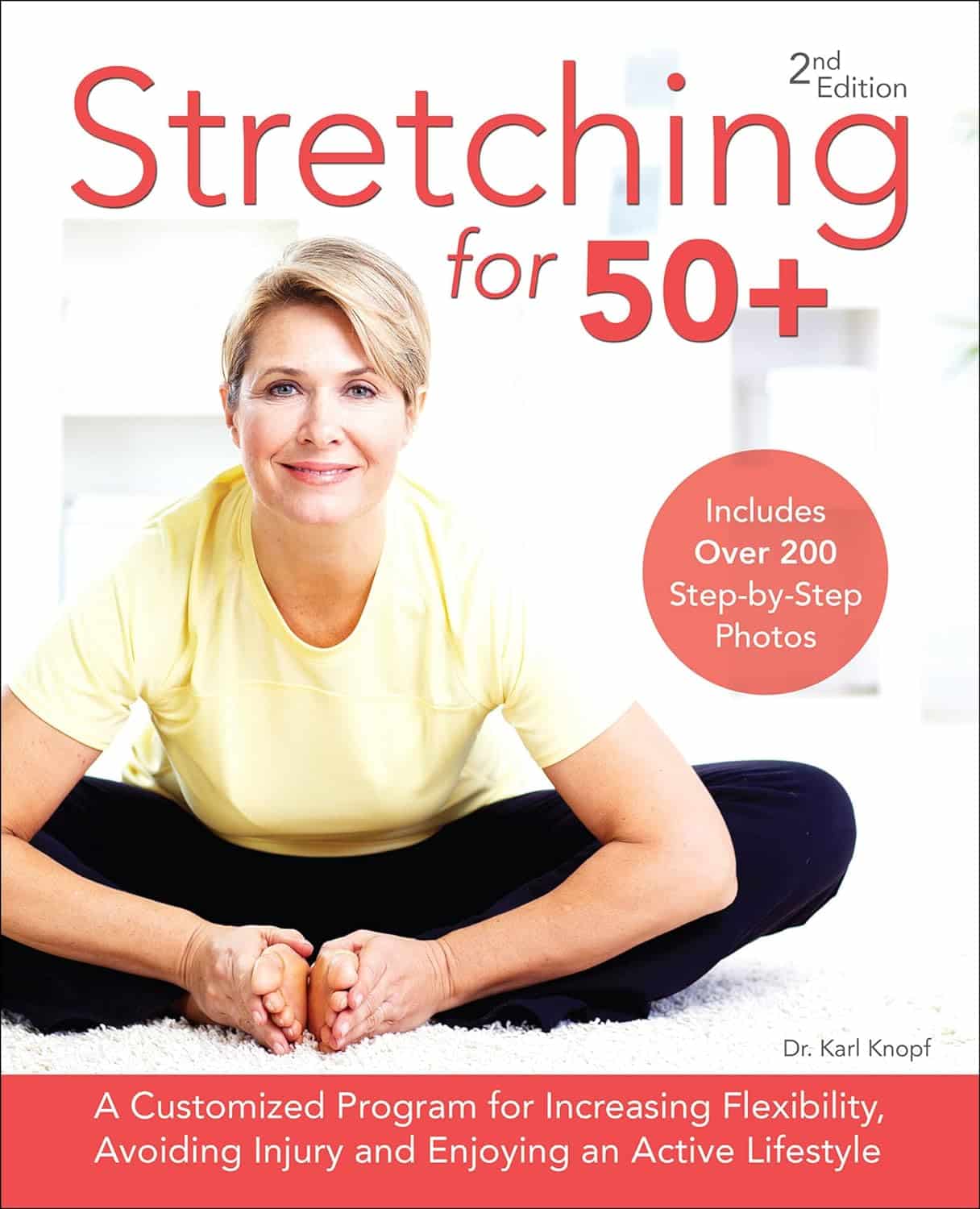
Stretching for 50+ – by Dr. Karl Knopf
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Knopf explores in this book the two-way relationship between aging and stretching (i.e., each can have a large impact on the other). Thinking about stretching in those terms is an important reframe for going into any stretching program. We’d say “after the age of 50”, but honestly, at any age. But this book is written with over-50s in mind, as the title goes.
There’s an extensive encyclopedic section on stretches per body part, which is exactly as you might expect from any book of this kind. There is also a flexibility self-assessment, so that progress can be measured easily, and so that the reader knows where might need more improvement.
Perhaps this book’s greatest strength is the section on specialized programs based on things ranging from working to improve symptoms of any chronic conditions you may have (or at least working around them, if outright improvement is not possible by stretching), to your recreational activities of importance to you—so, what kinds of flexibilities will be important to you, and also, what kinds of injury you are most likely to need to avoid.
Bottom line: if you’re 50 and would like to do more stretching and less aging, then this book can help with that.
Click here to check out Stretching for 50+, and extend your healthspan!
Share This Post
-
What Macronutrient Balance Is Right For You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I want to learn more about macros. Can you cover that topic?❞
That’s a little broader than we usually go for, given the amount of space we have, but let’s give it a go!
Macronutrients, or “macros”, are the nutrients that we typically measure in grams rather than milligrams or micrograms, and are:
- Carbohydrates
- …and what kinds, of which usually the focus is on how much is sugars as opposed to more complex carbs that take longer to break down. See also: Should You Go Light Or Heavy On Carbs?
- …and of the sugars, the interested may further categorize them into sucrose, fructose, etc. See also: Which Sugars Are Healthier, And Which Are Just The Same?
- Proteins
- …of which, the amino acid make-up is generally considered a matter of micronutrients. See also: Protein: How Much Do We Need, Really?
- Fats
- …and what kinds, i.e. monounsaturated vs polyunsaturated vs saturated. See also: Saturated Fat: What’s The Truth?
- …and then the interested may further categorize them for their fatty acids / triglycerides profile, etc. See also: What Omega-3 Fatty Acids Really Do For Us
- Fiber
- …which often gets ignored by people counting macros, as “stuff that doesn’t do anything”, despite it in fact being very important for health. See also: Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Water
- …which again tends to get disregarded but is very arguably a critical macronutrient. See also: Busting The Myth of “Eight Glasses Of Water A Day”
In terms of how much we need of each, you can read more in the above-linked articles, but:
- General scientific consensus is we need plenty of fiber (30 or 40g per day is good) and water (highly dependent on climate and activity), and there’s a clear minimum requisite for protein (usually put at around 1g of protein per day per 1kg of body weight).
- There is vigorous debate in the general health community about what the best ratio of carbs to fat is.
The reality is that humans are quite an adaptable species, and while we absolutely do need at least some of both (carbohydrates and fats), we can play around with the ratios quite a bit, provided we don’t get too extreme about it.
While some influence is social and often centered around weight loss (see for example keto which seeks to minimize carbs, and volumetrics, which seeks maximise volume-to-calorie ratio, which de facto tends to minimize fats), some of what drives us to lean one way or the other will be genetics, too—dependent on what our ancestors ate more or less of.
Writer’s example: my ancestors could not grow much grain (or crops in general) where they were, so they got more energy from such foods as whale and seal fat (with protein coming more from reindeer). Now, biology is not destiny, and I personally enjoy a vegan diet, but my genes are probably why I am driven to get most of my daily calories from fat (of which, a lot of fatty nuts (don’t tell almonds, but I prefer walnuts and cashews) and healthy oils such as olive oil, avocado oil, and coconut oil).
However! About that adaptability. Provided we make changes slowly, we can usually adjust our diet to whatever we want it to be, including whether we get our energy more from carbs or fats. The reason we need to make changes slowly is because our gut needs time to adjust. For example, if your vegan writer here were to eat her ancestrally-favored foods now, I’d be very ill, because my gut microbiome has no idea what to do with animal products anymore, no matter what genes I have. In contrast, if an enthusiastic enjoyer of a meat-heavy diet were to switch to my fiber-rich diet overnight, they’d be very ill.
So: follow your natural inclinations, make any desired changes slowly, and if in doubt, it’s hard to go wrong with enjoying carbs and fats in moderation.
Learn more: Intuitive Eating Might Not Be What You Think
Take care!
Share This Post
- Carbohydrates
Related Posts
-
What does it mean to be transgender?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Transgender media coverage has surged in recent years for a wide range of reasons. While there are more transgender television characters than ever before, hundreds of bills are targeting transgender people’s access to medical care, sports teams, gender-specific public spaces, and other institutions.
Despite the increase in conversation about the transgender community, public confusion around transgender identity remains.
Read on to learn more about what it means to be transgender and understand challenges transgender people may face.
What does it mean to be transgender?
Transgender—or “trans”—is an umbrella term for people whose gender identity or gender expression does not conform to their sex assigned at birth. People can discover they are trans at any age.
Gender identity refers to a person’s inner sense of being a woman, a man, neither, both, or something else entirely. Trans people who don’t feel like women or men might describe themselves as nonbinary, agender, genderqueer, or two-spirit, among other terms.
Gender expression describes the way a person communicates their gender through their appearance—such as their clothing or hairstyle—and behavior.
A person whose gender expression doesn’t conform to the expectations of their assigned sex may not identify as trans. The only way to know for sure if someone is trans is if they tell you.
Cisgender—or “cis”—describes people whose gender identities match the sex they were assigned at birth.
How long have transgender people existed?
Being trans isn’t new. Although the word “transgender” only dates back to the 1960s, people whose identities defy traditional gender expectations have existed across cultures throughout recorded history.
How many people are transgender?
A 2022 Williams Institute study estimates that 1.6 million people over the age of 13 identify as transgender in the United States.
Is being transgender a mental health condition?
No. Conveying and communicating about your gender in a way that feels authentic to you is a normal and necessary part of self-expression.
Social and legal stigma, bullying, discrimination, harassment, negative media messages, and barriers to gender-affirming medical care can cause psychological distress for trans people. This is especially true for trans people of color, who face significantly higher rates of violence, poverty, housing instability, and incarceration—but trans identity itself is not a mental health condition.
What is gender dysphoria?
Gender dysphoria describes a feeling of unease that some trans people experience when their perceived gender doesn’t match their gender identity, or their internal sense of gender. A 2021 study of trans adults pursuing gender-affirming medical care found that most participants started experiencing gender dysphoria by the time they were 7.
When trans people don’t receive the support they need to manage gender dysphoria, they may experience depression, anxiety, social isolation, suicidal ideation, substance use disorder, eating disorders, and self-injury.
How do trans people manage gender dysphoria?
Every trans person’s experience with gender dysphoria is unique. Some trans people may alleviate dysphoria by wearing gender-affirming clothing or by asking others to refer to them by a new name and use pronouns that accurately reflect their gender identity. The 2022 U.S. Trans Survey found that nearly all trans participants who lived as a different gender than the sex they were assigned at birth reported that they were more satisfied with their lives.
Some trans people may also manage dysphoria by pursuing medical transition, which may involve taking hormones and getting gender-affirming surgery.
Access to gender-affirming medical care has been shown to reduce the risk of depression and suicide among trans youth and adults.
To learn more about the trans community, visit resources from the National Center for Transgender Equality, the Trevor Project, PFLAG, and Planned Parenthood.
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Early Detection May Help Kentucky Tamp Down Its Lung Cancer Crisis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anthony Stumbo’s heart sank after the doctor shared his mother’s chest X-ray.
“I remember that drive home, bringing her back home, and we basically cried,” said the internal medicine physician, who had started practicing in eastern Kentucky near his childhood home shortly before his mother began feeling ill. “Nobody wants to get told they’ve got inoperable lung cancer. I cried because I knew what this meant for her.”
Now Stumbo, whose mother died the following year, in 1997, is among a group of Kentucky clinicians and researchers determined to rewrite the script for other families by promoting training and boosting awareness about early detection in the state with the highest lung cancer death rate. For the past decade, Kentucky researchers have promoted lung cancer screening, first recommended by the U.S. Preventive Services Task Force in 2013. These days the Bluegrass State screens more residents who are at high risk of developing lung cancer than any state except Massachusetts — 10.6% of eligible residents in 2022, more than double the national rate of 4.5% — according to the most recent American Lung Association analysis.
The effort has been driven by a research initiative called the Kentucky LEADS (Lung Cancer Education, Awareness, Detection, and Survivorship) Collaborative, which in 2014 launched to improve screening and prevention, to identify more tumors earlier, when survival odds are far better. The group has worked with clinicians and hospital administrators statewide to boost screening rates both in urban areas and regions far removed from academic medical centers, such as rural Appalachia. But, a decade into the program, the researchers face an ongoing challenge as they encourage more people to get tested, namely the fear and stigma that swirl around smoking and lung cancer.
Lung cancer kills more Americans than any other malignancy, and the death rates are worst in a swath of states including Kentucky and its neighbors Tennessee and West Virginia, and stretching south to Mississippi and Louisiana, according to data from the Centers for Disease Control and Prevention.
It’s a bit early to see the impact on lung cancer deaths because people may still live for years with a malignancy, LEADS researchers said. Plus, treatment improvements and other factors may also help reduce death rates along with increased screening. Still, data already shows that more cancers in Kentucky are being detected before they become advanced, and thus more difficult to treat, they said. Of total lung cancer cases statewide, the percentage of advanced cases — defined as cancers that had spread to the lymph nodes or beyond — hovered near 81% between 2000 and 2014, according to Kentucky Cancer Registry data. By 2020, that number had declined to 72%, according to the most recent data available.
“We are changing the story of families. And there is hope where there has not been hope before,” said Jennifer Knight, a LEADS principal investigator.
Older adults in their 60s and 70s can hold a particularly bleak view of their mortality odds, given what their loved ones experienced before screening became available, said Ashley Shemwell, a nurse navigator for the lung cancer screening program at Owensboro Health, a nonprofit health system that serves Kentucky and Indiana.
“A lot of them will say, ‘It doesn’t matter if I get lung cancer or not because it’s going to kill me. So I don’t want to know,’” said Shemwell. “With that generation, they saw a lot of lung cancers and a lot of deaths. And it was terrible deaths because they were stage 4 lung cancers.” But she reminds them that lung cancer is much more treatable if caught before it spreads.
The collaborative works with several partners, including the University of Kentucky, the University of Louisville, and GO2 for Lung Cancer, and has received grant funding from the Bristol Myers Squibb Foundation. Leaders have provided training and other support to 10 hospital-based screening programs, including a stipend to pay for resources such as educational materials or a nurse navigator, Knight said. In 2022, state lawmakers established a statewide lung cancer screening program based in part on the group’s work.
Jacob Sands, a lung cancer physician at Boston’s Dana-Farber Cancer Institute, credits the LEADS collaborative with encouraging patients to return for annual screening and follow-up testing for any suspicious nodules. “What the Kentucky LEADS program is doing is fantastic, and that is how you really move the needle in implementing lung screening on a larger scale,” said Sands, who isn’t affiliated with the Kentucky program and serves as a volunteer spokesperson for the American Lung Association.
In 2014, Kentucky expanded Medicaid, increasing the number of lower-income people who qualified for lung cancer screening and any related treatment. Adults 50 to 80 years old are advised to get a CT scan every year if they have accumulated at least 20 pack years and still smoke or have quit within the past 15 years, according to the latest task force recommendation, which widened the pool of eligible adults. (To calculate pack years, multiply the packs of cigarettes smoked daily by years of smoking.) The lung association offers an online quiz, called “Saved By The Scan,” to figure out likely eligibility for insurance coverage.
Half of U.S. patients aren’t diagnosed until their cancer has spread beyond the lungs and lymph nodes to elsewhere in the body. By then, the five-year survival rate is 8.2%.
But regular screening boosts those odds. When a CT scan detects lung cancer early, patients have an 81% chance of living at least 20 years, according to data published in November in the journal Radiology.
Some adults, like Lisa Ayers, didn’t realize lung cancer screening was an option. Her family doctor recommended a CT scan last year after she reported breathing difficulties. Ayers, who lives in Ohio near the Kentucky border, got screened at UK King’s Daughters, a hospital in far eastern Kentucky. The scan didn’t take much time, and she didn’t have to undress, the 57-year-old said. “It took me longer to park,” she quipped.
She was diagnosed with a lung carcinoid tumor, a type of neuroendocrine cancer that can grow in various parts of the body. Her cancer was considered too risky for surgery, Ayers said. A biopsy showed the cancer was slow-growing, and her doctors said they would monitor it closely.
Ayers, a lifelong smoker, recalled her doctor said that her type of cancer isn’t typically linked to smoking. But she quit anyway, feeling like she’d been given a second chance to avoid developing a smoking-related cancer. “It was a big wake-up call for me.”
Adults with a smoking history often report being treated poorly by medical professionals, said Jamie Studts, a health psychologist and a LEADS principal investigator, who has been involved with the research from the start. The goal is to avoid stigmatizing people and instead to build rapport, meeting them where they are that day, he said.
“If someone tells us that they’re not ready to quit smoking but they want to have lung cancer screening, awesome; we’d love to help,” Studts said. “You know what? You actually develop a relationship with an individual by accepting, ‘No.’”
Nationally, screening rates vary widely. Massachusetts reaches 11.9% of eligible residents, while California ranks last, screening just 0.7%, according to the lung association analysis.
That data likely doesn’t capture all California screenings, as it may not include CT scans done through large managed care organizations, said Raquel Arias, a Los Angeles-based associate director of state partnerships at the American Cancer Society. She cited other 2022 data for California, looking at lung cancer screening for eligible Medicare fee-for-service patients, which found a screening rate of 1%-2% in that population.
But, Arias said, the state’s effort is “nowhere near what it needs to be.”
The low smoking rate in California, along with its image as a healthy state, “seems to have come with the unintended consequence of further stigmatizing people who smoke,” said Arias, citing one of the findings from a 2022 report looking at lung cancer screening barriers. For instance, eligible patients may be reluctant to share prior smoking habits with their health provider, she said.
Meanwhile, Kentucky screening efforts progress, scan by scan.
At Appalachian Regional Healthcare, 3,071 patients were screened in 2023, compared with 372 in 2017. “We’re just scratching the surface of the potential lives that we can have an effect on,” said Stumbo, a lung cancer screening champion at the health system, which includes 14 hospitals, most located in eastern Kentucky.
The doctor hasn’t shed his own grief about what his family missed after his mother died at age 51, long before annual screening was recommended. “Knowing that my children were born, and never knowing their grandmother,” he said, “just how sad is that?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Off-Button For Your Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Off-Button For Your Brain
We evolved our emotions for our own benefit as a species. Even the “negative” ones:
- Stress keeps us safe by making sure we take important situations seriously
- Anger keeps us safe by protecting us from threats
- Disgust keeps us safe by helping us to avoid things that might cause disease
- Anxiety keeps us safe by ensuring we don’t get complacent
- Guilt keeps us safe by ensuring we can function as a community
- Sadness keeps us safe by ensuring we value things that are important to us, and learn to become averse to losing them
- …and so on
But that’s not always useful. What was once a very good response to a common source of fear (for example, a sabre-toothed tiger) is no longer a helpful response to a modern source of fear (for example, an important interview).
Sometimes it’s good to take the time and energy to process our feelings and the event(s) that prompted those feelings. Sometimes, we don’t have that luxury.
For example, if you are stressed about your workload? Then staying awake half the night thinking about it is only going to make your problems worse the next day.
So, how to switch that off, or at least put a pause on it?
The human mind tends to have a “negative bias”, evolved for our own protection. If something is “good enough”, we don’t need to worry about it, so we move on to the next thing, until we find something that is a problem, then we dwell on that. That’s not always helpful, and the good news is, there’s a way to flip the switch on this process:
Identifying the positive, and releasing the rest
This exercise can be done when you’re trying to sleep, or at any time you need a calmer, quieter mind.
Take a moment to notice whatever you’re experiencing.
If it’s something that feels good, or neutral, identify it with a single word. For example:
- Warmth
- Soft
- Security
- Smile
- Peace
If it’s something that feels bad, then instead of identifying it, simply say (or think) to yourself “release”.
You can’t fight bad feelings with force, and you can’t “just not think about them”, but you can dismiss them as soon as they arrive and move onto the next thing. So where your train of thought may previously have been:
It’s good to be in bed ➔ I have eight hours to sleep before my meeting ➔ Have I done everything I was supposed to? ➔ I hope that what I’ve done is good enough ➔ [Mentally rehearsing how the meeting might go] ➔ [various disaster preparations] ➔ What am I even going to wear? ➔ Ugh I forgot to do the laundry ➔ That reminds the electricity bill is due ➔ Etc
Now your train of thought may be more like:
Relief ➔ Rest ➔ But my meeti—release ➔ If I—release ➔ soft ➔ comfort ➔ release ➔ pillow ➔ smile ➔ release ➔ [and before you know it you’re asleep]
And if you do this in a situation where you’re not going to sleep? Same process, just a more wakeful result, for example, let’s move the scene to an office where your meeting will shortly take place:
Five minutes to go ➔ What a day ➔ Ok, I’d better clear my head a bit ➔ release ➔ release ➔ breath ➔ light ➔ chair ➔ what if—release ➔ prepared ➔ ready ➔ calm ➔ [and before you know it you’re impressing your work associate with your calm preparedness]
In summary:
If you need to stop a train of thought, this method may help. Especially if you’re in a situation where you can’t use some external distraction to keep you from thinking about the bad thing!
You’re probably still going to have to deal with the Bad Thing™ at some point—you’ve just recognized that now isn’t the time for that. Mentally postpone that so that you will be well-rested when you choose to deal with the Bad Thing™ later at your convenience.
So remember: identify the positive (with a single word), and anything else, just release.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: