Mindfulness – by Olivia Telford
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Olivia Telford takes us on a tour of mindfulness, meditation, mindfulness meditation, and how each of these things impacts stress, anxiety, and depression—as well as less obvious things too, like productivity and relationships.
In the category of how much this is a “how-to-” guide… It’s quite a “how-to” guide. We’re taught how to meditate, we’re taught assorted mindfulness exercises, and we’re taught specific mindfulness interventions such as beating various life traps (e.g. procrastination, executive dysfunction, etc) with mindfulness.
The writing style is simple and to the point, explanatory and very readable. References are made to pop-science and hard science alike, and all in all, is not too far from the kind of writing you might expect to find here at 10almonds.
Bottom line: if you’d like to practice mindfulness meditation and want an easy “in”, or perhaps you’re curious and wonder what mindfulness could tangibly do for you and how, then this book is a great choice for that.
Click here to check out Mindfulness, and enjoy being more present in life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Yes, you still need to use sunscreen, despite what you’ve heard on TikTok
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Summer is nearly here. But rather than getting out the sunscreen, some TikTokers are urging followers to chuck it out and go sunscreen-free.
They claim it’s healthier to forgo sunscreen to get the full benefits of sunshine.
Here’s the science really says.
Karolina Grabowska/Pexels How does sunscreen work?
Because of Australia’s extreme UV environment, most people with pale to olive skin or other risk factors for skin cancer need to protect themselves. Applying sunscreen is a key method of protecting areas not easily covered by clothes.
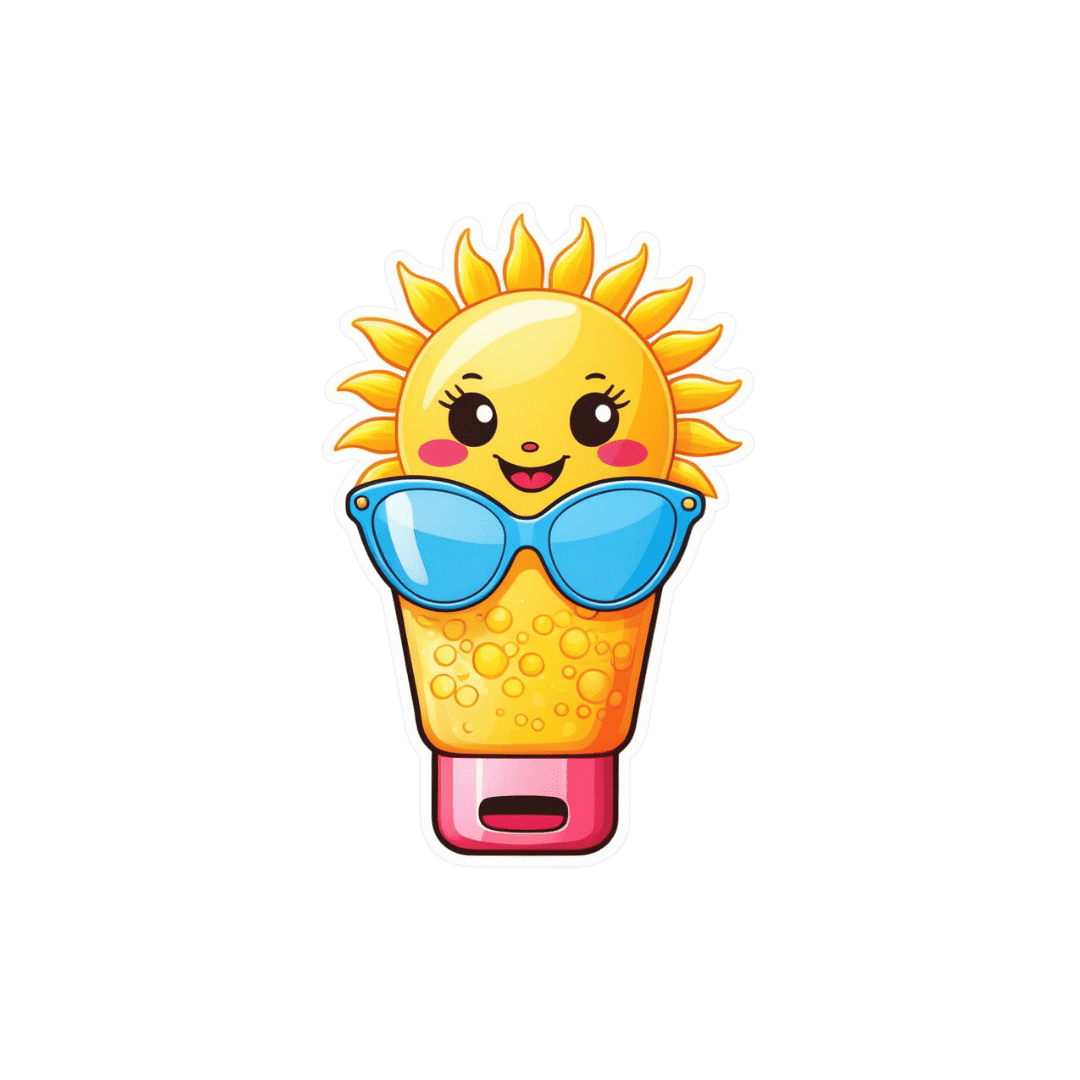
Sunscreen works by absorbing or scattering UV rays before they can enter your skin and damage DNA or supportive structures such as collagen.
When UV particles hit DNA, the excess energy can damage our DNA. This damage can be repaired, but if the cell divides before the mistake is fixed, it causes a mutation that can lead to skin cancers.
The energy from a particle of UV (a photon) causes DNA strands to break apart and reconnect incorrectly. This causes a bump in the DNA strand that makes it difficult to copy accurately and can introduce mutations. NASA/David Herring The most common skin cancers are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Melanoma is less common, but is the most likely to spread around the body; this process is called metastasis.
Two in three Australians will have at least one skin cancer in their lifetime, and they make up 80% of all cancers in Australia.
Around 99% of skin cancers in Australia are caused by excessive exposure to UV radiation.
Excessive exposure to UV radiation also affects the appearance of your skin. UVA rays are able to penetrate deep into the skin, where they break down supportive structures such as elastin and collagen.
This causes signs of premature ageing, such as deep wrinkling, brown or white blotches, and broken capillaries.
Sunscreen can help prevent skin cancers
Used consistently, sunscreen reduces your risk of skin cancer and slows skin ageing.
In a Queensland study, participants either used sunscreen daily for almost five years, or continued their usual use.
At the end of five years, the daily-use group had reduced their risk of squamous cell carcinoma by 40% compared to the other group.
Ten years later, the daily use group had reduced their risk of invasive melanoma by 73%
Does sunscreen block the health-promoting properties of sunlight?
The answer is a bit more complicated, and involves personalised risk versus benefit trade-offs.
First, the good news: there are many health benefits of spending time in the sun that don’t rely on exposure to UV radiation and aren’t affected by sunscreen use.
Sunscreen only filters UV rays, not all light. Ron Lach/Pexels Sunscreen only filters UV rays, not visible light or infrared light (which we feel as heat). And importantly, some of the benefits of sunlight are obtained via the eyes.
Visible light improves mood and regulates circadian rhythm (which influences your sleep-wake cycle), and probably reduces myopia (short-sightedness) in children.
Infrared light is being investigated as a treatment for several skin, neurological, psychiatric and autoimmune disorders.
So what is the benefit of exposing skin to UV radiation?
Exposing the skin to the sun produces vitamin D, which is critical for healthy bones and muscles.
Vitamin D deficiency is surprisingly common among Australians, peaking in Victoria at 49% in winter and being lowest in Queensland at 6% in summer.
Luckily, people who are careful about sun protection can avoid vitamin D deficiency by taking a supplement.
Exposing the skin to UV radiation might have benefits independent of vitamin D production, but these are not proven. It might reduce the risk of autoimmune diseases such as multiple sclerosis or cause release of a chemical that could reduce blood pressure. However, there is not enough detail about these benefits to know whether sunscreen would be a problem.
What does this mean for you?
There are some benefits of exposing the skin to UV radiation that might be blunted by sunscreen. Whether it’s worth foregoing those benefits to avoid skin cancer depends on how susceptible you are to skin cancer.
If you have pale skin or other factors that increase you risk of skin cancer, you should aim to apply sunscreen daily on all days when the UV index is forecast to reach 3.
If you have darker skin that rarely or never burns, you can go without daily sunscreen – although you will still need protection during extended times outdoors.
For now, the balance of evidence suggests it’s better for people who are susceptible to skin cancer to continue with sun protection practices, with vitamin D supplementation if needed.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Rachel Neale, Principal research fellow, QIMR Berghofer Medical Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Mango vs Papaya – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
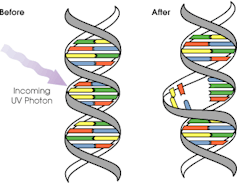
When comparing mango to papaya, we picked the mango.
Why?
Both are great! But there are some things to set them apart:
In terms of macros, this one’s not so big of a difference. They are equal in fiber, while mango has more protein and slightly more carbs. They are both low glycemic index, so we’ll call this one a tie, or the slenderest nominal win for papaya.
When it comes to vitamins, mango has more of vitamins A, B1, B3, B5, B7, B9, E, K, and choline, while papaya has more vitamin C. However, a cup of mango already gives the RDA of vitamin C, so at this point, it’s not even really much of a bonus that papaya has more. In any case, a clear and overwhelming win in the vitamins category for mango.
As for minerals, this one’s closer; mango has more copper, manganese, phosphorus, and zinc, while papaya has more calcium, iron, and magnesium. Still, a 4:3 win for mango.
Adding these up makes for a clear win for mango. However, one extra thing to bear in mind about both:
Both of these fruits interact with warfarin and many other anticoagulants. So if you’re taking those, you might want to skip these, or at least consult with your doctor/pharmacist for input on your personal situation.
Aside from that; enjoy both; diversity is good! But mango is the more nutritionally dense, and thus the winner here.
Want to learn more?
You might like to read:
5 Ways To Make Your Smoothie Blood Sugar Friendly (Avoid the Spike!)
Take care!
Share This Post
-
Gentle Nutrition – by Rachel Hartley, RD, LD
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle here claims “a non-diet approach”, but doesn’t everything, nowadays? Even books titled “The such-and-such Diet” tend to also assure us “it’s not actually a diet; it’s just a way of eating”, as if a diet is not—by definition—a way of eating. Usually what they want to communicate is that it’s not a restrictive diet, usually meaning not restrictive in quantity, or not restrictive in food type (rarely both).
This book is about intuitive eating, which is about as non-restrictive as any dietary approach can be, since it doesn’t restrict food type at at all, and it doesn’t restrict quantity in advance—rather, we learn to pay closer attention to our full signals.
No wait, we don’t. This time, it’s not about “full”, it’s about “satisfied”. This comes in two forms:
- A principle somewhat akin to the “eat until 80% full” idea
- A principle of ensuring the good is culinarily satisfying
This latter is important, if we want to have a good relationship with eating, and it also helps reduce portion sizes, when we truly take the time to mindfully savor a tasty morsel, rather than wolf down a plate of mediocre food.
The style is one that balance being encouraging with delivering science to back up that encouragement. This not only means encouragement to take up this dietary approach, but also, encouragement to let go of things like calorie-counting and BMI.
The recipes arranged per meal type, and indeed include things not found in many healthy eating books, such as gyoza dumplings, gnocchi, wontons, and shortbread. The recipes are mostly not, by default, vegan, vegetarian, gluten-free, dairy-free, or such. So if you have your own food restriction(s), the number of usable recipes will be diminished, barring any substitutions you can make yourself.
Bottom line: this is more about about how to go about intuitive eating, than it is a book with a lot of nutritional information (though there is some of that too). If you’d like to get going with intuitive eating, then this book can help.
Click here to check out Gentle Nutrition, and nourish gently!
Share This Post
Related Posts
-
Hello Sleep – by Dr. Jade Wu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed other sleep books before, so what makes this one stand out?
Mostly, it’s because this one takes quite a different approach.
While still giving a nod to the sensible advice you’ve already read in many places (including here at 10almonds), Dr. Wu looks to help the reader avoid falling into the trap (or: help the reader get out of the trap, if already there) of focussing so much on getting better sleep that it becomes an all-consuming stressor that takes up much of the day thinking about it, and guess what, much of the night too, because you’re busy working out how sleep-deprived you’re going to be tomorrow.
Instead, Dr. Wu recommends to work with your body rather than against it, worry less, and ultimately sleep better. Of course, the “how” of this is what makes most of the book.
She does also give chapters on things that may be different for you, based on such things as hormones, age, or medical conditions.
The writing style is pop-science but with frequent references to scientific papers as appropriate, making good science very accessible.
Bottom line: if you’ve tried everything else and/but good sleep still eludes you, this book will help you to end the battle and make friends with your sleep (a metaphor the author uses throughout the book, by the way).
Click here to check out Hello Sleep, and indeed get better sleep!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are GMOs Good Or Bad For Us?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unzipping Our Food’s Genes
In yesterday’s newsletter, we asked you for your (health-related) views on GMOs.
But what does the science say?
First, a note on terms
Technically, we (humans) have been (g)enetically (m)odifying (o)rganisms for thousands of years.
If you eat a banana, you are enjoying the product of many generations of artificial selection, to change its genes to produce a fruit that is soft, sweet, high in nutrients, and digestible without cooking. The original banana plant would be barely recognizable to many people now (and also, barely edible). We’ve done similarly with countless other food products.
So in this article, we’re going to be talking exclusively about modern genetic modification of organisms, using exciting new (ish, new as in “in the last century”) techniques to modify the genes directly, in a copy-paste fashion.
For more details on the different kinds of genetic modification of organisms, and how they’re each done (including the modern kinds), check out this great article from Sciencing, who explain it in more words than we have room for here:
Sciencing | How Are GMOs Made?
(the above also offers tl;dr section summaries, which are great too)
GMOS are outright dangerous (cancer risks, unknown risks, etc): True or False?
False, so far as we know, in any direct* fashion. Obviously “unknown risks” is quite a factor, since those are, well, unknown. But GMOs on the market undergo a lot of safety testing, and have invariably passed happily.
*However! Glyphosate (the herbicide), on the other hand, has a terrible safety profile and is internationally banned in very many countries for this reason.
Why is this important? Because…
- in the US (and two out of ten Canadian provinces), glyphosate is not banned
- In the US (and we may hypothesize, those two Canadian provinces) one of the major uses of genetic modification of foodstuffs is to make it resistant to glyphosate
- Consequently, GMO foodstuffs grown in those places have generally been liberally doused in glyphosate
So… It’s not that the genetic modification itself makes the food dangerous and potentially carcinogenic (it doesn’t), but it is that the genetic modification makes it possible to use a lot more glyphosate without losing crops to glyphosate’s highly destructive properties.
Which results in the end-consumer eating glyphosate. Which is not good. For example:
❝Following the landmark case against Monsanto, which saw them being found liable for a former groundskeeper, 46 year old Dewayne Johnson’s cancer, 32 countries have to date banned the use of Glyphosate, the key ingredient in Monsanto’s Roundup weed killer. The court awarded Johnson R4.2 billion in damages finding Monsanto “acted with malice or oppression”.❞
Source: see below!
You can read more about where glyphosate is and isn’t banned, here:
33 countries ban the use of Glyphosate—the key ingredient in Roundup
For the science of this (and especially the GMO → glyphosate use → cancer pipeline), see:
Use of Genetically Modified Organism (GMO)-Containing Food Products in Children
GMOs are extra healthy because of the modifications (they were designed for that, right?): True or False?
True or False depending on who made them and why! As we’ve seen above, not all companies seem to have the best interests of consumer health in mind.
However, they can be! Here are a couple of great examples:
❝Recently, two genome-edited crops targeted for nutritional improvement, high GABA tomatoes and high oleic acid soybeans, have been released to the market.
Nutritional improvement in cultivated crops has been a major target of conventional genetic modification technologies as well as classical breeding methods❞
Source: Drs. Nagamine & Ezura
Read in full: Genome Editing for Improving Crop Nutrition
(note, they draw a distinction of meaning between genome editing and genetic modification, according to which of two techniques is used, but for the purposes of our article today, this is under the same umbrella)
Want to know more?
If you’d like to read more about this than we have room for here, here’s a great review in the Journal of Food Science & Nutrition:
Should we still worry about the safety of GMO foods? Why and why not? A review
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hearing loss is twice as common in Australia’s lowest income groups, our research shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Around one in six Australians has some form of hearing loss, ranging from mild to complete hearing loss. That figure is expected to grow to one in four by 2050, due in a large part to the country’s ageing population.
Hearing loss affects communication and social engagement and limits educational and employment opportunities. Effective treatment for hearing loss is available in the form of communication training (for example, lipreading and auditory training), hearing aids and other devices.
But the uptake of treatment is low. In Australia, publicly subsidised hearing care is available predominantly only to children, young people and retirement-age people on a pension. Adults of working age are mostly not eligible for hearing health care under the government’s Hearing Services Program.
Our recent study published in the journal Ear and Hearing showed, for the first time, that working-age Australians from lower socioeconomic backgrounds are at much greater risk of hearing loss than those from higher socioeconomic backgrounds.
We believe the lack of socially subsidised hearing care for adults of working age results in poor detection and care for hearing loss among people from disadvantaged backgrounds. This in turn exacerbates social inequalities.
Population data shows hearing inequality
We analysed a large data set called the Household, Income and Labour Dynamics in Australia (HILDA) survey that collects information on various aspects of people’s lives, including health and hearing loss.
Using a HILDA sub-sample of 10,719 working-age Australians, we evaluated whether self-reported hearing loss was more common among people from lower socioeconomic backgrounds than for those from higher socioeconomic backgrounds between 2008 and 2018.
Relying on self-reported hearing data instead of information from hearing tests is one limitation of our paper. However, self-reported hearing tends to underestimate actual rates of hearing impairment, so the hearing loss rates we reported are likely an underestimate.
We also wanted to find out whether people from lower socioeconomic backgrounds were more likely to develop hearing loss in the long run.
Hearing care is publicly subsidised for children.
mady70/ShutterstockWe found people in the lowest income groups were more than twice as likely to have hearing loss than those in the highest income groups. Further, hearing loss was 1.5 times as common among people living in the most deprived neighbourhoods than in the most affluent areas.
For people reporting no hearing loss at the beginning of the study, after 11 years of follow up, those from a more deprived socioeconomic background were much more likely to develop hearing loss. For example, a lack of post secondary education was associated with a more than 1.5 times increased risk of developing hearing loss compared to those who achieved a bachelor’s degree or above.
Overall, men were more likely to have hearing loss than women. As seen in the figure below, this gap is largest for people of low socioeconomic status.
Why are disadvantaged groups more likely to experience hearing loss?
There are several possible reasons hearing loss is more common among people from low socioeconomic backgrounds. Noise exposure is one of the biggest risks for hearing loss and people from low socioeconomic backgrounds may be more likely to be exposed to damaging levels of noise in jobs in mining, construction, manufacturing, and agriculture.
Lifestyle factors which may be more prevalent in lower socioeconomic communities such as smoking, unhealthy diet, and a lack of regular exercise are also related to the risk of hearing loss.
Finally, people with lower incomes may face challenges in accessing timely hearing care, alongside competing health needs, which could lead to missed identification of treatable ear disease.
Why does this disparity in hearing loss matter?
We like to think of Australia as an egalitarian society – the land of the fair go. But nearly half of people in Australia with hearing loss are of working age and mostly ineligible for publicly funded hearing services.
Hearing aids with a private hearing care provider cost from around A$1,000 up to more than $4,000 for higher-end devices. Most people need two hearing aids.
Hearing loss might be more common in low income groups because they’re exposed to more noise at work.
Dmitry Kalinovsky/ShutterstockLack of access to affordable hearing care for working-age adults on low incomes comes with an economic as well as a social cost.
Previous economic analysis estimated hearing loss was responsible for financial costs of around $20 billion in 2019–20 in Australia. The largest component of these costs was productivity losses (unemployment, under-employment and Jobseeker social security payment costs) among working-age adults.
Providing affordable hearing care for all Australians
Lack of affordable hearing care for working-age adults from lower socioeconomic backgrounds may significantly exacerbate the impact of hearing loss among deprived communities and worsen social inequalities.
Recently, the federal government has been considering extending publicly subsidised hearing services to lower income working age Australians. We believe reforming the current government Hearing Services Program and expanding eligibility to this group could not only promote a more inclusive, fairer and healthier society but may also yield overall cost savings by reducing lost productivity.
All Australians should have access to affordable hearing care to have sufficient functional hearing to achieve their potential in life. That’s the land of the fair go.
Mohammad Nure Alam, PhD Candidate in Economics, Macquarie University; Kompal Sinha, Associate Professor, Department of Economics, Macquarie University, and Piers Dawes, Professor, School of Health and Rehabilitation Sciences, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: