Magnesium Glycinate vs Magnesium Citrate – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
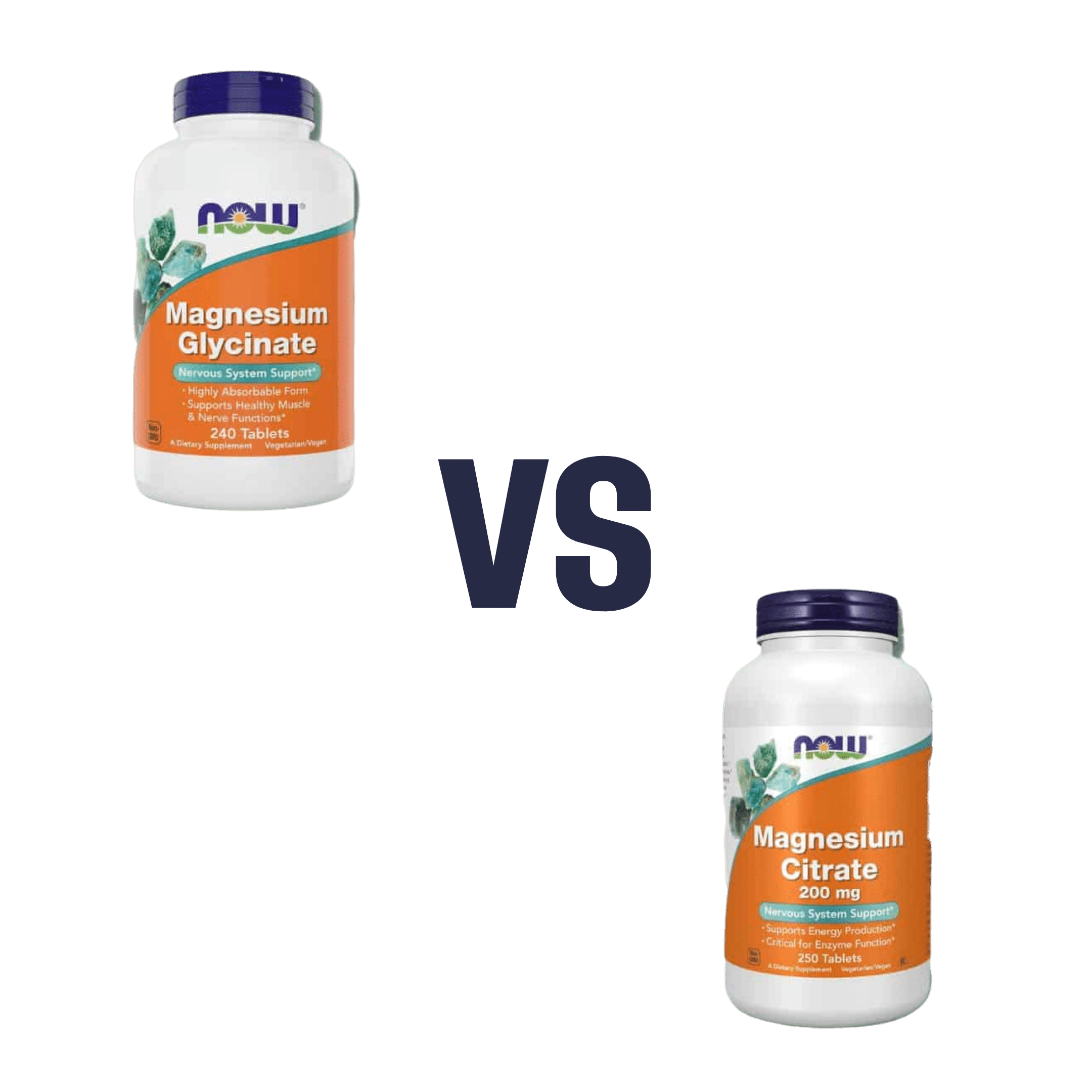
When comparing magnesium glycinate to magnesium citrate, we picked the citrate.
Why?
Both are fine sources of magnesium, a nutrient in which it’s very common to be deficient—a lot of people don’t eat many leafy greens, beans, nuts, and so forth that contain it.
A quick word on a third contender we didn’t include here: magnesium oxide is probably the most widely-sold magnesium supplement because it’s cheapest to make. It also has woeful bioavailability, to the point that there seems to be negligible benefit to taking it. So we don’t recommend that.
Magnesium glycinate and magnesium citrate are both absorbed well, but magnesium citrate is the most well-absorbed form of magnesium supplement.
In terms of the relative merits of the glycine or the citric acid (the “other part” of magnesium glycinate and magnesium citrate, respectively), both are also great nutrients, but the amount delivered with the magnesium is quite small in each case, and so there’s nothing here to swing it one way or the other.
For this reason, we went with the magnesium citrate, as the most readily bioavailable!
Want to try them out?
Here they are on Amazon:
Magnesium glycinate | Magnesium citrate
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Coca-Cola vs Diet Coke – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Coca-Cola to Diet Coke, we picked the Diet Coke.
Why?
While the Diet Coke is bad, the Coca-Cola has mostly the same problems plus sugar.
The sugar in a can of Coca-Cola is 39g high-fructose corn syrup (the worst kind of sugar yet known to humanity), and of course it’s being delivered in liquid form (the most bioavailable way to get, which in this case, is bad).
To put those 39g into perspective, the daily recommended amount of sugar is 36g for men or 25g for women, according to the AHA.
The sweetener in Diet Coke is aspartame, which has had a lot of health risk accusations made against it, most of which have not stood up to scrutiny, and the main risk it does have is “it mimics sugar too well” and it can increase cravings for sweetness, and therefore higher consumption of sugars in other products. For this reason, the World Health Organization has recommended to simply reduce sugar intake without looking to artificial sweeteners to help.
Nevertheless, aspartame has been found safe (in moderate doses; the upper tolerance level would equate to more than 20 cans of diet coke per day) by food safety agencies ranging from the FDA to the EFSA, based on a large body of science.
Other problems that Diet Coke has are present in Coca-Cola too, such as its acidic nature (bad for tooth enamel) and gassy nature (messes with leptin/ghrelin balance).
Summary: the Diet Coke is relatively less unhealthy, but is still bad in numerous ways, and remains best avoided.
Read more:
Share This Post
-
Cannabis Myths vs Reality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cannabis Myths vs Reality
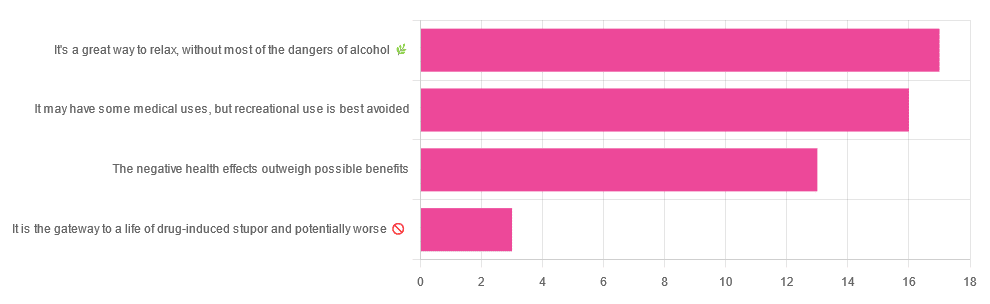
We asked you for your (health-related) opinion on cannabis use—specifically, the kind with psychoactive THC, not just CBD. We got the above-pictured, below-described, spread of responses:
- A little over a third of you voted for “It’s a great way to relax, without most of the dangers of alcohol”.
- A little under a third of you voted for “It may have some medical uses, but recreational use is best avoided”.
- About a quarter of you voted for “The negative health effects outweigh the possible benefits”
- Three of you voted for “It is the gateway to a life of drug-induced stupor and potentially worse”
So, what does the science say?
A quick legal note first: we’re a health science publication, and are writing from that perspective. We do not know your location, much less your local laws and regulations, and so cannot comment on such. Please check your own local laws and regulations in that regard.
Cannabis use can cause serious health problems: True or False?
True. Whether the risks outweigh the benefits is a personal and subjective matter (for example, a person using it to mitigate the pain of late stage cancer is probably unconcerned with many other potential risks), but what’s objectively true is that it can cause serious health problems.
One subscriber who voted for “The negative health effects outweigh the possible benefits” wrote:
❝At a bare minimum, you are ingesting SMOKE into your lungs!! Everyone SEEMS TO BE against smoking cigarettes, but cannabis smoking is OK?? Lung cancer comes in many forms.❞
Of course, that is assuming smoking cannabis, and not consuming it as an edible. But, what does the science say on smoking it, and lung cancer?
There’s a lot less research about this when it comes to cannabis, compared to tobacco. But, there is some:
❝Results from our pooled analyses provide little evidence for an increased risk of lung cancer among habitual or long-term cannabis smokers, although the possibility of potential adverse effect for heavy consumption cannot be excluded.❞
Read: Cannabis smoking and lung cancer risk: Pooled analysis in the International Lung Cancer Consortium
Another study agreed there appears to be no association with lung cancer, but that there are other lung diseases to consider, such as bronchitis and COPD:
❝Smoking cannabis is associated with symptoms of chronic bronchitis, and there may be a modest association with the development of chronic obstructive pulmonary disease. Current evidence does not suggest an association with lung cancer.❞
Read: Cannabis Use, Lung Cancer, and Related Issues
Cannabis edibles are much safer than smoking cannabis: True or False?
Broadly True, with an important caveat.
One subscriber who selected “It may have some medical uses, but recreational use is best avoided”, wrote:
❝I’ve been taking cannabis gummies for fibromyalgia. I don’t know if they’re helping but they’re not doing any harm. You cannot overdose you don’t become addicted.❞
Firstly, of course consuming edibles (rather than inhaling cannabis) eliminates the smoke-related risk factors we discussed above. However, other risks remain, including the much greater ease of accidentally overdosing.
❝Visits attributable to inhaled cannabis are more frequent than those attributable to edible cannabis, although the latter is associated with more acute psychiatric visits and more ED visits than expected.❞
Note: that “more frequent” for inhaled cannabis, is because more people inhale it than eat it. If we adjust the numbers to control for how much less often people eat it, suddenly we see that the numbers of hospital admissions are disproportionately high for edibles, compared to inhaled cannabis.
Or, as the study author put it:
❝There are more adverse drug events associated on a milligram per milligram basis of THC when it comes in form of edibles versus an inhaled cannabis. If 1,000 people smoked pot and 1,000 people at the same dose in an edible, then more people would have more adverse drug events from edible cannabis.❞
See the numbers: Acute Illness Associated With Cannabis Use, by Route of Exposure
Why does this happen?
- It’s often because edibles take longer to take effect, so someone thinks “this isn’t very strong” and has more.
- It’s also sometimes because someone errantly eats someone else’s edibles, not realising what they are.
- It’s sometimes a combination of the above problems: a person who is now high, may simply forget and/or make a bad decision when it comes to eating more.
On the other hand, that doesn’t mean inhaling it is necessarily safer. As well as the pulmonary issues we discussed previously, inhaling cannabis has a higher risk of cannabinoid hyperemesis syndrome (and the resultant cyclic vomiting that’s difficult to treat).
You can read about this fascinating condition that’s sometimes informally called “scromiting”, a portmanteau of screaming and vomiting:
Cannabinoid Hyperemesis Syndrome
You can’t get addicted to cannabis: True or False?
False. However, it is fair to say that the likelihood of developing a substance abuse disorder is lower than for alcohol, and much lower than for nicotine.
See: Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013
If you prefer just the stats without the science, here’s the CDC’s rendering of that:
Addiction (Marijuana or Cannabis Use Disorder)
However, there is an interesting complicating factor, which is age. One is 4–7 times more likely to develop a substance abuse disorder, if one starts use as an adolescent, rather than later in life:
Cannabis is the gateway to use of more dangerous drugs: True or False?
False, generally speaking. Of course, for any population there will be some outliers, but there appears to be no meaningful causal relation between cannabis use and other substance use:
Interestingly, the strongest association (where any existed at all) was between cannabis use and opioid use. However, rather than this being a matter of cannabis use being a gateway to opioid use, it seems more likely that this is a matter of people looking to both for the same purpose: pain relief.
As a result, growing accessibility of cannabis may actually reduce opioid problems:
- Cannabis as a Gateway Drug for Opioid Use Disorder
- Association between medical cannabis laws and opioid overdose mortality has reversed over time
Some final words…
Cannabis is a complex drug with complex mechanisms and complex health considerations, and research is mostly quite young, due to its historic illegality seriously cramping science by reducing sample sizes to negligible. Simply put, there’s a lot we still don’t know.
Also, we covered some important topics today, but there were others we didn’t have time to cover, such as the other potential psychological benefits—and risks. Likely we’ll revisit those another day.
Lastly, while we’ve covered a bunch of risks today, those of you who said it has fewer and lesser risks than alcohol are quite right—the only reason we couldn’t focus on that more, is because to talk about all the risks of alcohol would make this feature many times longer!
Meanwhile, whether you partake or not, stay safe and stay well.
Share This Post
-
10,000 Steps, 30 Days, 4 Changes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ariel wasn’t the most active person, and took on a “30 day challenge” to do the commonly-prescribed 10,000 steps per day—without adjusting her diet or doing any other exercise. How much of a difference does it make, really?
Stepping onwards
The 4 main things that she found changed for her weren’t all what she expected:
- Weight loss yes, but only marginally: she lost 3 lbs in a month, which did nevertheless make a visible difference. We might hypothesize that part of the reason for the small weight loss and yet visible difference is that she gained a little muscle, and the weight loss was specifically shifting away from a cortisol-based fat distribution, to a more healthy fat distribution.
- Different eating habits: she felt less hungry and craved less sugar. This likely has less to do with calorie consumption, and more to do with better insulin signalling.
- Increased energy and improved mood: these are going together in one item, because she said “4 things”, but really they are two related things. So, consider one of them a bonus item! In any case, she felt more energized and productive, and less reliant on caffeine.
- Improved sleep: or rather, at first, disrupted sleep, and then slept better and stayed better. A good reminder that changes for the better don’t always feel better in the first instance!
To hear about it in her own words, and see the before and after pictures, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
Fat’s Real Barriers To Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fat Justice In Healthcare
This is Aubrey Gordon, an author, podcaster, and fat justice activist. What does that mean?
When it comes to healthcare, we previously covered some ideas very similar to her work, such as how…
There’s a lot of discrimination in healthcare settings
In this case, it often happens that a thin person goes in with a medical problem and gets treated for that, while a fat person can go in with the same medical problem and be told “you should try losing some weight”.
Top tip if this happens to you… Ask: “what would you advise/prescribe to a thin person with my same symptoms?”
Other things may be more systemic, for example:
When a thin person goes to get their blood pressure taken, and that goes smoothly, while a fat person goes to get their blood pressure taken, and there’s not a blood pressure cuff to fit them, is the problem the size of the person or the size of the cuff? It all depends on perspective, in a world built around thin people.
That’s a trivial-seeming example, but the same principle has far-reaching (and harmful) implications in healthcare in general, e.g:
- Surgeons being untrained (and/or unwilling) to operate on fat people
- Getting a one-size-fits-all dose that was calculated using average weight, and now doesn’t work
- MRI machines are famously claustrophobia-inducing for thin people; now try not fitting in it in the first place
…and so forth. So oftentimes, obesity will be correlated with a poor healthcare outcome, where the problem is not actually the obesity itself, but rather the system having been set up with thin people in mind.
It would be like saying “Having O- blood type results in higher risks when receiving blood transfusions”, while omitting to add “…because we didn’t stock O- blood”.
Read more on this topic: Shedding Some Obesity Myths
Does she have practical advice about this?
If she could have you understand one thing, it would be:
You deserve better.
Or if you are not fat: your fat friends deserve better.
How this becomes useful is: do not accept being treated as the problem!
Demand better!
If you meekly accept that you “just need to lose weight” and that thus you are the problem, you take away any responsibility from your healthcare provider(s) to actually do their jobs and provide healthcare.
See also Gordon’s book, which we’ve not reviewed yet but probably will one of these days:
“You Just Need to Lose Weight”: And 19 Other Myths About Fat People – by Aubrey Gordon
Are you saying fat people don’t need to lose weight?
That’s a little like asking “would you say office workers don’t need to exercise more?”; there are implicit assumptions built into the question that are going unaddressed.
Rather: some people might benefit healthwise from losing weight, some might not.
In fact, over the age of 65, being what is nominally considered “overweight” reduces all-cause mortality risk.
For details of that and more, see: When BMI Doesn’t Measure Up
But what if I do want/need to lose weight?
Gordon’s not interested in helping with that, but we at 10almonds are, so…
Check out: Lose Weight, But Healthily
Where can I find more from Aubrey Gordon?
You might enjoy her blog:
Aubrey Gordon | Your Fat Friend
Or her other book, which we reviewed previously:
What We Don’t Talk About When We Talk About Fat – by Aubrey Gordon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s So Special About Alpha-Lipoic Acid?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Access-All-Areas Antioxidant
Alpha-Lipoic Acid (ALA) is one of the most bioavailable antioxidants in existence. A bold claim, but most antioxidants are only water-soluble or fat-soluble, whereas ALA is both. This has far-reaching implications—and we mean that literally, because its “go everywhere” status means that it can access (and operate in) all living cells of the human body.
We make it inside our body, and we can also get it in our diet, or take it as a supplement.
What foods contain it?
The richest food sources are:
- For the meat-eaters: organ meats
- For everyone: broccoli, tomatoes, & spinach
However, supplements are more efficient at delivering it, by several orders of magnitude:
Read more: Lipoic acid – biological activity and therapeutic potential
What are its benefits?
Most of its benefits are the usual benefits you would expect from any antioxidant, just, more of it. In particular, reduced inflammation and slowed skin aging are common reasons that people take ALA as a supplement.
Does it really reduce inflammation?
Yes, it does. This one’s not at all controversial, as this systematic review of studies shows:
(C-reactive protein is a marker of inflammation)
Does it really reduce skin aging?
Again yes—which again is not surprising for such a potent antioxidant; remember that oxidative stress is one of the main agonists of cellular aging:
As a special feature, ALA shows particular strength against sun-related skin aging, because of how it protects against UV radiation and increases levels of gluthianone, which also helps:
- Photochemical stability of lipoic acid and its impact on skin ageing
- Modern approach to topical treatment of aging skin
Where can I get some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is Dairy Scary?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is Dairy Scary?
Milk and milk products are popularly enjoyed as a good source of calcium and vitamin D.
In contrast, critics of dairy products (for medical reasons, rather than ethical, which is another matter entirely and beyond the scope of this article) point to risks of cancer, heart disease, and—counterintuitively—osteoporosis. We’ll focus more on the former, but touch on the latter two before closing.
Dairy & Cancer
Evidence is highly conflicting. There are so many studies with so many different results. This is partially explicable by noting that not only is cancer a many-headed beast that comes in more than a hundred different forms and all or any of them may be affected one way or another by a given dietary element, but also… Not all milk is created equal, either!
Joanna Lampe, of the Public Health Sciences division, Fred Hutchinson Cancer Research Center in Seattle, writes:
❝Dairy products are a complex group of foods and composition varies by region, which makes evaluation of their association with disease risk difficult. For most cancers, associations between cancer risk and intake of milk and dairy products have been examined only in a small number of cohort studies, and data are inconsistent or lacking❞
In her systematic review of studies, she noted, for example, that:
- Milk and dairy products contain micronutrients and several bioactive constituents that may influence cancer risk and progression
- There’s probable association between milk intake and lower risk of colorectal cancer
- There’s a probable association between diets high in calcium and increased risk of prostate cancer
- Some studies show an inverse association between intake of cultured dairy products and bladder cancer (i.e., if you eat yogurt you’re less likely to get bladder cancer)
Since that systemic review was undertaken, more research has been conducted, and the results are… Not conclusive, but converging towards a conclusion:
- Dairy products can increase or decrease cancer risk
- The increase in cancer risk seems strongest when milk is consumed in quantities that result in too much calcium. When it comes to calcium, you can absolutely have too much of a good thing—just ask your arteries!
- The decrease in cancer seems to be mostly, if not exclusively, from fermented dairy products. This usually means yogurts. The benefit here is not from the milk itself, but rather from the gut-friendly bacteria.
You may be wondering: “Hardened arteries, gut microbiome health? I thought we were talking about cancer?” and yes we are. No part of your health is an island unrelated to other parts of your health. One thing can lead to another. Sometimes we know how and why, sometimes we don’t, but it’s best to not ignore the data.
The bottom line on dairy products and cancer is:
- Consuming dairy products in general is probably fine
- Yogurt, specifically, is probably beneficial
Dairy and Heart Disease
The reason for the concern is clear enough: it’s largely assumed to be a matter of saturated fat intake.
The best combination of “large” and “recent” that we found was a three-cohort longitudinal study in 2019, which pretty much confirms what was found in smaller or less recent studies:
- There is some evidence to suggest that consumption of dairy can increase all-cause mortality in general, and death from (cancer and) cardiovascular disease in particular
- The evidence is not, however, overwhelming. It is marginal.
Dairy and Osteoporosis
Does dairy cause osteoporosis? Research here tends to fall into one of two categories when it comes to conclusions, so we’ll give an example of each:
- “Results are conflicting, saying yes/no/maybe, and basically we just don’t know”
- “Results are conflicting, but look: cross-sectional and case-control studies say yes; cohort studies say maybe or no; we prefer the cohort studies”
See them for yourself:
- Osteoporosis: Is milk a kindness or a curse?
- Consumption of milk and dairy products and risk of osteoporosis and hip fracture
Conclusion: really, the jury is very much still out on this one
Summary:
- Moderate consumption of dairy products is almost certainly fine
- More specifically: it probably has some (small) pros and some (small) cons
- Yogurt is almost certainly healthier than other dairy products, and is almost universally considered a healthy food (assuming not being full of added sugar etc, of course)
- If you’re going to have non-dairy alternatives to milk, choose wisely!
That’s all we have time for today, but perhaps in a future edition we’ll do a run-down of the pros and cons of various dairy alternatives!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: