Macadamia Nuts vs Brazil Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing macadamia nuts to Brazil nuts, we picked the Brazil nuts.
Why?
They’re a lot more nutrient dense! But watch out…
First, to do due diligence in terms of macros: Brazil nuts have twice as much protein and less fat, as well as being a little higher in fiber and slightly lower in carbs.
In terms of vitamins, Brazil nuts are about 10x higher in vitamin E, while macadamias are somewhat higher in several B-vitamins.
The category of minerals is where it gets interesting. Macadamia nuts are a little higher in iron and considerably higher in Manganese. But… Brazil nuts are a lot higher in calcium, copper, magnesium, phosphorus, potassium, selenium, and zinc.
About that selenium… Specifically, it’s more than 5,000x higher, and a cup of Brazil nuts would give nearly 10,000x the recommended daily amount of selenium. Now, selenium is an essential mineral (needed for thyroid hormone production, for example), and at the RDA it’s good for good health. Your hair will be luscious and shiny. However, go much above that, and selenium toxicity becomes a thing, you may get sick, and it can cause your (luscious and shiny) hair to fall out. For this reason, it’s recommended to eat no more than 3–4 Brazil nuts per day.
In short… Brazil nuts are much more nutrient dense in general, and thus come out on top here. But, they’re so nutrient dense in the case of selenium, that careful moderation is advised.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why STIs Are On The Rise In Older Adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Three Little Words
Sexually Transmitted Infections (STIs) are often thought of as something that predominantly plagues younger people… The truth, however, is different:
❝Rising divorce rates, forgoing condoms as there is no risk of pregnancy, the availability of drugs for sexual dysfunction, the large number of older adults living together in retirement communities, and the increased use of dating apps are likely to have contributed to the growing incidence of STIs in the over-50s.
These data likely underestimate the true extent of the problem as limited access to sexual health services for the over 50s, and trying to avoid the stigma and embarrassment both on the part of older people and healthcare professionals, is leading to this age group not seeking help for STIs.❞
Read more: Managing The Rise In STIs Among Older Adults
That said, there is a gender gap when it comes to the increased risk, for example:
❝A retrospective study from the USA involving 420,790 couples aged 67 to 99 years, found that widowhood was associated with an increased risk of STIs in older men, but not women❞
~ US Dept of Health & Human Services
Source: CDC: | Sexually Transmitted Disease Surveillance
Is abstinence the best preventative, then?
It is inarguably the most effective, but not necessarily the best for everyone.
This is because for most adults, a healthy sex life is an important part of overall wellbeing.
See also: Mythbusting The Big O
Even in this case there is a gender gap in:
- the level of importance placed on frequency of sexual interactions
- what act(s) of sexuality are held to be most important:
❝Among sexually active men, frequent (≥2 times a month) sexual intercourse (P < .001) and frequent kissing, petting, or fondling (P < .001) were associated with greater enjoyment of life.
Among sexually active women, frequent kissing, petting, or fondling was also associated with greater enjoyment of life (P < .001), but there was no significant association with frequent intercourse (P = .101).
Concerns about one’s sex life and problems with sexual function were strongly associated with lower levels of enjoyment of life in men and to a lesser extent in women.❞
Source: Sexual Activity is Associated with Greater Enjoyment of Life in Older Adults
If you have the time to go into it much more deeply, this paper from the Journal of Gerontology is much more comprehensive, looking also at related lifestyle factors, religious/political backgrounds, views on monogamy or non-monogamy (of various kinds), hormonal considerations, the impact of dementia or other long-term disabilities that may affect things, widowhood, and many other elements:
The National Social Life, Health, and Aging Project: An Introduction
What’s the best preventative, then?
Regular health screening for yourself and your partner(s) is an important key to preventative health when it comes to STIs.
You can Google search for a local STI clinic, and worry not, they are invariably discreet and are well-used to everybody coming in. They’re just glad you’re being responsible about things. It’s also not their job to judge your sexual activities, even if it’s something you might have reason to wish to be secretive about, try to be honest there.
Secondly, most of the usual advice about safe sex still goes, even when there’s no risk of pregnancy. For example, if there’s at least one penis involved, then condoms remain the #1 barrier to all manner of potential infections (we know, almost nobody likes condoms, but sometimes the truth isn’t what we want to hear).
Lastly, if there’s at least one vagina involved, then please for the love of all that is holey, do not put anything there that could cause a yeast infection.
What can cause a yeast infection? Pretty much anything with sugar, which includes but is not limited to:
- Most kinds of food that Cosmo-style “liven things up in the bedroom” advice columns might suggest using (including fruit, honey, chocolate sauce, whipped cream, etc)
- Hands that are not clean (watch out for bacteria too)
- A mouth that has recently been eating or drinking anything with sugar in it, and that includes many kinds of alcohol, as well as milk or hot drinks that had milk in
Yeast infections are not nearly so serious as the STIs the other measures are there to avoid, but they’re not fun either, so some sensible policies in that regard are always good!
On a related note, see also: How To Avoid UTIs
Recap on the single most important part of this article:
At all ages, it remains a good health practice—unless one is absolutely celibate—to regularly get oneself and one’s partner(s) checked for STIs.
Take care!
Share This Post
-
Blueberries vs Elderberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blueberries to elderberries, we picked the elderberries.
Why?
Both are certainly top-tier fruits! But…
In terms of macros, elderberries have more than 2x the fiber, while the two berries are approximately equal on other macros. An easy win for elderberries in this category.
In the category of vitamins, blueberries have more of vitamins E, K, and choline, while elderberries have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, and C, scoring another win for elderberries here.
When it comes to minerals, blueberries have more magnesium, manganese, and zinc, while elderberries have more calcium, copper, iron, phosphorus, potassium, and selenium—one more win for elderberries.
In terms of phytochemicals, both berries are (like most berries) an abundant source of polyphenols, but elderberries have more, including more quercetin, too.
Adding up the sections makes for a convincing win for elderberries, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Herbs For Evidence-Based Health & Healing ← elderberry significantly hastens recovery from upper respiratory viral infections 😎
Enjoy!
Share This Post
-
Oral vaccines could provide relief for people who suffer regular UTIs. Here’s how they work
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a recent TikTok video, Australian media personality Abbie Chatfield shared she was starting a vaccine to protect against urinary tract infections (UTIs).
Huge news for the UTI girlies. I am starting a UTI vaccine tonight for the first time.
Chatfield suffers from recurrent UTIs and has turned to the Uromune vaccine, an emerging option for those seeking relief beyond antibiotics.
But Uromune is not a traditional vaccine injected to your arm. So what is it and how does it work?
9nong/Shutterstock First, what are UTIs?
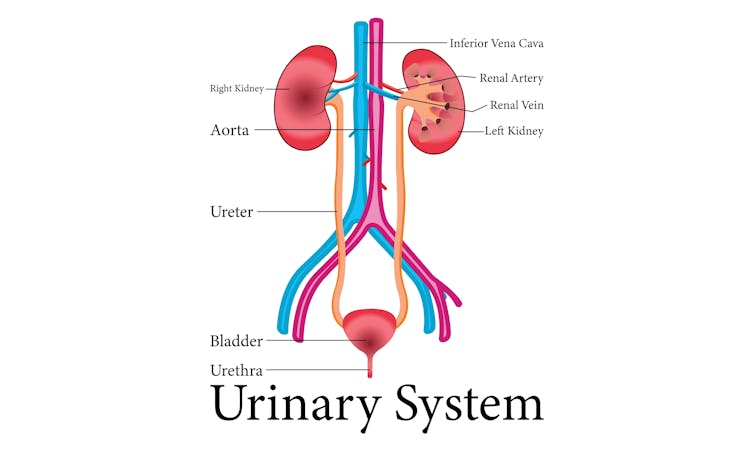
UTIs are caused by bacteria entering the urinary system. This system includes the kidneys, bladder, ureters (thin tubes connecting the kidneys to the bladder), and the urethra (the tube through which urine leaves the body).
The most common culprit is Escherichia coli (E. coli), a type of bacteria normally found in the intestines.
While most types of E. coli are harmless in the gut, it can cause infection if it enters the urinary tract. UTIs are particularly prevalent in women due to their shorter urethras, which make it easier for bacteria to reach the bladder.
Roughly 50% of women will experience at least one UTI in their lifetime, and up to half of those will have a recurrence within six months.
UTIs are caused by bacteria enterning the urinary system. oxo7051/Shutterstock The symptoms of a UTI typically include a burning sensation when you wee, frequent urges to go even when the bladder is empty, cloudy or strong-smelling urine, and pain or discomfort in the lower abdomen or back. If left untreated, a UTI can escalate into a kidney infection, which can require more intensive treatment.
While antibiotics are the go-to treatment for UTIs, the rise of antibiotic resistance and the fact many people experience frequent reinfections has sparked more interest in preventive options, including vaccines.
What is Uromune?
Uromune is a bit different to traditional vaccines that are injected into the muscle. It’s a sublingual spray, which means you spray it under your tongue. Uromune is generally used daily for three months.
It contains inactivated forms of four bacteria that are responsible for most UTIs, including E. coli. By introducing these bacteria in a controlled way, it helps your immune system learn to recognise and fight them off before they cause an infection. It can be classified as an immunotherapy.
A recent study involving 1,104 women found the Uromune vaccine was 91.7% effective at reducing recurrent UTIs after three months, with effectiveness dropping to 57.6% after 12 months.
These results suggest Uromune could provide significant (though time-limited) relief for women dealing with frequent UTIs, however peer-reviewed research remains limited.
Any side effects of Uromune are usually mild and may include dry mouth, slight stomach discomfort, and nausea. These side effects typically go away on their own and very few people stop treatment because of them. In rare cases, some people may experience an allergic reaction.
How can I access it?
In Australia, Uromune has not received full approval from the Therapeutic Goods Administration (TGA), and so it’s not something you can just go and pick up from the pharmacy.
However, Uromune can be accessed via the TGA’s Special Access Scheme or the Authorised Prescriber pathway. This means a GP or specialist can apply for approval to prescribe Uromune for patients with recurrent UTIs. Once the patient has a form from their doctor documenting this approval, they can order the vaccine directly from the manufacturer.
Antibiotics are the go-to treatment for UTIs – but scientists are looking at options to prevent them in the first place. Photoroyalty/Shutterstock Uromune is not covered under the Pharmaceutical Benefits Scheme, meaning patients must cover the full cost out-of-pocket. The cost of a treatment program is around A$320.
Uromune is similarly available through special access programs in places like the United Kingdom and Europe.
Other options in the pipeline
In addition to Uromune, scientists are exploring other promising UTI vaccines.
Uro-Vaxom is an established immunomodulator, a substance that helps regulate or modify the immune system’s response to bacteria. It’s derived from E. coli proteins and has shown success in reducing UTI recurrences in several studies. Uro-Vaxom is typically prescribed as a daily oral capsule taken for 90 days.
FimCH, another vaccine in development, targets something called the adhesin protein that helps E. coli attach to urinary tract cells. FimCH is typically administered through an injection and early clinical trials have shown promising results.
Meanwhile, StroVac, which is already approved in Germany, contains inactivated strains of bacteria such as E. coli and provides protection for up to 12 months, requiring a booster dose after that. This injection works by stimulating the immune system in the bladder, offering temporary protection against recurrent infections.
These vaccines show promise, but challenges like achieving long-term immunity remain. Research is ongoing to improve these options.
No magic bullet, but there’s reason for optimism
While vaccines such as Uromune may not be an accessible or perfect solution for everyone, they offer real hope for people tired of recurring UTIs and endless rounds of antibiotics.
Although the road to long-term relief might still be a bit bumpy, it’s exciting to see innovative treatments like these giving people more options to take control of their health.
Iris Lim, Assistant Professor in Biomedical Science, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
In Defense of Food – by Michael Pollan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eat more like the French. Or the Italians. Or the Japanese. Or…
Somehow, whatever we eat is not good enough, and we should always be doing it differently!
Michael Pollan takes a more down-to-Earth approach.
He kicks off by questioning the wisdom of thinking of our food only in terms of nutritional profiles, and overthinking healthy-eating. He concludes, as many do, that a “common-sense, moderate” approach is needed.
And yet, most people who believe they are taking a “common-sense, moderate” approach to health are in fact over-fed yet under-nourished.
So, how to fix this?
He offers us a reframe: to think of food as a relationship, and health being a product of it:
- If we are constantly stressing about a relationship, it’s probably not good.
- On the other hand, if we are completely thoughtless about it, it’s probably not good either.
- But if we can outline some good, basic principles and celebrate it with a whole heart? It’s probably at the very least decent.
The style is very casual and readable throughout. His conclusions, by the way, can be summed up as “Eat real food, make it mostly plants, and make it not too much”.
However, to summarize it thusly undercuts a lot of the actual value of the book, which is the principles for discerning what is “real food” and what is “not too much”.
Bottom line: if you’re tired of complicated eating plans, this book can help produce something very simple, attainable, and really quite good.
Click here to check out In Defense of Food, for some good, hearty eating.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Health Insurers Limit Coverage of Prosthetic Limbs, Questioning Their Medical Necessity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Michael Adams was researching health insurance options in 2023, he had one very specific requirement: coverage for prosthetic limbs.
Adams, 51, lost his right leg to cancer 40 years ago, and he has worn out more legs than he can count. He picked a gold plan on the Colorado health insurance marketplace that covered prosthetics, including microprocessor-controlled knees like the one he has used for many years. That function adds stability and helps prevent falls.
But when his leg needed replacing last January after about five years of everyday use, his new marketplace health plan wouldn’t authorize it. The roughly $50,000 leg with the electronically controlled knee wasn’t medically necessary, the insurer said, even though Colorado law leaves that determination up to the patient’s doctor, and his has prescribed a version of that leg for many years, starting when he had employer-sponsored coverage.
“The electronic prosthetic knee is life-changing,” said Adams, who lives in Lafayette, Colorado, with his wife and two kids. Without it, “it would be like going back to having a wooden leg like I did when I was a kid.” The microprocessor in the knee responds to different surfaces and inclines, stiffening up if it detects movement that indicates its user is falling.
People who need surgery to replace a joint typically don’t encounter similar coverage roadblocks. In 2021, 1.5 million knee or hip joint replacements were performed in United States hospitals and hospital-owned ambulatory facilities, according to the federal Agency for Healthcare Research and Quality, or AHRQ. The median price for a total hip or knee replacement without complications at top orthopedic hospitals was just over $68,000 in 2020, according to one analysis, though health plans often negotiate lower rates.
To people in the amputee community, the coverage disparity amounts to discrimination.
“Insurance covers a knee replacement if it’s covered with skin, but if it’s covered with plastic, it’s not going to cover it,” said Jeffrey Cain, a family physician and former chair of the board of the Amputee Coalition, an advocacy group. Cain wears two prosthetic legs, having lost his after an airplane accident nearly 30 years ago.
AHIP, a trade group for health plans, said health plans generally provide coverage when the prosthetic is determined to be medically necessary, such as to replace a body part or function for walking and day-to-day activity. In practice, though, prosthetic coverage by private health plans varies tremendously, said Ashlie White, chief strategy and programs officer at the Amputee Coalition. Even though coverage for basic prostheses may be included in a plan, “often insurance companies will put caps on the devices and restrictions on the types of devices approved,” White said.
An estimated 2.3 million people are living with limb loss in the U.S., according to an analysis by Avalere, a health care consulting company. That number is expected to as much as double in coming years as people age and a growing number lose limbs to diabetes, trauma, and other medical problems.
Fewer than half of people with limb loss have been prescribed a prosthesis, according to a report by the AHRQ. Plans may deny coverage for prosthetic limbs by claiming they aren’t medically necessary or are experimental devices, even though microprocessor-controlled knees like Adams’ have been in use for decades.
Cain was instrumental in getting passed a 2000 Colorado law that requires insurers to cover prosthetic arms and legs at parity with Medicare, which requires coverage with a 20% coinsurance payment. Since that measure was enacted, about half of states have passed “insurance fairness” laws that require prosthetic coverage on par with other covered medical services in a plan or laws that require coverage of prostheses that enable people to do sports. But these laws apply only to plans regulated by the state. Over half of people with private coverage are in plans not governed by state law.
The Medicare program’s 80% coverage of prosthetic limbs mirrors its coverage for other services. Still, an October report by the Government Accountability Office found that only 30% of beneficiaries who lost a limb in 2016 received a prosthesis in the following three years.
Cost is a factor for many people.
“No matter your coverage, most people have to pay something on that device,” White said. As a result, “many people will be on a payment plan for their device,” she said. Some may take out loans.
The federal Consumer Financial Protection Bureau has proposed a rule that would prohibit lenders from repossessing medical devices such as wheelchairs and prosthetic limbs if people can’t repay their loans.
“It is a replacement limb,” said White, whose organization has heard of several cases in which lenders have repossessed wheelchairs or prostheses. Repossession is “literally a punishment to the individual.”
Adams ultimately owed a coinsurance payment of about $4,000 for his new leg, which reflected his portion of the insurer’s negotiated rate for the knee and foot portion of the leg but did not include the costly part that fits around his stump, which didn’t need replacing. The insurer approved the prosthetic leg on appeal, claiming it had made an administrative error, Adams said.
“We’re fortunate that we’re able to afford that 20%,” said Adams, who is a self-employed leadership consultant.
Leah Kaplan doesn’t have that financial flexibility. Born without a left hand, she did not have a prosthetic limb until a few years ago.
Growing up, “I didn’t want more reasons to be stared at,” said Kaplan, 32, of her decision not to use a prosthesis. A few years ago, the cycling enthusiast got a prosthetic hand specially designed for use with her bike. That device was covered under the health plan she has through her county government job in Spokane, Washington, helping developmentally disabled people transition from school to work.
But when she tried to get approval for a prosthetic hand to use for everyday activities, her health plan turned her down. The myoelectric hand she requested would respond to electrical impulses in her arm that would move the hand to perform certain actions. Without insurance coverage, the hand would cost her just over $46,000, which she said she can’t afford.
Working with her doctor, she has appealed the decision to her insurer and been denied three times. Kaplan said she’s still not sure exactly what the rationale is, except that the insurer has questioned the medical necessity of the prosthetic hand. The next step is to file an appeal with an independent review organization certified by the state insurance commissioner’s office.
A prosthetic hand is not a luxury device, Kaplan said. The prosthetic clinic has ordered the hand and made the customized socket that will fit around the end of her arm. But until insurance coverage is sorted out, she can’t use it.
At this point she feels defeated. “I’ve been waiting for this for so long,” Kaplan said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dates vs Raisins – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to raisins, we picked the dates.
Why?
There are benefits for each fruit, but we say dates come out on top. See what you think:
In terms of macros, while they’re both dried fruits, dates contain more water (unless you leave them sitting open for a while), which will tend to mathematically lower the relative percentages of other components because they’re being held against water weight too. However, even though this is the case (i.e. dates are being mathematically disadvantaged), dates contain more than twice the fiber that raisins do (8g/100g compared to raisins’ 3.7g/100g).
While we’re talking macros, dates are also lower in total carbs, as well as obviously net carbs, and have a much lower glycemic index than raisins (dates have a glycemic index of 42, considered low, while raisins have a glycemic index of 64, considered medium; their respective glycemic loads are even more telling: 13 for raisins and just 2 for dates!).
About those carbs… For dates, it’s an approximately equal mix of sucrose, glucose, and fructose, while for raisins it’s 49% glucose and 49% fructose. Because sucrose is the only disaccharide here, this (as well as the fiber difference) is one of the reasons for the different glycemic indices and glycemic loads, since glucose and fructose are more quickly absorbed.
That’s more than we usually write about macros, but in this case, both fruits are ones especially often hit with the “aren’t they full of sugar though?” question, so it was important to cover the critical distinctions between the two, because they really are very different.
Summary of macros: dates win easily in every aspect we looked at
In the category of vitamins, raisins get a tally in their favor. Raisins are higher in vitamins B1, B2, C, E, K, and choline, while dates are higher in vitamins A, B3, B5, and B9, giving raisins a 6:4 lead here. In dates’ defense, the difference in vitamin K is marginal, and it’d make it a 5:4 lead if we considered that within the margin of error (because all these figures are of course based on averages), and the vitamins that dates are higher in, the margins are much wider indeed, meaning that both fruits have approximately the same overall levels of vitamins when looked at in total, but still, we’ll call this category a nominal win for raisins.
When it comes to minerals, dates have more magnesium, selenium, and zinc, while raisins have more copper, iron, phosphorus, and potassium. Nominally that’s a 4:3 lead for raisins, but if we consider that raisins also contain more sodium, it’s more like a tie here. If we have to pick one though, this is a very slight win for raisins.
Adding up the sections, we have one huge win for dates (macros) with two very marginal wins for raisins—hence, we say that dates win out.
Still, of course enjoy both; diversity is good for the health.
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: