How Ibogaine Can Beat Buprenorphine For Beating Addictions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Questions?❞
It seems that this week, everyone was so satisfied with our information, that we received no questions! (If you sent one and we somehow missed it, please accept our apologies and do bring our attention to it)
However, we did receive some expert feedback that we wanted to share because it’s so informative:
❝I work at a detox rehab in Mexico, where we can use methods not legal in the United States. Therefore, while much of the linked articles had useful information, I’m in the “trenches” every day, and there’s some information I’d like to share that you may wish to share, with additional information:
- Buprenorphine is widely used and ineffective for addiction because it’s synthetic and has many adverse side effects. For heavy drug users it isn’t enough and they still hit the streets for more opioid, resulting in fentanyl deaths. Depending on length of usage and dose, it can take WEEKS to get off of, and it’s extremely difficult.
- Ibogaine is the medicine we use to detox people off opiates, alcohol, meth as well as my own specialty, bulimia. It’s psychoactive and it temporarily “resets” the brain to a pre-addictive state. Supplemented by behavior and lifestyle changes, as well as addressing the traumas that led to the addiction is extremely effective.
Our results are about 50%, meaning the client is free of the substance or behavior 1 year later. Ibogaine isn’t a “magic pill” or cure, it’s an opening tool that makes the difficult work of reclaiming one’s life easier.
Ibogaine is not something that should be done outside a medical setting. It requires an EKG to ensure the heart is healthy and doesn’t have prolonged QT intervals; also blood testing to ensure organs are functioning (especially the liver) and mineral levels such as magnetic and potassium are where they should be. It is important that this treatment be conducted by experienced doctors or practitioners, and monitoring vital signs constantly is imperative.
I’m taking time to compose this information because it needs to be shared that there is an option available most people have not heard about.❞
~ 10almonds reader (slightly edited for formatting and privacy)
Thank you for that! Definitely valuable information for people to know, and (if applicable for oneself or perhaps a loved one) ask about when it comes to local options.
We see it’s also being studied for its potential against other neurological conditions, too:
❝The combination of ibogaine and antidepressants produces a synergistic effect in reducing symptoms of psychiatric disorders such as bipolar disorder, depression, schizophrenia, paranoia, anxiety, panic disorder, mania, post-traumatic stress disorder (PTSD), and obsessive–compulsive disorder. Though ibogaine and the antidepressant act in different pathways, together they provide highly efficient therapeutic responses compared to when each of the active agents is used alone.❞
Read more: Ibogaine and Their Analogs as Therapeutics for Neurological and Psychiatric Disorders
For those who missed it, today’s information about ibogaine was in response to our article:
Let’s Get Letting Go (Of These Three Things)
…which in turn referenced our previous main feature:
Which Addiction-Quitting Methods Work Best?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s the difference between vegan and vegetarian?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
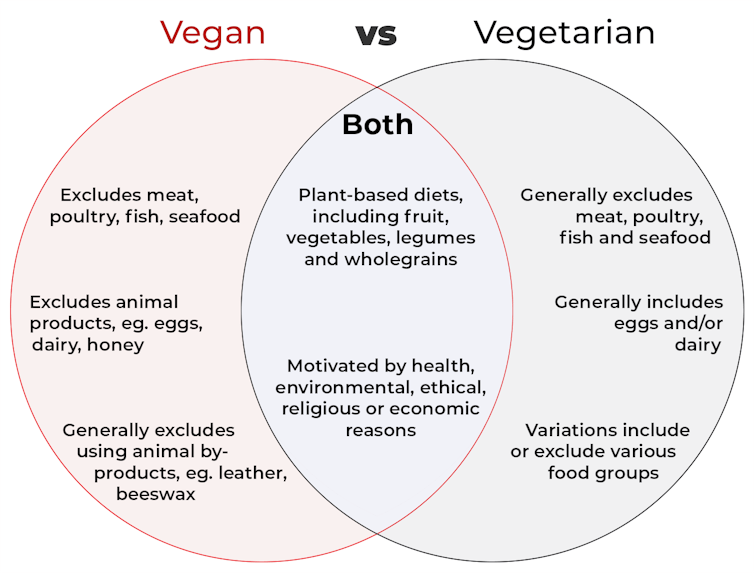
Vegan and vegetarian diets are plant-based diets. Both include plant foods, such as fruits, vegetables, legumes and whole grains.
But there are important differences, and knowing what you can and can’t eat when it comes to a vegan and vegetarian diet can be confusing.
So, what’s the main difference?
Creative Cat Studio/Shutterstock What’s a vegan diet?
A vegan diet is an entirely plant-based diet. It doesn’t include any meat and animal products. So, no meat, poultry, fish, seafood, eggs, dairy or honey.
What’s a vegetarian diet?
A vegetarian diet is a plant-based diet that generally excludes meat, poultry, fish and seafood, but can include animal products. So, unlike a vegan diet, a vegetarian diet can include eggs, dairy and honey.
But you may be wondering why you’ve heard of vegetarians who eat fish, vegetarians who don’t eat eggs, vegetarians who don’t eat dairy, and even vegetarians who eat some meat. Well, it’s because there are variations on a vegetarian diet:
- a lacto-ovo vegetarian diet excludes meat, poultry, fish and seafood, but includes eggs, dairy and honey
- an ovo-vegetarian diet excludes meat, poultry, fish, seafood and dairy, but includes eggs and honey
- a lacto-vegetarian diet excludes meat, poultry, fish, seafood and eggs, but includes dairy and honey
- a pescatarian diet excludes meat and poultry, but includes eggs, dairy, honey, fish and seafood
- a flexitarian, or semi-vegetarian diet, includes eggs, dairy and honey and may include small amounts of meat, poultry, fish and seafood.
Are these diets healthy?
A 2023 review looked at the health effects of vegetarian and vegan diets from two types of study.
Observational studies followed people over the years to see how their diets were linked to their health. In these studies, eating a vegetarian diet was associated with a lower risk of developing cardiovascular disease (such as heart disease or a stroke), diabetes, hypertension (high blood pressure), dementia and cancer.
For example, in a study of 44,561 participants, the risk of heart disease was 32% lower in vegetarians than non-vegetarians after an average follow-up of nearly 12 years.
Further evidence came from randomised controlled trials. These instruct study participants to eat a specific diet for a specific period of time and monitor their health throughout. These studies showed eating a vegetarian or vegan diet led to reductions in weight, blood pressure, and levels of unhealthy cholesterol.
For example, one analysis combined data from seven randomised controlled trials. This so-called meta-analysis included data from 311 participants. It showed eating a vegetarian diet was associated with a systolic blood pressure (the first number in your blood pressure reading) an average 5 mmHg lower compared with non-vegetarian diets.
It seems vegetarian diets are more likely to be healthier, across a number of measures.
For example, a 2022 meta-analysis combined the results of several observational studies. It concluded a vegetarian diet, rather than vegan diet, was recommended to prevent heart disease.
There is also evidence vegans are more likely to have bone fractures than vegetarians. This could be partly due to a lower body-mass index and a lower intake of nutrients such as calcium, vitamin D and protein.
But it can be about more than just food
Many vegans, where possible, do not use products that directly or indirectly involve using animals.
So vegans would not wear leather, wool or silk clothing, for example. And they would not use soaps or candles made from beeswax, or use products tested on animals.
The motivation for following a vegan or vegetarian diet can vary from person to person. Common motivations include health, environmental, ethical, religious or economic reasons.
And for many people who follow a vegan or vegetarian diet, this forms a central part of their identity.
More than a diet: veganism can form part of someone’s identity. Shutterstock So, should I adopt a vegan or vegetarian diet?
If you are thinking about a vegan or vegetarian diet, here are some things to consider:
- eating more plant foods does not automatically mean you are eating a healthier diet. Hot chips, biscuits and soft drinks can all be vegan or vegetarian foods. And many plant-based alternatives, such as plant-based sausages, can be high in added salt
- meeting the nutrient intake targets for vitamin B12, iron, calcium, and iodine requires more careful planning while on a vegan or vegetarian diet. This is because meat, seafood and animal products are good sources of these vitamins and minerals
- eating a plant-based diet doesn’t necessarily mean excluding all meat and animal products. A healthy flexitarian diet prioritises eating more whole plant-foods, such as vegetables and beans, and less processed meat, such as bacon and sausages
- the Australian Dietary Guidelines recommend eating a wide variety of foods from the five food groups (fruit, vegetables, cereals, lean meat and/or their alternatives and reduced-fat dairy products and/or their alternatives). So if you are eating animal products, choose lean, reduced-fat meats and dairy products and limit processed meats.
Katherine Livingstone, NHMRC Emerging Leadership Fellow and Senior Research Fellow at the Institute for Physical Activity and Nutrition, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Teen Daily Delivery Requested
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I thoroughly enjoy your daily delivery. I’d love to see one for teens too!
That’s great to hear! The average age of our subscribers is generally rather older, but it’s good to know there’s an interest in topics for younger people. We’ll bear that in mind, and see what we can do to cater to that without alienating our older readers!
That said: it’s never too soon to be learning about stuff that affects us when we’re older—there are lifestyle factors at 20 that affect Alzheimer’s risk at 60, for example (e.g. drinking—excessive drinking at 20* is correlated to higher Alzheimer’s risk at 60).
*This one may be less of an issue for our US readers, since the US doesn’t have nearly as much of a culture of drinking under 21 as some places. Compare for example with general European practices of drinking moderately from the mid-teens, or the (happily, diminishing—but historically notable) British practice of drinking heavily from the mid-teens.
Share This Post
-
53 Studies Later: The Best Way to Improve VO2 Max
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
VO2 max measures maximum oxygen usage during intense exercise and reflects overall health and performance. To have a high VO2 max, efficient functioning of lungs, heart, red blood cells, muscles, and mitochondria is crucial. So, how to get those?
Let’s HIIT it!
High-Intensity Interval Training (HIIT) outperforms moderate-intensity exercise, by a long way. Further, based on the data from the 53 studies mentioned in the title, we can know which of the protocols tested work best, and they are:
- 15×15 Interval Training: 15 seconds sprint (90–95% max heart rate) + 15 seconds active rest (70% max heart rate), repeated 47 times.
- 4×4 Interval Training: 4 minutes sprint (90–95% max heart rate) + 3 minutes active rest (70% max heart rate), repeated 4 times.
Whichever you choose, it is best to then do that 3x per week.
Note that “sprint” can mean any maximum-effort cardio exercise; it doesn’t have to be running specifically. Cycling or swimming, for example, are fine options too, as is jumping rope.
For more on each of these, plus how the science got there, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Do HIIT (Without Wrecking Your Body)
Take care!
Share This Post
Related Posts
-
Simple, 10-Minute Hip Opening Routine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hips Feeling Stiff?
If so, Flow with Adee’s video (below) has just the solution with a quick 10-minute hip-opening routine. Designed for intermediates but open to all, we love Adee’s work and recommend that you reach out to her to tell her what you’d like to see next.
Other Methods
If you’re a book lover, we’ve reviewed a fantastic book on reducing hip pain. Alternatively, learn stretching from a ballerina with Jasmine McDonald’s ballet stretching routine.
Otherwise, enjoy today’s video:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Early Detection May Help Kentucky Tamp Down Its Lung Cancer Crisis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anthony Stumbo’s heart sank after the doctor shared his mother’s chest X-ray.
“I remember that drive home, bringing her back home, and we basically cried,” said the internal medicine physician, who had started practicing in eastern Kentucky near his childhood home shortly before his mother began feeling ill. “Nobody wants to get told they’ve got inoperable lung cancer. I cried because I knew what this meant for her.”
Now Stumbo, whose mother died the following year, in 1997, is among a group of Kentucky clinicians and researchers determined to rewrite the script for other families by promoting training and boosting awareness about early detection in the state with the highest lung cancer death rate. For the past decade, Kentucky researchers have promoted lung cancer screening, first recommended by the U.S. Preventive Services Task Force in 2013. These days the Bluegrass State screens more residents who are at high risk of developing lung cancer than any state except Massachusetts — 10.6% of eligible residents in 2022, more than double the national rate of 4.5% — according to the most recent American Lung Association analysis.
The effort has been driven by a research initiative called the Kentucky LEADS (Lung Cancer Education, Awareness, Detection, and Survivorship) Collaborative, which in 2014 launched to improve screening and prevention, to identify more tumors earlier, when survival odds are far better. The group has worked with clinicians and hospital administrators statewide to boost screening rates both in urban areas and regions far removed from academic medical centers, such as rural Appalachia. But, a decade into the program, the researchers face an ongoing challenge as they encourage more people to get tested, namely the fear and stigma that swirl around smoking and lung cancer.
Lung cancer kills more Americans than any other malignancy, and the death rates are worst in a swath of states including Kentucky and its neighbors Tennessee and West Virginia, and stretching south to Mississippi and Louisiana, according to data from the Centers for Disease Control and Prevention.
It’s a bit early to see the impact on lung cancer deaths because people may still live for years with a malignancy, LEADS researchers said. Plus, treatment improvements and other factors may also help reduce death rates along with increased screening. Still, data already shows that more cancers in Kentucky are being detected before they become advanced, and thus more difficult to treat, they said. Of total lung cancer cases statewide, the percentage of advanced cases — defined as cancers that had spread to the lymph nodes or beyond — hovered near 81% between 2000 and 2014, according to Kentucky Cancer Registry data. By 2020, that number had declined to 72%, according to the most recent data available.
“We are changing the story of families. And there is hope where there has not been hope before,” said Jennifer Knight, a LEADS principal investigator.
Older adults in their 60s and 70s can hold a particularly bleak view of their mortality odds, given what their loved ones experienced before screening became available, said Ashley Shemwell, a nurse navigator for the lung cancer screening program at Owensboro Health, a nonprofit health system that serves Kentucky and Indiana.
“A lot of them will say, ‘It doesn’t matter if I get lung cancer or not because it’s going to kill me. So I don’t want to know,’” said Shemwell. “With that generation, they saw a lot of lung cancers and a lot of deaths. And it was terrible deaths because they were stage 4 lung cancers.” But she reminds them that lung cancer is much more treatable if caught before it spreads.
The collaborative works with several partners, including the University of Kentucky, the University of Louisville, and GO2 for Lung Cancer, and has received grant funding from the Bristol Myers Squibb Foundation. Leaders have provided training and other support to 10 hospital-based screening programs, including a stipend to pay for resources such as educational materials or a nurse navigator, Knight said. In 2022, state lawmakers established a statewide lung cancer screening program based in part on the group’s work.
Jacob Sands, a lung cancer physician at Boston’s Dana-Farber Cancer Institute, credits the LEADS collaborative with encouraging patients to return for annual screening and follow-up testing for any suspicious nodules. “What the Kentucky LEADS program is doing is fantastic, and that is how you really move the needle in implementing lung screening on a larger scale,” said Sands, who isn’t affiliated with the Kentucky program and serves as a volunteer spokesperson for the American Lung Association.
In 2014, Kentucky expanded Medicaid, increasing the number of lower-income people who qualified for lung cancer screening and any related treatment. Adults 50 to 80 years old are advised to get a CT scan every year if they have accumulated at least 20 pack years and still smoke or have quit within the past 15 years, according to the latest task force recommendation, which widened the pool of eligible adults. (To calculate pack years, multiply the packs of cigarettes smoked daily by years of smoking.) The lung association offers an online quiz, called “Saved By The Scan,” to figure out likely eligibility for insurance coverage.
Half of U.S. patients aren’t diagnosed until their cancer has spread beyond the lungs and lymph nodes to elsewhere in the body. By then, the five-year survival rate is 8.2%.
But regular screening boosts those odds. When a CT scan detects lung cancer early, patients have an 81% chance of living at least 20 years, according to data published in November in the journal Radiology.
Some adults, like Lisa Ayers, didn’t realize lung cancer screening was an option. Her family doctor recommended a CT scan last year after she reported breathing difficulties. Ayers, who lives in Ohio near the Kentucky border, got screened at UK King’s Daughters, a hospital in far eastern Kentucky. The scan didn’t take much time, and she didn’t have to undress, the 57-year-old said. “It took me longer to park,” she quipped.
She was diagnosed with a lung carcinoid tumor, a type of neuroendocrine cancer that can grow in various parts of the body. Her cancer was considered too risky for surgery, Ayers said. A biopsy showed the cancer was slow-growing, and her doctors said they would monitor it closely.
Ayers, a lifelong smoker, recalled her doctor said that her type of cancer isn’t typically linked to smoking. But she quit anyway, feeling like she’d been given a second chance to avoid developing a smoking-related cancer. “It was a big wake-up call for me.”
Adults with a smoking history often report being treated poorly by medical professionals, said Jamie Studts, a health psychologist and a LEADS principal investigator, who has been involved with the research from the start. The goal is to avoid stigmatizing people and instead to build rapport, meeting them where they are that day, he said.
“If someone tells us that they’re not ready to quit smoking but they want to have lung cancer screening, awesome; we’d love to help,” Studts said. “You know what? You actually develop a relationship with an individual by accepting, ‘No.’”
Nationally, screening rates vary widely. Massachusetts reaches 11.9% of eligible residents, while California ranks last, screening just 0.7%, according to the lung association analysis.
That data likely doesn’t capture all California screenings, as it may not include CT scans done through large managed care organizations, said Raquel Arias, a Los Angeles-based associate director of state partnerships at the American Cancer Society. She cited other 2022 data for California, looking at lung cancer screening for eligible Medicare fee-for-service patients, which found a screening rate of 1%-2% in that population.
But, Arias said, the state’s effort is “nowhere near what it needs to be.”
The low smoking rate in California, along with its image as a healthy state, “seems to have come with the unintended consequence of further stigmatizing people who smoke,” said Arias, citing one of the findings from a 2022 report looking at lung cancer screening barriers. For instance, eligible patients may be reluctant to share prior smoking habits with their health provider, she said.
Meanwhile, Kentucky screening efforts progress, scan by scan.
At Appalachian Regional Healthcare, 3,071 patients were screened in 2023, compared with 372 in 2017. “We’re just scratching the surface of the potential lives that we can have an effect on,” said Stumbo, a lung cancer screening champion at the health system, which includes 14 hospitals, most located in eastern Kentucky.
The doctor hasn’t shed his own grief about what his family missed after his mother died at age 51, long before annual screening was recommended. “Knowing that my children were born, and never knowing their grandmother,” he said, “just how sad is that?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Escape From The Clutches Of Shame
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about managing various emotions, including “negative” ones. We put that in “scare quotes” because they also all have positive aspects, that are just generally overshadowed by the fact that the emotions themselves are not pleasant. But for example…
We evolved our emotions, including the “negative” ones, for our own benefit as a species:
- Stress keeps us safe by making sure we take important situations seriously
- Anger keeps us safe by protecting us from threats
- Disgust keeps us safe by helping us to avoid things that might cause disease
- Anxiety keeps us safe by ensuring we don’t get complacent
- Guilt keeps us safe by ensuring we can function as a community
- Sadness keeps us safe by ensuring we value things that are important to us, and learn to become averse to losing them
- …and so on
You can read more about how to turn these off (or rather, at least pause them) when they’re misfiring and/or just plain not convenient, here:
While it’s generally considered good to process feelings instead of putting them aside, the fact is that sometimes we have to hold it together while we do something, such that we can later have an emotional breakdown at a convenient time and place, instead of the supermarket or bank or office or airport or while entertaining houseguests or… etc.
Today, though, we’re not putting things aside, for the most part (though we will get to that too).
We’ll be dealing with shame, which is closely linked to the guilt we mentioned in that list there.
See also: Reconsidering the Differences Between Shame and Guilt
Shame’s purpose
Shame’s purpose is to help us (as a community) avoid anti-social behavior for which we might be shamed, and thus exiled from the in-group. It helps us all function better together, which is how we thrive as a species.
Shame, therefore, is often assumed to be something we can (and possibly should) use to ensure that we (ourselves and/or others) “do the right thing”.
But there’s a catch…
Shame only works negatively
You may be thinking “well duh, it’s a negative emotion”, but this isn’t about negativity in the subjective sense, but rather, positive vs negative motivation:
- Positive motivation: motivation that encourages us to do a given thing
- Negative motivation: motivation that encourages us to specifically not do a given thing
Shame is only useful as a negative motivation, i.e., encouraging us to specifically not do a given thing.
Examples:
- You cannot (in any way that sticks, at least) shame somebody into doing more housework.
- You can, however, shame somebody out of drinking and driving.
This distinction matters a lot when it comes to how we are with our children, or with our employees (or those placed under us in a management structure), or with people who otherwise look to us as leaders.
It also matters when it comes to how we are with ourselves.
Here’s a paper about this, by the way, with assorted real-world examples:
The negative side of motivation: the role of shame
From those examples, we can see that attempts to shame someone (including oneself) into doing something positive will generally not only fail, they will actively backfire, and people (including oneself) will often perform worse than pre-shaming.
Looking inwards: healthy vs unhealthy shame
Alcoholics Anonymous and similar programs use a degree of pro-social shame to help members abstain from the the act being shamed.
Rather than the unhelpful shame of exiling a person from a group for doing a shameful thing, however, they take an approach of laying out the shame for all to see, feeling the worst of it and moving past it, which many report as being quite freeing emotionally while still [negatively] motivational to not use the substance in question in the future (and similar for activity-based addictions/compulsions, such as gambling, for example).
As such, if you are trying to avoid doing a thing, shame can be a useful motivator. So by all means, if it’s appropriate to your goals, tell your friends/family about how you are now quitting this or that (be it an addiction, or just something generally unhealthy that you’d like to strike off your regular consumption/activity list).
You will still be tempted! But the knowledge of the shame you would feel as a result will help keep you from straying into that temptation.
If you are trying to do a thing, however, (even something thought of in a negative frame, such as “lose weight”), then shame is not helpful and you will do best to set it aside.
You can shame yourself out of drinking sodas (if that’s your plan), but you can’t shame yourself into eating healthy meals. And even if your plan is just shaming yourself out of eating unhealthy food… Without a clear active positive replacement to focus on instead, all you’ll do there is give yourself an eating disorder. You’ll eat nothing when people are looking, and then either a) also eat next to nothing in private or else b) binge in secret, and feel terrible about yourself, neither of which are any good for you whatsoever.
Similarly, you can shame yourself out of bed, but you can’t shame yourself into the gym:
Let it go
There are some cases, especially those where shame has a large crossover with guilt, that it serves no purpose whatsoever, and is best processed and then put aside.
For example, if you did something that you are ashamed of many years ago, and/or feel guilty about something that you did many years ago, but this is not an ongoing thing for you (i.e., it was a one-off bad decision, or a bad habit that have now long since dropped), then feeling shame and/or guilt about that does not benefit you or anyone else.
As to how to process it and put it aside, if your thing harmed someone else, you could see if there’s a way to try to make amends (even if without confessing ill, such as by acting anonymously to benefit the person/group you harmed).
And then, forgive yourself. Regardless of whether you feel like you deserve it. Make the useful choice, that better benefits you, and by extension those around you.
If you are religious, you may find that of help here too. We’re a health science publication not a theological one, but for example: Buddhism preaches compassion including for oneself. Judaism preaches atonement. Christianity, absolution. For Islam, mercy is one of the holiest ideals of the religion, along with forgiveness. So while religion isn’t everyone’s thing, for those for whom it is, it can be an asset in this regard.
For a more worldly approach:
To Err Is Human; To Forgive, Healthy (Here’s How To Do It) ← this goes for when the forgiveness in question is for yourself, too—and we do write about that there (and how)!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: