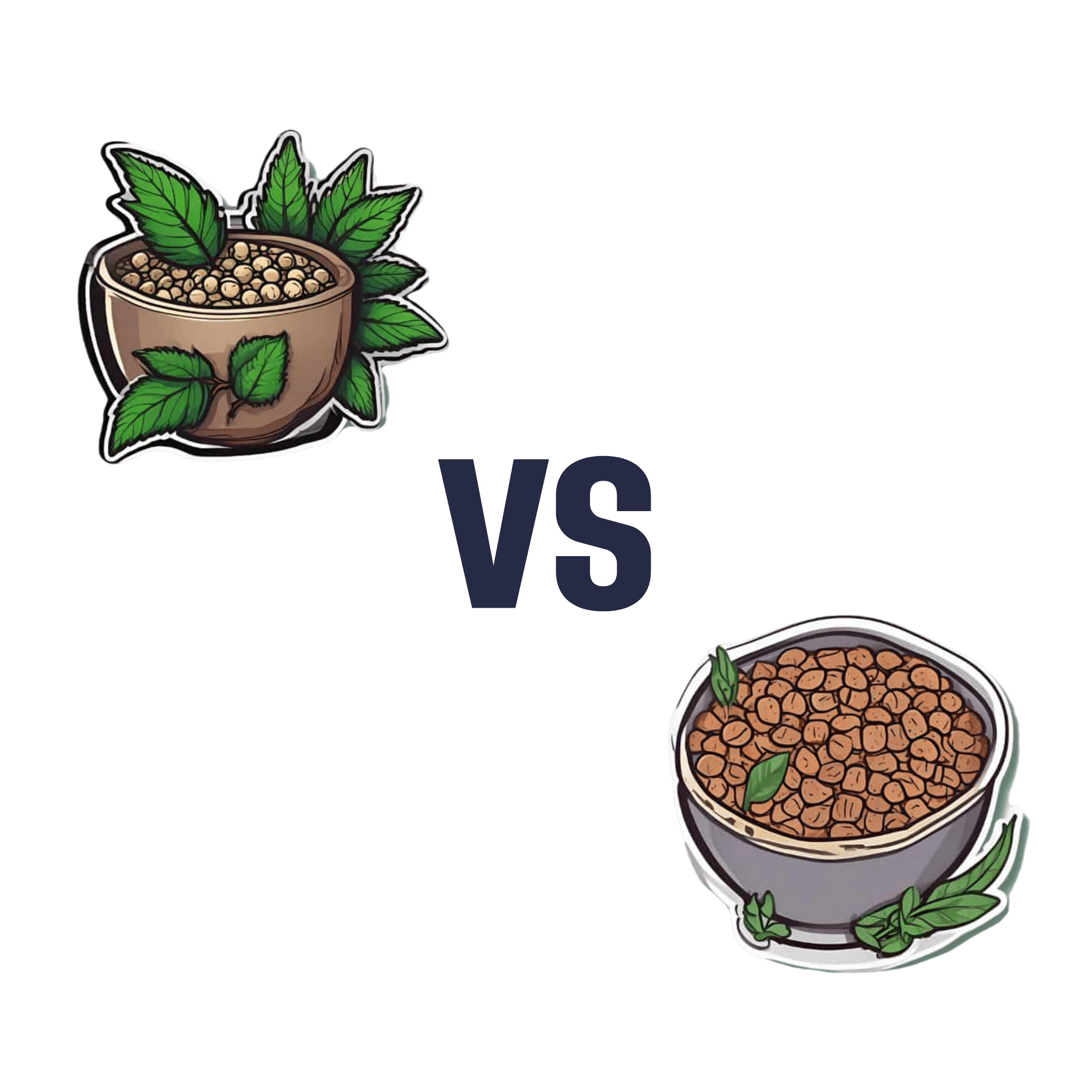
Hemp Seeds vs Flax Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hemp seeds to flax seeds, we picked the flax.
Why?
Both are great, but quite differently so! In other words, they both have their advantages, but on balance, we prefer the flax’s advantages.
Part of this come from the way in which they are sold/consumed—hemp seeds must be hulled first, which means two things as a result:
- Flax seeds have much more fiber (about 8x more)
- Hemp seeds have more protein (about 2x more), proportionally, at least ← this is partly because they lost a bunch of weight by losing their fiber to the hulling, so the “per 100g” values of everything else go up, even though the amount per seed didn’t change
Since people’s diets are more commonly deficient in fiber than protein, and also since 8x is better than 2x, we consider this a win for flax.
Of course, many people enjoy hemp or flax specifically for the healthy fatty acids, so how do they stack up in that regard?
- Flax seeds have more omega-3s
- Hemp seeds have more omega-6s
This, for us, is a win for flax too, as the omega-3s are generally what we need more likely to be deficient in. Hemp enthusiasts, however, may argue that the internal balance of omega-3s to omega-6s is closer to an ideal ratio in hemp—but nutrition doesn’t exist in a vacuum, so we have to consider things “as part of a balanced diet” (because if one were trying to just live on hemp seeds, one would die), and most people’s diets are skewed far too far in favor or omega-6 compared to omega-3. So for most people, the higher levels of omega-3s are the more useful.
Want to learn more?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s the difference between ‘strep throat’ and a sore throat? We’re developing a vaccine for one of them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
It’s the time of the year for coughs, colds and sore throats. So you might have heard people talk about having a “strep throat”.
But what is that? Is it just a bad sore throat that goes away by itself in a day or two? Should you be worried?
Here’s what we know about the similarities and differences between strep throat and a sore throat, and why they matter.
Prostock-studio/Shutterstock How are they similar?
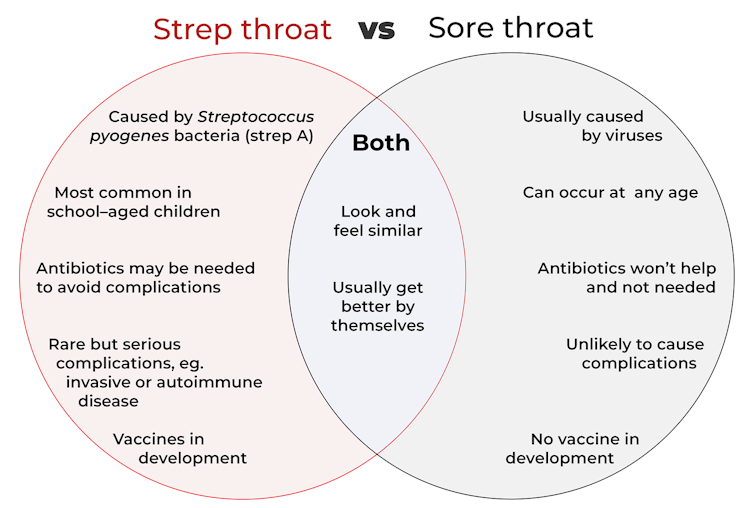
It’s difficult to tell the difference between a sore throat and strep throat as they look and feel similar.
People usually have a fever, a bright red throat and sometimes painful lumps in the neck (swollen lymph nodes). A throat swab can help diagnose strep throat, but the results can take a few days.
Thankfully, both types of sore throat usually get better by themselves.
How are they different?
Most sore throats are caused by viruses such as common cold viruses, the flu (influenza virus), or the virus that causes glandular fever (Epstein-Barr virus).
These viral sore throats can occur at any age. Antibiotics don’t work against viruses so if you have a viral sore throat, you won’t get better faster if you take antibiotics. You might even have some unwanted antibiotic side-effects.
But strep throat is caused by Streptococcus pyogenes bacteria, also known as strep A. Strep throat is most common in school-aged children, but can affect other age groups. In some cases, you may need antibiotics to avoid some rare but serious complications.
In fact, the potential for complications is one key difference between a viral sore throat and strep throat.
Generally, a viral sore throat is very unlikely to cause complications (one exception is those caused by Epstein-Barr virus which has been associated with illnesses such as chronic fatigue syndrome, multiple sclerosis and certain cancers).
But strep A can cause invasive disease, a rare but serious complication. This is when bacteria living somewhere on the body (usually the skin or throat) get into another part of the body where there shouldn’t be bacteria, such as the bloodstream. This can make people extremely sick.
Invasive strep A infections and deaths have been rising in recent years around the world, especially in young children and older adults. This may be due to a number of factors such as increased social mixing at this stage of the COVID pandemic and an increase in circulating common cold viruses. But overall the reasons behind the increase in invasive strep A infections are not clear.
Another rare but serious side effect of strep A is autoimmune disease. This is when the body’s immune system makes antibodies that react against its own cells.
The most common example is rheumatic heart disease. This is when the body’s immune system damages the heart valves a few weeks or months after a strep throat or skin infection.
Around the world more than 40 million people live with rheumatic heart disease and more than 300,000 die from its complications every year, mostly in developing countries.
However, parts of Australia have some of the highest rates of rheumatic heart disease in the world. More than 5,300 Indigenous Australians live with it.
Strep throat is caused by Streptococcus bacteria and can be treated with antibiotics if needed. Kateryna Kon/Shutterstock Why do some people get sicker than others?
We know strep A infections and rheumatic heart disease are more common in low socioeconomic communities where poverty and overcrowding lead to increased strep A transmission and disease.
However, we don’t fully understand why some people only get a mild infection with strep throat while others get very sick with invasive disease.
We also don’t understand why some people get rheumatic heart disease after strep A infections when most others don’t. Our research team is trying to find out.
How about a vaccine for strep A?
There is no strep A vaccine but many groups in Australia, New Zealand and worldwide are working towards one.
For instance, Murdoch Children’s Research Institute and Telethon Kids Institute have formed the Australian Strep A Vaccine Initiative to develop strep A vaccines. There’s also a global consortium working towards the same goal.
Companies such as Vaxcyte and GlaxoSmithKline have also been developing strep A vaccines.
What if I have a sore throat?
Most sore throats will get better by themselves. But if yours doesn’t get better in a few days or you have ongoing fever, see your GP.
Your GP can examine you, consider running some tests and help you decide if you need antibiotics.
Kim Davis, General paediatrician and paediatric infectious diseases specialist, Murdoch Children’s Research Institute; Alma Fulurija, Immunologist and the Australian Strep A Vaccine Initiative project lead, Telethon Kids Institute, and Myra Hardy, Postdoctoral Researcher, Infection, Immunity and Global Health, Murdoch Children’s Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How To Avoid Carer Burnout (Without Dropping Care)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Avoid Carer Burnout
Sometimes in life we find ourselves in a caregiving role.
Maybe we chose it. For example, by becoming a professional carer, or even just by being a parent.
Oftentimes we didn’t. Sometimes because our own parents now need care from us, or because a partner becomes disabled.
Philosophical note: an argument could be made for that latter also having been a pre-emptive choice; we probably at some point said words to the effect of “in sickness and in health”, hopefully with free will, and hopefully meant it. And of course, sometimes we enter into a relationship with someone who is already disabled.
But, we are not a philosophy publication, and will henceforth keep to the practicalities.
First: are you the right person?
Sometimes, a caregiving role might fall upon you unasked-for, and it’s worth considering whether you are really up for it. Are you in a position to be that caregiver? Do you want to be that caregiver?
It may be that you do, and would actively fight off anyone or anything that tried to stop you. If so, great, now you only need to make sure that you are actually in a position to provide the care in question.
It may be that you do want to, but your circumstances don’t allow you to do as good a job of it as you’d like, or it means you have to drop other responsibilities, or you need extra help. We’ll cover these things later.
It may be that you don’t want to, but you feel obliged, or “have to”. If that’s the case, it will be better for everyone if you acknowledge that, and find someone else to do it. Nobody wants to feel a burden, and nobody wants someone providing care to be resentful of that. The result of such is two people being miserable; that’s not good for anyone. Better to give the job to someone who actually wants to (a professional, if necessary).
So, be honest (first with yourself, then with whoever may be necessary) about your own preferences and situation, and take steps to ensure you’re only in a caregiving role that you have the means and the will to provide.
Second: are you out of your depth?
Some people have had a life that’s prepared them for being a carer. Maybe they worked in the caring profession, maybe they have always been the family caregiver for one reason or another.
Yet, even if that describes you… Sometimes someone’s care needs may be beyond your abilities. After all, not all care needs are equal, and someone’s condition can (and more often than not, will) deteriorate.
So, learn. Learn about the person’s condition(s), medications, medical equipment, etc. If you can, take courses and such. The more you invest in your own development in this regard, the more easily you will handle the care, and the less it will take out of you.
And, don’t be afraid to ask for help. Maybe the person knows their condition better than you, and certainly there’s a good chance they know their care needs best. And certainly, there are always professionals that can be contacted to ask for advice.
Sometimes, a team effort may be required, and there’s no shame in that either. Whether it means enlisting help from family/friends or professionals, sometimes “many hands make light work”.
Check out: Caregiver Action Network: Organizations Near Me
A very good resource-hub for help, advice, & community
Third: put your own oxygen mask on first
Like the advice to put on one’s own oxygen mask first before helping others (in the event of a cabin depressurization in an airplane), the rationale is the same here. You can’t help others if you are running on empty yourself.
As a carer, sometimes you may have to put someone else’s needs above yours, both in general and in the moment. But, you do have needs too, and cannot neglect them (for long).
One sleepless night looking after someone else is… a small sacrifice for a loved one, perhaps. But several in a row starts to become unsustainable.
Sometimes it will be necessary to do the best you can, and accept that you cannot do everything all the time.
There’s a saying amongst engineers that applies here too: “if you don’t schedule time for maintenance, your equipment will schedule it for you”.
In other words: if you don’t give your body rest, your body will break down and oblige you to rest. Please be aware this goes for mental effort too; your brain is just another organ.
So, plan ahead, schedule breaks, find someone to take over, set up your cared-for-person with the resources to care for themself as well as possible (do this anyway, of course—independence is generally good so far as it’s possible), and make the time/effort to get you what you need for you. Sleep, distraction, a change of scenery, whatever it may be.
Lastly: what if it’s you?
If you’re reading this and you’re the person who has the higher care needs, then firstly:all strength to you. You have the hardest job here; let’s not forget that.
About that independence: well-intentioned people may forget that, so don’t be afraid to remind them when “I would prefer to do that myself”. Maintaining independence is generally good for the health, even if sometimes it is more work for all concerned than someone else doing it for you. The goal, after all, is your wellbeing, so this shouldn’t be cast aside lightly.
On the flipside: you don’t have to be strong all the time; nobody should.
Being disabled can also be quite isolating (this is probably not a revelation to you), so if you can find community with other people with the same or similar condition(s), even if it’s just online, that can go a very, very long way to making things easier. Both practically, in terms of sharing tips, and psychologically, in terms of just not feeling alone.
See also: How To Beat Loneliness & Isolation
Share This Post
-
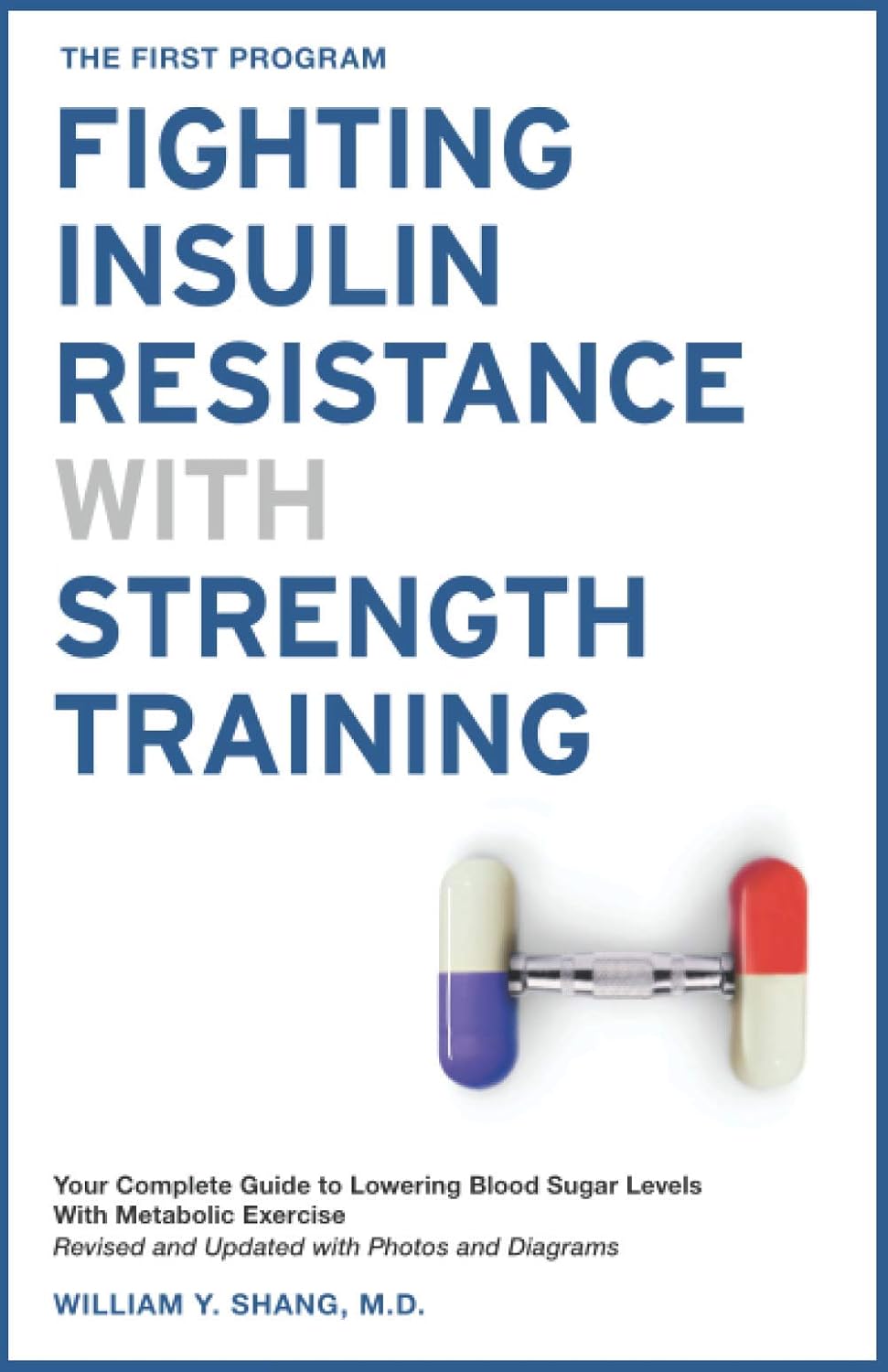
The FIRST Program: Fighting Insulin Resistance with Strength Training – by Dr. William Shang
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of advice about fighting insulin resistance focuses on diet. And, that’s worthwhile! How we eat does make a huge difference to our insulin responses (as does fasting). But, we expect our regular 10almonds readers either know these things now, or can read one of several very good books we’ve already reviewed about such.
This one’s different: it focuses, as the title promises, on fighting insulin resistance with strength training. And why?
It’s because of the difference that our body composition makes to our metabolism. Now, our body fat percentage is often talked about (or, less usefully but more prevalently, even if woefully misleadingly, our BMI), but Dr. Shang makes the case for it being our musculature that has the biggest impact; because of how it hastens our metabolism, and because of how it is much healthier for the body to store glycogen in muscle tissue, than just cramming whatever it can into the liver and visceral fat. It becomes relevant, then, that there’s a limit to how much glycogen can be stored in muscle tissue, and that limit is how much muscle you have.
This is not, however, 243 pages to say “lift some weights, lazybones”. Rather, he explains the relevant pathophysiology (we will be more likely to adhere to things we understand, than things we do not), and gives practical advice on exercising the different kinds of muscle fibers, arguing that the whole is greater than the sum of its parts, as well as outlining an exercise program for the gym, plus a chapter on no-gym exercises too.
The style is quite dense, which may be offputting for some, but it suffices to take one’s time and read thoughtfully; the end result is worth it.
Bottom line: if you’d like to keep insulin resistance at bay, this book is an excellent extra tool for that.
Share This Post
Related Posts
-
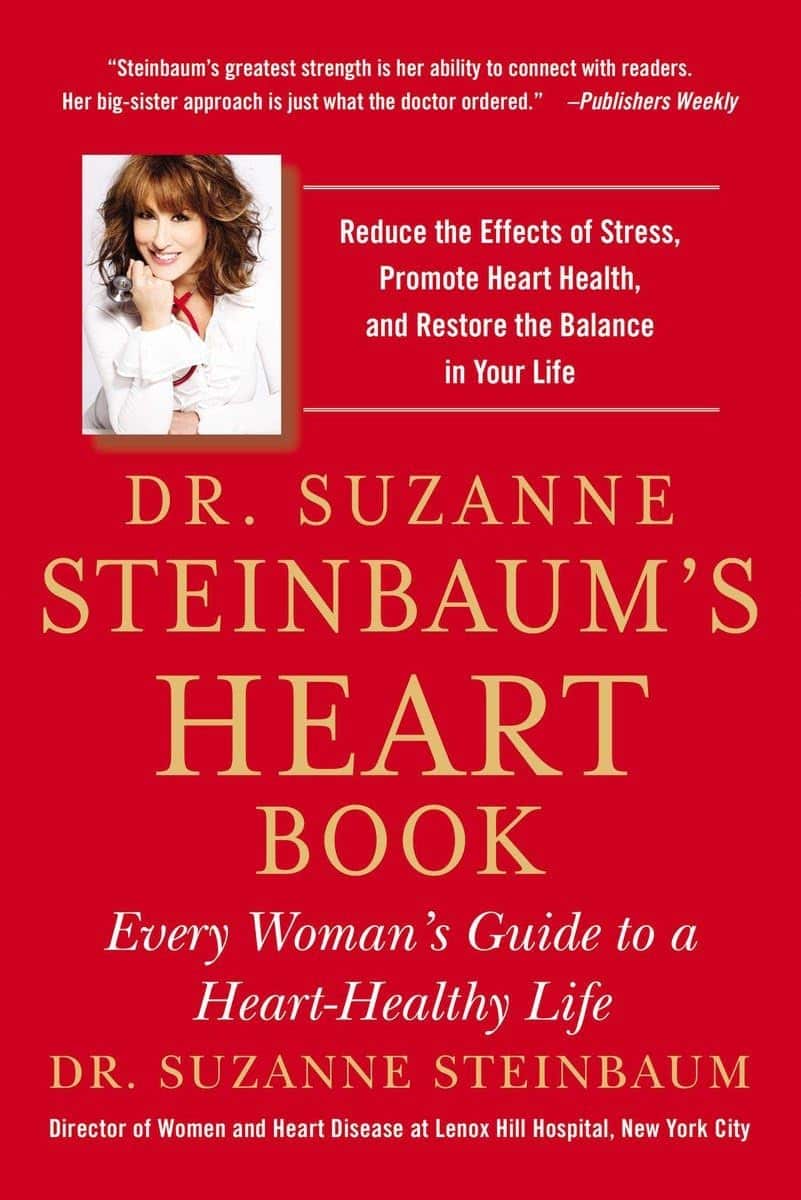
Dr. Suzanne Steinbaum’s Heart Book – by Dr. Suzanne Steinbaum
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book is divided into three parts:
- What you should know
- What you should do
- All about you
This is a very useful format, since it lays out all the foundational knowledge, before offering practical advice and “how to” explanations, before finally wrapping up with personalizing things.
The latter is important, because while our basic risk factors can be assembled in a few lines of data (age, sex, race, genes, diet, exercise habits, etc) there’s a lot more to us than that, and oftentimes the data that doesn’t make the cut, makes the difference. Hormones on high on this list; we can say that a person is a 65-year-old woman and make a guess, but that’s all it is: a guess. Very few of us are the “average person” that statistical models represent accurately. And nor are social and psychological factors irrelevant; in fact often they are deciding factors!
So, it’s important to be able to look at ourselves as the whole persons we are, or else we’ll get a heart-healthy protocol that works on paper but actually falls flat in application, because the mathematical model didn’t take into account that lately we have been very stressed about such-and-such a thing, and deeply anxious about so-and-so, and a hopefully short-term respiratory infection has reduced blood oxygen levels, and all these kinds of things need to be taken into account too, for an overall plan to work.
The greatest strength of this book is that it attends to that.
The style of the book is a little like a long sales pitch (when all that’s being sold, by the way, is the ideas the book is offering; she wants you to take her advice with enthusiasm), but there’s plenty of very good information all the way through, making it quite worth the read.
Bottom line: if you’re a woman and/or love at least one woman, then you can benefit from this important book for understanding heart health that’s not the default.
Click here to check out Dr. Suzanne Steinbaum’s Heart Book, and enjoy a heart-healthy life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Resistance band Training – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those who’d like a full gym workout at home, without splashing out thousands on a home gym, resistance bands provide a lot of value. But how much value, really?
As James Atkinson demonstrates, there’s more exercise available than one might think.
Did you know that you can use the same band to strengthen your triceps as well as your biceps, for instance? and the same goes for your quadriceps and biceps femoris. And core strength? You bet.
The style here is not a sales pitch (though he does, at the end, offer extra resources if desired), but rather, instructional, and this book is in and of itself already a complete guide. With clear instructions and equally clear illustrations, you don’t need to spend a dime more (unless you don’t own a resistance band, in which case then yes, you will need one of those).
Bottom line: if you’d like to give your body the workout it deserves, this book is a potent resource.
Click here to check out Resistance Band Training, and get training!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
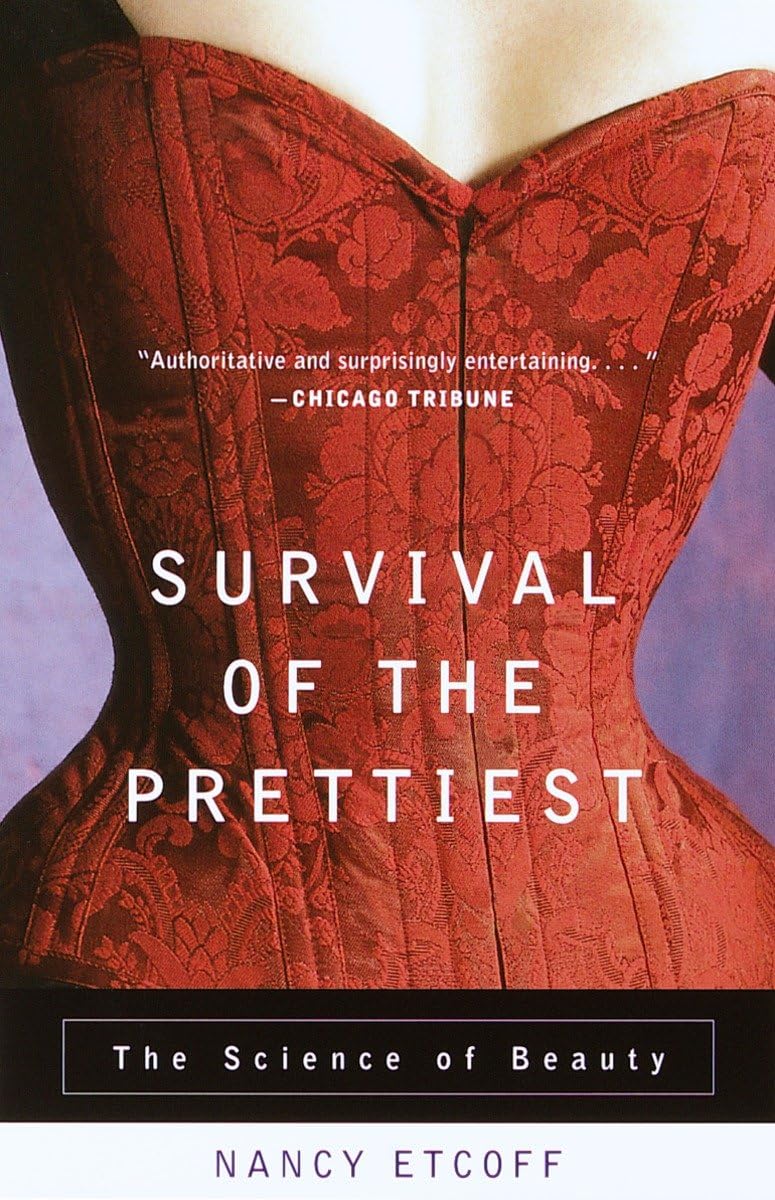
Survival of the Prettiest – by Dr. Nancy Etcoff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beauty is in the eye of the beholder, right? And what does it matter, in this modern world, especially if we are already in a happy stable partnership?
The science of it, as it turns out, is less poetic. Not only is evolutionary psychology still the foundation of our perception of human beauty (yes, even if we have zero possibility of further procreation personally), but also, its effects are far, far wider than partner selection.
From how nice people are to you, to how much they trust you, to how easily they will forgive a (real or perceived) misdeed, to what kind of medical care you get (or don’t), your looks shape your experiences.
In this very easy-reading work that nevertheless contains very many references, Dr. Etcoff explores the science of beauty. Not just what traits are attractive and why, but also, what they will do for (or against) us—in concrete terms, with numbers.
Bottom line: if you’d like to better understand the subconscious biases held by yourself and others, this book is a top-tier primer.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: