Healthy Living in a Contaminated World – by Dr. Donald Hoernschemeyer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot going on here, as this book tackles very many kinds of common contaminants, from waste products and industrial chemicals (such as from fracking), pesticides that are banned in most places but not the US, smog and soot from coal and oil power, mercury and other heavy metals, dioxins, Teflon and its close relatives, phthalates, BPA, and other things again regulated out of use in many countries but not entirely in the US (which bans them only in some things, like baby bottles), drinking water issues of various kinds, and much more.
Indeed, there’s a whole chapter on the US and international regulation of toxic substances; the problem is often that on a political level, the same people who are against nebulous “chemicals” are also against environmentalist regulations that would ban them. This is mostly not a political book though, and rather is chiefly a book of chemistry (the author’s field).
It does also cover the medical maladies associated with various contaminants, while the bulk of the data is on the chemistry side of such things as “elimination times for toxic chemicals”, “amounts of pesticides in fruit and vegetables”, “antibiotics and hormones used in animal agriculture”, and so forth.
The style is dense, and/but it is clear the author has made an effort to not be too dry. Still, this is not a fun read; it’s depressing in content and the style is more suited to academia. There are appendices containing glossaries and acronym tables, but reading front-to-back, there’s a lot that’s not explained so unless you also are a PhD chemist, chances are you’ll be needing to leaf forwards and backwards a lot.
Bottom line: this book is not thrilling, but what you don’t know, can kill you.
Click here to check out Healthy Living In A Contaminated World, and improve your odds!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
To Pee Or Not To Pee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is it “strengthening” to hold, or are we doing ourselves harm if we do? Dr. Heba Shaheed explains in this short video:
A flood of reasons not to hold
Humans should urinate 4–6 times daily, but for many people, the demands of modern life often lead to delaying urination, raising questions about its effects on the body.
So first, let’s look at how it all works: the bladder is part of the urinary system, which includes the kidneys, ureters, urethra, and sphincters. Urine is produced by the kidneys and transported via the ureters into the bladder, a hollow organ with a muscular wall. This muscle (called the detrusor) allows the bladder to inflate as it fills with urine (bearing in mind, the main job of any muscle is to be able to stretch and contract).
As the bladder fills, stretch receptors in that muscle signal fullness to the spinal cord. This triggers the micturition reflex, causing the detrusor to contract and the internal urethral sphincter to open involuntarily. Voluntary control over the external urethral sphincter allows a person to delay or release urine as needed.
So, at what point is it best to go forth and pee?
For most people, bladder fullness is first noticeable at around 150-200ml, with discomfort occurring at 400-500ml (that’s about two cups*). Although the bladder can stretch to hold up to a liter, exceeding this capacity can cause it to rupture, a rare but serious condition requiring surgical intervention.
*note, however, that this doesn’t necessarily mean that drinking two cups will result in two cups being in your bladder; that’s not how hydration works. Unless you are already perfectly hydrated, most if not all of the water will be absorbed into the rest of your body where it is needed. Your bladder gets filled when your body has waste products to dispose of that way, and/or is overhydrated (though overhydration is not very common).
Habitually holding urine and/or urinating too quickly (note: not “too soon”, but literally, “too quickly”, we’re talking about the velocity at which it exits the body) can weaken pelvic floor muscles over time. This can lead to bladder pain, urgency, incontinence, and/or a damaged pelvic floor.
In short: while the body’s systems are equipped to handle occasional delays, holding it regularly is not advisable. For the good of your long-term urinary health, it’s best to avoid straining the system and go whenever you feel the urge.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Keeping your kidneys happy: it’s more than just hydration!
Take care!
Share This Post
-
Cold Weather Health Risks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many Are Cold; Few Are Frozen
Many of those of us in the Northern Hemisphere are getting hit with a cold spell around now. How severe that may be depends on more precisely where we are, but it’s affecting a lot of people. So, with apologies to our readers in Australia, we’re going to do a special on that today.
Acute cold is, for most people, good for the health:
A Cold Shower A Day Keeps The Doctor Away?
Persistent cold, not so much. Let’s look at the risks, and what can be done about them…
Hypothermia
It kills. Don’t let it kill you or your loved ones.
And, this is really important: it doesn’t care whether you’re on a mountain or not.
In other words: a lot of people understand (correctly!) that hypothermia is a big risk to hikers, climbers, and the like. But if the heating goes out in your house and the temperature drops for long enough before the heating is fixed, you can get hypothermia there too just the same if you’re not careful.
How cold is too cold? It doesn’t even have to be sub-zero. According to the CDC, temperatures of 4℃ (40℉) can be low enough to cause hypothermia if other factors combine:
CDC | Prevent Hypothermia & Frostbite ← you can also see the list of symptoms to watch out for, there!
Skin health
Not generally an existential risk, but we may as well stay healthy as not!
Cold air often means dry air, so use a moisturizer with an oil base (if you don’t care for fancy beauty products, ordinary coconut oil is top-tier).
Bonus if you do it after a warming bath/shower!
Heart health
Cold has a vasconstricting effect; that is to say, it causes the body’s vasculature to shrink, increasing localized blood pressure. If it’s a cold shower as above, that can be very invigorating. If it’s a week of sub-zero temperatures, it can become a problem.
❝Shoveling a little snow off your sidewalk may not seem like hard work. However, […] combined with the fact that the exposure to cold air can constrict blood vessels throughout the body, you’re asking your heart to do a lot more work in conditions that are diminishing the heart’s ability to function at its best.❞
Source: Snow shoveling, cold temperatures combine for perfect storm of heart health hazards
If you have a heart condition, please do not shovel snow. Let someone else do it, or stay put.
And if you are normally able to exercise safely? Unless you’re sure your heart is in good order, exercising in the warmth, not the cold, seems to be the best bet.
See also: Heart Attack: His & Hers (Be Prepared!) ← can you remember which symptoms are for which sex? If not, now’s a good time to refresh that knowledge.
Immune health
We recently discussed how cold weather indirectly increases the risk of respiratory viral infection:
The Cold Truth About Respiratory Infections
So, now’s the time to be extra on-guard about that.
See also: Beyond Supplements: The Real Immune-Boosters!
Balance
Icy weather increases the risk of falling. If you think “having a fall” is something that happens to other/older people, please remember that there’s a first time for everything. Some tips:
- Walk across icy patches with small steps in a flat-footed fashion like a penguin.
- It may not be glamorous, but neither is going A-over-T and breaking (or even just spraining) things.
- Use a handrail if available, even if you don’t think you need to.
You can also check out our previous article about falling (avoiding falling, minimizing the damage of falling, etc):
Fall Special: Some Fall-Themed Advice
Take care!
Share This Post
- Walk across icy patches with small steps in a flat-footed fashion like a penguin.
-
Tasty Tabbouleh with Tahini
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tabbouleh is a salad, but it’s not “just a salad”. It’s a special kind of salad that’s as exciting for the tastebuds as it is healthy for the body and brain. Its core ingredients have been traditional for about a dozen generations, and seasonings are always a personal matter (not to mention that Lebanese tabbouleh-makers centuries ago might not have used miso and nooch, as we will today), but the overall feel of the Gestalt of tabbouleh seasonings remains the same, and this recipe is true to that.
You will need
For the tabbouleh:
- 1 cup bulgur wheat
- 1 cup plum tomatoes, chopped
- 1 cucumber, peeled and chopped (add the peel to a jug of water and put it in the fridge; this will be refreshing cucumber water later!)
- 1 cup chickpeas, cooked without salt
- 1/2 cup parsley, chopped
- 1/2 cup mint, chopped
- 2 spring onions, finely chopped
- 2oz fresh lemon juice
- 1 tsp white miso paste
- 1 tsp garlic powder
- 1 tsp ground cumin
- 1 tsp ground celery seeds
- 1 tsp ground nigella seeds
- 1 tsp ground black pepper
- 1 tsp MSG, or 1/2 tsp low sodium salt (you can find it in supermarkets, the sodium chloride is cut with potassium chloride to make it have less sodium and more potassium)
- 1 tbsp nutritional yeast (nooch), ground (it comes in flakes; you will have to grind it in a spice grinder or with a pestle and mortar)
For the tahini sauce:
- 3 garlic cloves, crushed
- 3 tbsp tahini
- 1 tbsp fresh lemon juice
- 1 tbsp white miso paste
- 1 tsp ground cumin
To serve:
- A generous helping of leafy greens; we recommend collard greens, but whatever works for you is good; just remember that dark green is best. Consider cavolo nero, or even kale if that’s your thing, but to be honest this writer doesn’t love kale
- 1 tsp coarsely ground nigella seeds
- Balsamic vinegar, ideally aged balsamic vinegar (this is thicker and sweeter, but unlike most balsamic vinegar reductions, doesn’t have added sugar).
Method
(we suggest you read everything at least once before doing anything)
1) Rinse the bulgur wheat and then soak it in warm water. There is no need to boil it; the warm water is enough to soften it and you don’t need to cook it (bulgur wheat has already been parboiled before it got to you).
2) While you wait, take a small bowl and mix the rest of the ingredients from the tabbouleh section (so, the lemon juice, miso paste, and all those ground spices and MSG/salt and ground nutritional yeast); you’re making a dressing out of all the ingredients here.
3) When the bulgur wheat is soft (expect it to take under 15 minutes), drain it and put it in a big bowl. Add the tomatoes, cucumber, chickpeas, parsley, mint, and spring onions. This now technically qualifies as tabbouleh already, but we’re not done.
4) Add the dressing to the tabbouleh and mix thoroughly but gently (you don’t want to squash the tomatoes, cucumber, etc). Leave it be for at least 15 minutes while the flavors blend.
5) Take the “For the tahini sauce” ingredients (all of them) and blend them with 4 oz water, until smooth. You’re going to want to drizzle this sauce, so if the consistency is too thick for drizzling, add a little more water and/or lemon juice (per your preference), 1 tbsp at a time.
6) Roughly chop the leafy greens and put them in a bowl big enough for the tabbouleh to join them there. The greens will serve as a bed for the tabbouleh itself.
7) Drizzle the tahini over the tabbouleh, and drizzle a little of the aged balsamic vinegar too.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Share This Post
Related Posts
-
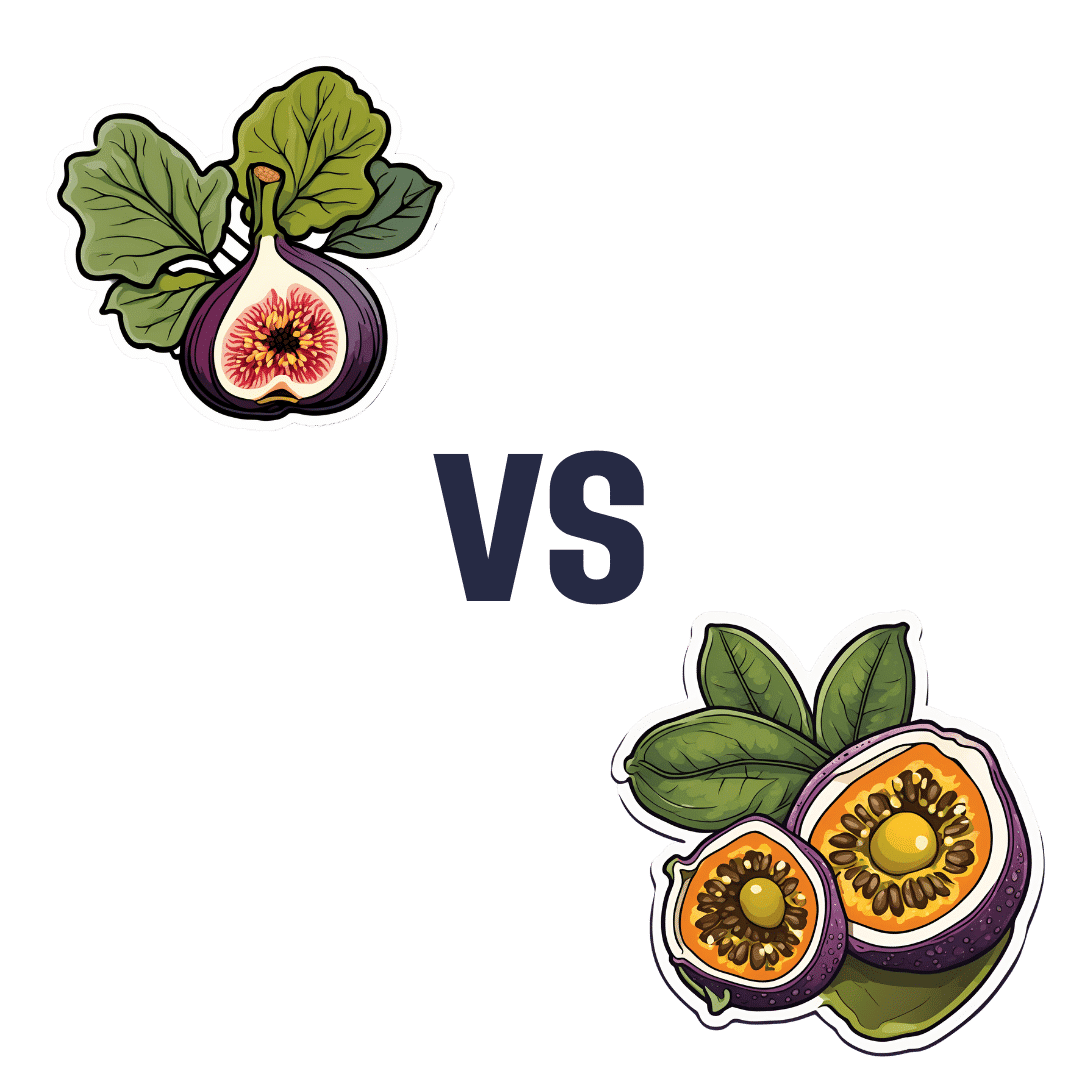
Figs vs Passion Fruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing figs to passion fruit, we picked the passion fruit.
Why?
Both are top-tier fruits! But the passion fruit is just that bit more passionate about delivering healthy nutrients:
In terms of macros, passion fruit has slightly more carbs, notably more protein, and a lot more fiber, giving it the win in this category.
In the category of vitamins, figs have more of vitamins B1, B5, B6, E, and K, while passion fruit has more of vitamins A, B2, B3, B9, C, and choline, making for a marginal win by the numbers for passion fruit here.
When it comes to minerals, figs have more calcium, manganese, and zinc, while passion fruit has more copper, iron, magnesium, phosphorus, potassium, and selenium. A clearer win for passion fruit this time.
Adding up the sections makes for an easy overall win for passion fruit, but again, figs are really a top-tier fruit too; passion fruit just beats them! By all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Top 8 Fruits That Prevent & Kill Cancer ← figs have antitumor effects specifically, while removing carcinogens too, and additionally sensitizing cancer cells to light therapy
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Non-Sleep Deep Rest: A Neurobiologist’s Take
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to get many benefits of sleep, while awake!
Today we’re talking about Dr. Andrew Huberman, a neuroscientist and professor in the department of neurobiology at Stanford School of Medicine.
He’s also a popular podcaster, and as his Wikipedia page notes:
❝In episodes lasting several hours, Huberman talks about the state of research in a specific topic, both within and outside his specialty❞
Today, we won’t be taking hours, and we will be taking notes from within his field of specialty (neurobiology). Specifically, in this case:
Non-Sleep Deep Rest (NSDR)
What is it? To quote from his own dedicated site on the topic:
❝What is NSDR (Yoga Nidra)? Non-Sleep Deep Rest, also known as NSDR, is a method of deep relaxation developed by Dr. Andrew Huberman, a neuroscientist at Stanford University School of Medicine.
It’s a process that combines controlled breathing and detailed body scanning to bring you into a state of heightened awareness and profound relaxation. The main purpose of NSDR is to reduce stress, enhance focus, and improve overall well-being.❞
While it seems a bit bold of Dr. Huberman to claim that he developed yoga nidra, it is nevertheless reassuring to get a neurobiologist’s view on this:
How it works, by science
Dr. Huberman says that by monitoring EEG readings during NSDR, we can see how the brain slows down. Measurably!
- It goes from an active beta range of 13–30 Hz (normal waking) to a conscious meditation state of an alpha range of 8–13 Hz.
- However, with practice, it can drop further, into a theta range of 4–8 Hz.
- Ultimately, sustained SSDR practice can get us to 0.5–3 Hz.
This means that the brain is functioning in the delta range, something that typically only occurs during our deepest sleep.
You may be wondering: why is delta lower than theta? That’s not how I remember the Greek alphabet being ordered!
Indeed, while the Greek alphabet goes alpha beta gamma delta epsilon zeta eta theta (and so on), the brainwave frequency bands are:
- Gamma = concentrated focus, >30 Hz
- Beta = normal waking, 13–30 Hz
- Alpha = relaxed state, 8–13 Hz
- Theta = light sleep, 4–8 Hz
- Delta = deep sleep, 1–4 Hz
Source: Sleep Foundation ← with a nice infographic there too
NSDR uses somatic cues to engage our parasympathetic nervous system, which in turn enables us to reach those states. The steps are simple:
- Pick a time and place when you won’t be disturbed
- Lie on your back and make yourself comfortable
- Close your eyes as soon as you wish, and now that you’ve closed them, imagine closing them again. And again.
- Slowly bring your attention to each part of your body in turn, from head to toe. As your attention goes to each part, allow it to relax more.
- If you wish, you can repeat this process for another wave, or even a third.
- Find yourself well-rested!
Note: this engagement of the parasympathetic nervous system and slowing down of brain activity accesses restorative states not normally available while waking, but 10 minutes of NSDR will not replace 7–9 hours of sleep; nor will it give you the vital benefits of REM sleep specifically.
So: it’s an adjunct, not a replacement
Want to try it, but not sure where/how to start?
When you’re ready, let Dr. Huberman himself guide you through it in this shortish (10:49) soundtrack:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to try it, but not right now? Bookmark it for later
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Green Roasting Tin – by Rukmini Iyer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be wondering: “do I really need a book to tell me to put some vegetables in a roasting tin and roast them?” and maybe not, but the book offers a lot more than that.
Indeed, the author notes “this book was slightly in danger of becoming the gratin and tart book, because I love both”, but don’t worry, most of the recipes are—as you might expect—very healthy.
As for formatting: the 75 recipes are divided first into vegan or vegetarian, and then into quick/medium/slow, in terms of how long they take.
However, even the “slow” recipes don’t actually take more effort, just, more time in the oven.
One of the greatest strengths of this book is that not only does it offer a wide selection of wholesome mains, but also, if you’re putting on a big spread, these can easily double up as high-class low-effort sides.
Bottom line: if you’d like to eat more vegetables in 2024 but want to make it delicious and with little effort, put this book on your Christmas list!
Click here to check out The Green Roasting Tin, and level-up yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: