Healthy Habits for Managing & Reversing Prediabetes – by Dr. Marie Feldman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
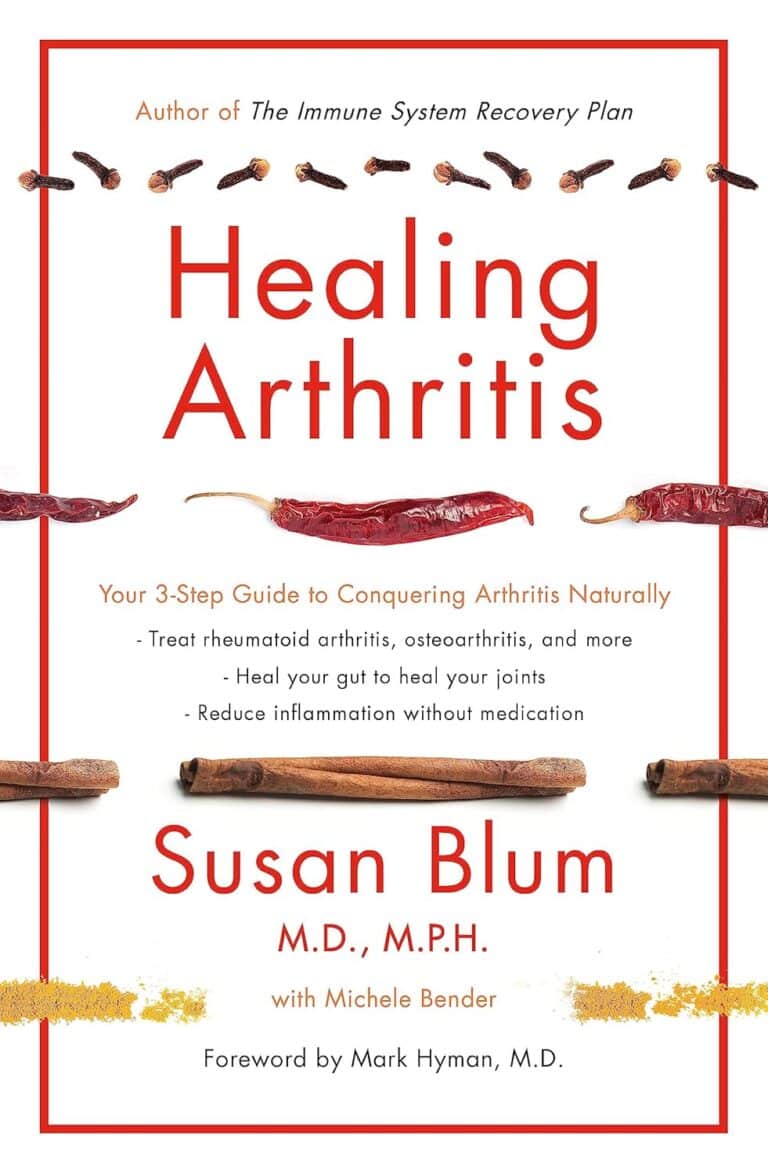
The book doesn’t assume prior knowledge, and does explain the science of diabetes, prediabetes, the terms and the symptoms, what’s going on inside, etc—before getting onto the main meat of the book, the tips.
The promised 100 tips are varied in their application; they range from diet and exercise, to matters of sleep, stress, and even love.
There are bonus tips too! For example, an appendix covers “tips for healthier eating out” (i.e. in restaurants etc) and a grocery list to ensure your pantry is good for defending you against prediabetes.
The writing style is very accessible pop-science; this isn’t like reading some dry academic paper—though it does cite its sources for claims, which we always love to see.
Bottom line: if you’d like to proof yourself against prediabetes, and are looking for “small things that add up” habits to get into to achieve that, this book is an excellent first choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 Tips To Burn Fat & Build Muscle At The Same Time
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cori Lefkowith, of “Redefining Strength” and “Strong At Any Age” fame, has her formula to share:
Know your priorities
We’ll not keep the 7 tips a mystery; they are:
- Determine your primary goal: decide whether your main focus is losing fat while building muscle or building muscle while trimming up. This choice will influence your calorie intake, macros, and cardio approach.
- Start tracking: spend 7–14 days logging your current food intake, including calories, protein, carbs, and fats, without taking any particular action to change them yet. Understanding your baseline will help tailor your diet and exercise plan.
- Prioritize strength training: focus on strength work over cardio to build muscle. Avoid turning strength sessions into cardio by rushing between sets—allow adequate rest for muscle progression.
- Center your meals on protein: adjust your protein intake based on your primary goal. For fat loss while gaining muscle, aim for 40-45% of calories from protein. For building muscle while losing fat, aim for 30-40% protein, with attention to maintaining sufficient carbs.
- Set your calories: after adjusting protein, fine-tune your calorie intake. However, make only small changes (e.g. 100 calories up or down) and reassess every 2–3 weeks to avoid extreme deficits or surpluses.
- Adjust your cardio: prioritize strength training but use walking as low-impact cardio. Avoid excessive cardio that may hinder muscle gains, and use strategic HIIT sessions if needed.
- Ditch the scale: avoid using the scale as your sole measure of progress. Instead, rely on measurements, progress photos, and how your clothes fit to track body recomposition effectively.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Can You Gain Muscle & Lose Fat At The Same Time? ← we got this question in our Q&A day not long back, and here was our answer. We went for a less numbers-based approach, and a more principles-based approach. Both ways work, so by all means pick whichever method you personally find better suits how you like to do things!
Take care!
Share This Post
-
What Is “75 Hard”?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
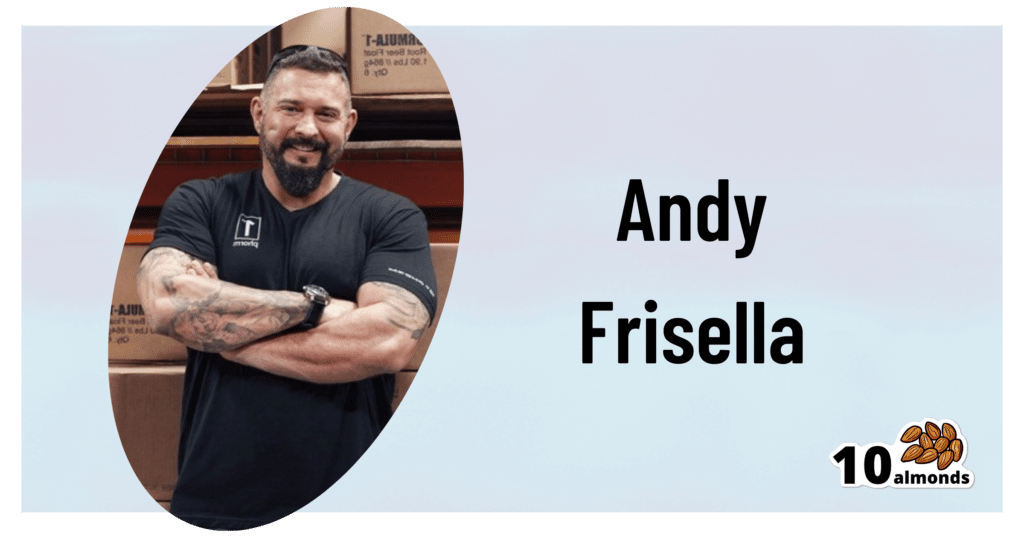
This is Andy Frisella. He’s not a doctor, scientist, nutritionist, personal trainer, or professional athlete, but he has kicked off a viral fitness challenge, so let’s take a look at it:
What it is
Firstly, Frisella asserts that it’s not a fitness challenge, but rather, he describes it as a “transformative mental toughness program”.
Here’s what it consists of:
- Follow a healthy diet plan with no deviations from it (i.e. no “cheat days”)
- Abstain from alcohol
- Exercise 2x per day, 45 minutes each
- One of the exercise sessions each day must be outside
- No rest days
- Drink 3.5 liters of water per day
And the duration? 75 days, hence the name of the
fitness challengetransformative mental toughness program.Why it is
Frisella’s rationale is:
- we must cultivate mental toughness by doing hard things
- allowing ourselves any deviation would be a sign of mental weakness
- if we allow ourselves to deviate, it becomes a habit
For this reason, he does not “allow” any substitutions, for example if somebody wants to do such-and-such a thing slightly differently instead. We put “allow” in quotation marks because of course, he’s not the boss of you, but per the rules of his challenge, at least.
These reasonings are in and of themselves somewhat sound, however, we at 10almonds would argue:
- before doing hard things, it is good to first consider “is it a good idea?” (amputating your leg using only a spork is a “hard thing”, and demonstrates incredible mental toughness, but that doesn’t make it a good idea)
- while being able to decide to do a thing and then do it is great characteristic to have, it’s good to first consider science; for example, restrictive diets with no flexibility simply do not work, and our bodies do require adequate rest, especially if being pushed through hard things, or problems will happen (injuries, illnesses, etc).
- while it’s true that allowing ourselves to deviate can become a habit, it’s good to first consider what habits we want to make, and make those habits, instead of potentially unsustainable or even simply unpleasant ones.
See also: What Flexible Dieting Really Means: When Flexibility Is The Dish Of The Day
And for that matter: How To Really Pick Up (And Keep!) Those Habits
Want a “75 Gentle” instead?
If you like the idea of making new habits, but are not sure if extreme (and perhaps arbitrary) standards are the ones you want to hold, check out:
Cori Lefkowith’s 25 Healthy Habits That Will Change Your Life
Take care!
Share This Post
-
Retinoids: Retinol vs Retinal vs Retinoic Acid vs..?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I’m confused about retinol, retinal, retinoin, retinoids, etc, and of course every product claims to be the best, what’s the actual science on it?❞
Before we get into these skincare products, let’s first note that for most people, what’s best for the skin is good sleep and hydration, a plants-centric whole foods diet, and good stress management:
See for example: Of Brains And Breakouts: The Brain Skin Doctor
However, the world of potions and lotions can be an alluring one, and there is some merit there too. So, in a nutshell:
- Retinoids are the overall class of chemicals, and not a specific type
- Retinoic acid is the strongest form of this chemical and is prescription-controlled in most places
- “Retinoin” is probably tretinoin (all-trans retinoic acid) with the “t” having fallen off; we can only find it being used as a product name, not an actual substance
- Retinal, when it’s not an adjective referring to the retina (the part of the eye that receives refocussed light) and is instead a noun, is a less potent retinoid than the prescription-only kinds, but still stronger than retinol
- Retinol is a much less potent form, and is the most widely found in skincare products
- Retinoic acid is the strongest form of this chemical and is prescription-controlled in most places
All of them work the same way; it is only how serious they are about it that differs.
The mechanism of action is that they speed up the turnover (shedding cycle) of skin, so that cells are replaced sooner. As with any non-cancerous human tissue, this means that the tissue itself (in this case, your skin) will be biologically younger than if it had been replaced later.
The downside, of course, of this is that—while trying to make your skin healthier and more beautiful—the first thing that will happen is skin shedding. Depending on the retinoid type, dose, and the health of your skin to start with, this may mean anything from needing to exfoliate in the morning, to having to go to hospital with what looks like the world’s worst sunburn. For this reason, it is recommended to start with weaker products and lower doses, and work up carefully.
A note on doses: the recommended doses for these products are always truly tiny, like “use a pea-sized amount of this 0.05% serum on your face”. Take them seriously until you’re absolutely sure from experience that your skin can handle more.
Also, a tip: wear gloves when you apply any of the above products. This is because your fingers are also covered in skin, and if you don’t use gloves, then half the product that you intended for your face will be absorbed into your fingers instead. On the bright side, you’ll have beautifully rejuvenated fingertips, though.
You can learn more about the science of retinoids here, in our article about tretinoin, the usually prescription-only form of retinoic acid:
Tretinoin: Undo The Sun’s Damage To Your Skin
Want to try some?
We don’t sell it, but here for your convenience is an example product of retinal (stronger than retinol) on Amazon 😎
Take care!
Share This Post
- Retinoids are the overall class of chemicals, and not a specific type
Related Posts
-
Infrared-Reflecting Patches For Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Hi! I’ve been reading about LifeWave patches, would you recommend them?❞
For reference first, this is talking about these: LifeWave.com
Short answer: no
Longer answer: their main premise seems to be that the patches (subscription prices seem to start from about $100–$300 per month) reflect infrared energy back into your body, making you more energized and healthy.
Fun fact: aluminum foil reflects infrared energy (which we feel as heat), by the way, and that is why space blankets (of the kind used in emergencies and by some athletes) are made shiny like that, often with aluminized mylar.
We cannot comment too closely on the rest of the presented science of their products, as it seems quite unlike anything we’re accustomed to reading, and we were not able to make a lot of sense of it.
They do cite research papers to back their claims, including research conducted by the company’s founder and published via an open journal.
Many others are independent studies conducted by often the same researchers as each other, mostly experts in acupuncture and acupressure.
For the papers we looked at, the sample sizes were very small, but the conclusions were very positive.
They were published in a variety of journals, of which we cannot claim any prior knowledge (i.e:, they were not the peer-reviewed journals from which we cite most of our sources).
Also, none were registered with ClinicalTrials.gov.
To be on the safe side, their disclaimer does advise:
❝LifeWave products are only intended to maintain or encourage a general state of health or healthy activity and are not intended to diagnose, treat, cure, mitigate, or prevent any disease or medical condition of the body❞
They do have a Frequently Asked Questions page, which tells about ancient Egyptian use of colored glass, as well as more modern considerations including joining, ordering, their commissions system, binary commissions and matching bonuses, and “how to rank up in LifeWave” as well as a lot of information about subscribing as a preferred customer or a brand partner, opting in to their multi-level marketing opportunities.
Here’s what “Honest Brand Reviews” had to say:
Honest Brand Reviews | LifeWave Review
Our position:
We cannot honestly claim to understand their science, and thus naturally won’t actively recommend what we can’t speak for.
An expert’s position:
Since we couldn’t understand how this would work, here’s what Dr. Paul Knoepfler has to say about their flagship product, the LifeWave X39 patch:
LifeWave X39 stem cell patch story has holes
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Aging Backwards – by Miranda Esmonde-White
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In this book, there’s an upside and a downside to the author’s professional background:
- Upside: Miranda Esmonde-White is a ballet-dancer-turned-physical-trainer, and it shows
- Downside: Miranda Esmonde-White is not a scientist, and it shows
She cites a lot of science, but she either does not understand it or else intentionally misrepresents it. We will assume the former. But as one example, she claims:
“for every minute you exercise, you lengthen your life by 7 minutes”
…which cheat code to immortality is absolutely not backed-up by the paper she cites for it. The paper, like most papers, was much more measured in its proclamations; “there was an association” and “with these conditions”, etc.
Nevertheless, while she misunderstands lots of science along the way, her actual advice is good and sound. Her workout programs really will help people to become younger by various (important, life-changing!) metrics of biological age, mostly pertaining to mobility.
And yes, this is a workout-based approach; we won’t read much about diet and other lifestyle factors here.
Bottom line: it has its flaws, but nevertheless delivers on its premise of helping the reader to become biologically younger through exercises, mostly mobility drills.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Get On It! – by Jane Aronovitch, Miriane Taylor, & Colleen Craig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Balance is important; without it, we die early. That’s quite a strong selling point for improving one’s balance, but why this book in particular?
This is—with one drawback—the best book of balance ball exercises we’ve seen. Notwithstanding the cover photo, many exercises do, by the way, involve standing on it with one or both feet, doing various kinds of squats, lunges, get-ups, and so forth. The ball (it’s not really a ball so much as an oblate hemisphere) can also be flipped and used the other way around, with a flat platform that will now wobble per your weight distribution, and train balance in different ways (dome-up trains large stabilizing muscles more; platform-up trains smaller stabilizing muscles more).
Indeed, that’s where the brand name Bosu, often stylized “BOSU”, comes from: both sides up!
So, what’s the drawback? Alas, the photos are black and white, which means in some cases they’re not as clear as they could be. Nothing that will prevent understanding the exercises, which are well-explained in any case, but it does mean that sometimes it’s necessary to look closely to see which leg is in front of the other for a given exercise, for example.
Still, with 80 different exercises it really does cover the whole body, and even gives workout program varieties for those who want that, including targeted to particular areas, e.g. lower body, core, upper body, or complete.
Bottom line: if you’d like to improve your balance (and have, or are willing to acquire, a balance ball like the Bosu), then this book will give you everything else you need in that regard.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: