Gut-Healthy Labneh Orecchiette
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Labneh (a sort of yogurt-cheese made from strained yogurt) is a great probiotic, and there’s plenty of resistant starch in this dish too, from how we cook, cool, and reheat the pasta. Add to this the lycopene from the tomatoes, the ergothioneine from the mushrooms, and the healthful properties of the garlic, black pepper, and red chili, and we have a very healthy dish!
You will need
- 10 oz labneh (if you can’t buy it locally, you can make your own by straining Greek yogurt through a muslin cloth, suspended over a bowl to catch the water that drips out, overnight—and yes, plant-based is also fine if you are vegan, and the gut benefits are similar because unlike vegan cheese, vegan yogurt is still fermented)
- 6 oz wholegrain orecchiette (or other pasta, but this shape works well for this sauce)
- ¼ bulb garlic, grated
- Juice of ½ lemon
- Large handful chopped parsley
- Large handful chopped dill
- 9 oz cherry tomatoes, halved
- 9 oz mushrooms (your choice what kind), sliced (unless you went for shiitake or similar, which don’t need it due to already being very thin)
- 2 tsp black pepper, coarse ground
- 1 tsp red chili flakes
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Cook the pasta as you normally would. Drain, and rinse with cold water. Set aside.
2) Combine the labneh with the garlic, black pepper, dill, parsley, and lemon juice, in a large bowl. Set aside.
3) Heat a little olive oil in a skillet; add the chili flakes, followed by the mushrooms. Cook until soft and browned, then add the tomatoes and fry for a further 1 minute—we want the tomatoes to be blistered, but not broken down. Stir in the MSG/salt, and take off the heat.
4) Refresh the pasta by passing a kettle of boiling water through it in a colander, then add the hot pasta to the bowl of labneh sauce, stirring to coat thoroughly.
5) Serve, spooning the mushrooms and tomatoes over the labneh pasta.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chicken or Fish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chicken to fish, we picked the fish.
Why?
To understand the choice, we have to start a bit earlier on the decision tree. For most people most of the time, when it comes to a diet high in plants or high in animals, the plant-centric diet will generally be best:
Do We Need Animal Products To Be Healthy?
When it comes to animal meats, red meat is a fairly uncontroversial first thing to strike off the list:
…with pork and some other meats not being much better.
But chicken? Poultry in general appears to be quite health-neutral. The jury is out and the science has mixed results, but the data is leaning towards “it’s probably fine”.
See for example this huge (n=29,682) study:
this same paper shows that…
❝higher intake of processed meat, unprocessed red meat, or poultry, but not fish, was significantly associated with a small increased risk of incident CVD, whereas higher intake of processed meat or unprocessed red meat, but not poultry or fish, was significantly associated with a small increased risk of all-cause mortality❞
So, since poultry isn’t significantly increasing all-cause mortality, and fish isn’t significantly increasing all-cause mortality or cardiovascular disease, fish comes out as the hands-down (fins-down?) winner.
One more (this time, easy) choice to make, though!
While fish in general (please, not fried, though!) is generally considered quite healthy, there is a big difference (more than you might think, and for reasons that are quite alarming), between…
Health Risks & Nutrition: Farmed Fish vs Wild-Caught
Enjoy, and take care!
Share This Post
-
An RSV vaccine has been approved for people over 60. But what about young children?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Therapeutic Goods Administration (TGA) has approved a vaccine against respiratory syncytial virus (RSV) in Australia for the first time. The shot, called Arexvy and manufactured by GSK, will be available by prescription to adults over 60.
RSV is a contagious respiratory virus which causes an illness similar to influenza, most notably in babies and older adults.
So while it will be good to have an RSV vaccine available for older people, where is protection up to for the youngest children?
A bit about RSV
RSV was discovered in chimpanzees with respiratory illness in 1956, and was soon found to be a common cause of illness in humans.
There are two key groups of people we would like to protect from RSV: babies (up to about one year old) and people older than 60.
Babies tend to fill up hospitals during the RSV season in late spring and winter in large numbers, but severe infection requiring admission to intensive care is less common.
In babies and younger children, RSV generally causes a wheezing asthma-like illness (bronchiolitis), but can also cause pneumonia and croup.
Although there are far fewer hospital admissions among older people, they can develop severe disease and die from an infection.
Babies account for the majority of hospitalisations with RSV.
Prostock-studio/ShutterstockRSV vaccines for older people
For older adults, there are actually several RSV vaccines in the pipeline. The recent Australian TGA approval of Arexvy is likely to be the first of several, with other vaccines from Pfizer and Moderna currently in development.
The GSK and Pfizer RSV vaccines are similar. They both contain a small component of the virus, called the pre-fusion protein, that the immune system can recognise.
Both vaccines have been shown to reduce illness from RSV by more than 80% in the first season after vaccination.
In older adults, side effects following Arexvy appear to be similar to other vaccines, with a sore arm and generalised aches and fatigue frequently reported.
Unlike influenza vaccines which are given each year, it is anticipated the RSV vaccine would be a one-off dose, at least at this stage.
Protecting young children from RSV
Younger babies don’t tend to respond well to some vaccines due to their immature immune system. To prevent other diseases, this can be overcome by giving multiple vaccine doses over time. But the highest risk group for RSV are those in the first few months of life.
To protect this youngest age group from the virus, there are two potential strategies available instead of vaccinating the child directly.
The first is to give a vaccine to the mother and rely on the protective antibodies passing to the infant through the placenta. This is similar to how we protect babies by vaccinating pregnant women against influenza and pertussis (whooping cough).
The second is to give antibodies directly to the baby as an injection. With both these strategies, the protection provided is only temporary as antibodies wane over time, but this is sufficient to protect infants through their highest risk period.
Women could be vaccinated during pregnancy to protect their baby in its first months of life.
Image Point Fr/ShutterstockAbrysvo, the Pfizer RSV vaccine, has been trialled in pregnant women. In clinical trials, this vaccine has been shown to reduce illness in infants for up to six months. It has been approved in pregnant women in the United States, but is not yet approved in Australia.
An antibody product called palivizumab has been available for many years, but is only partially effective and extremely expensive, so has only been given to a small number of children at very high risk.
A newer antibody product, nirsevimab, has been shown to be effective in reducing infections and hospitalisations in infants. It was approved by the TGA in November, but it isn’t yet clear how this would be accessed in Australia.
What now?
RSV, like influenza, is a major cause of respiratory illness, and the development of effective vaccines represents a major advance.
While the approval of the first vaccine for older people is an important step, many details are yet to be made available, including the cost and the timing of availability. GSK has indicated its vaccine should be available soon. While the vaccine will initially only be available on private prescription (with the costs paid by the consumer), GSK has applied for it to be made free under the National Immunisation Program.
In the near future, we expect to hear further news about the other vaccines and antibodies to protect those at higher risk from RSV disease, including young children.
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
My dance school is closed for the summer, how can I keep up my fitness?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Once the end-of-year dance concert and term wrap up for the year it is important to take a break. Both physical and mental rest are important and taking a few weeks off can help your body repair and have a mental break from dance.
If your mind and body are in need of an extended break (such as more than a few weeks), then it’s more than OK to take longer off, especially if you are training at a competitive or pre-professional level.
There is benefit in enjoying other aspects of your life outside of dance such as spending time with family, friends and enjoying hobbies.
Tatyana Vyc/Shutterstock A safe, fulfilling dancing life
Creating meaning and value in life outside of dance and expanding sense of self can make it easier to lean into other aspects when experiencing change or difficult times during dance training such as being injured.
Taking an extended break from dance training will, however, mean losing some fitness and physical capacity. When you return to dance your body will take time to return to full capacity again.
Approaches such as being “whipped back into shape” can promote sudden spikes in training load (hours and intensity of training) which can increase the risk of injury. It is advised to gradually and progressively increase training load over time to allow the body to adapt and return to full capacity safely.
A four-to-six week period of gradually progressing training load and introducing jumping has been suggested in dance settings.
For dancers wanting to maintain fitness over the summer holidays, a great place to start is focusing on building a physical foundation.
Exercise like running can help build a physical foundation. Jacek Chabraszewski/Shutterstock Building a physical foundation means focusing on targeted areas of fitness such as full body strength, cardiovascular fitness or stamina (such as skipping, cycling walking, running, swimming), flexibility, and some dance-specific conditioning (for example, calf rises for ballet).
A good physical foundation will mean an improved capacity and fitness level so your body is ready to take on more challenging dance movements and routines once you return to the studio.
Building full body strength at home or at the park
A great place to start is by choosing movements that require your muscles to work to support your own body weight.
Fundamental movements such as crawling (moving on the floor on hands and feet) and locomotion (travelling movements such as lunging, hopping, sliding) are great for developing body control, arm and leg stability and coordinated movement patterns.
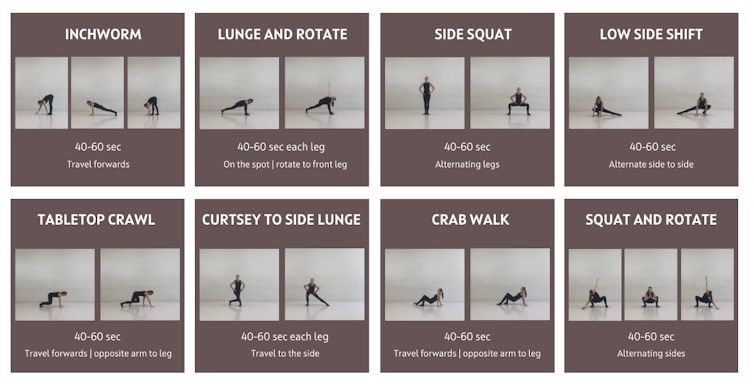
Below is a sequence that can be used as a warm up and even as a workout itself. The ten minute sequence is based on gross motor and fundamental movement patterns. It includes exercises that work through a range of joint movements and in multiple planes (forwards, sideways, rotating).
This fundamental movement sequence can be used as a warm-up or a workout. Joanna Nicholas, CC BY Once feeling comfortable with the above fundamental movements, it is time to introduce body weight resistance exercises.
Body weight resistance exercises can be beneficial for developing a strong foundation for dance movements such as jumping, landing, floorwork, partnering and aerial work.
Exercises from the above sequence can be used to form a safe and effective neuromuscular warm up.
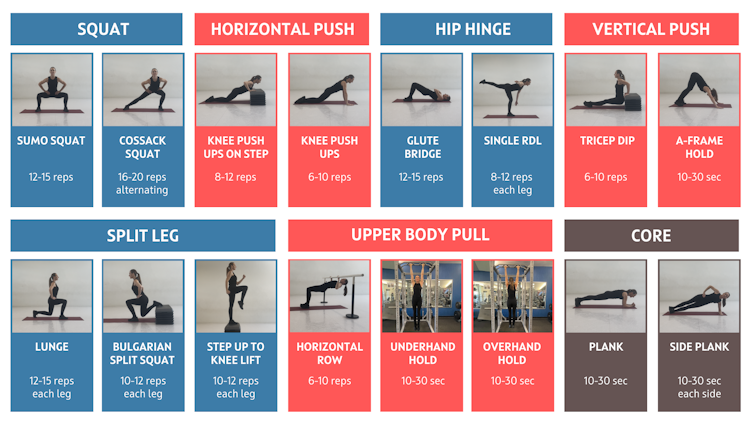
Aim to include one exercise from each of the below movement categories (squat, horizontal push etc) to build your own workout.
Aim to complete two to three sets (or rounds) of each exercise with about one minute rest between sets. An alternative is to complete one set of each exercise with minimal rest between, then complete a second or third time.
If training with friends, you could set a timer and do each exercise for up to 50 seconds (instead of counting reps) and take ten seconds to transition to the next exercise.
Depending on your level of strength you may need to do fewer repetitions and build up sets and repetitions overtime. After you have completed the body weight exercises complete a cool down including stretches for the upper and lower body muscles. Be sure to use a sturdy bar (such as an outdoor fitness station) for horizontal row and overhead hold.
Exercises may need to be modified depending on fitness level and physical limitations such as injury.
You can build your own full body strength workout using these movements. Joanna Nicholas, CC BY How often should I train?
A common misconception in dance is that “more is better”. This belief can lead to dancers training long hours on most or all days of the week which can lead to overtraining, plateauing and increased risk of injury.
Our bodies require sufficient time between training sessions to adapt and get stronger and fitter. The time between sessions is when our muscles and tissues repair and training gains are made.
By incorporating adequate recovery (including sleep and downtime) and including rest days throughout the week, our bodies can gain the most benefits from training.
Rest days are important, too. Manop Boonpeng/Shutterstock Muscles can take up to 48–72 hours to recover from most types of strength-based exercises (the more intense the longer they’ll need to recover).
Aerobic activity at low intensity, such as a brisk walk, can be done most days (24-hour recovery) while high stress anaerobic exercise such as high intensity intervals or sprints can take three days or more to recover from.
Aim to spread training sessions out over the week and allow time to recover between sessions.
Below is an example weekly schedule based on incorporating adequate recovery between sessions, and incorporating polarised training where some days are harder and others are easier.
Seek guidance from your healthcare provider and/or an exercise professional prior to undertaking a new exercise program.
Joanna Nicholas, Lecturer in Dance and Performance Science, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Your Brain On (And Off) Estrogen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Lisa Mosconi. She’s a professor of Neuroscience in Neurology and Radiology, and is one of the 1% most influential scientists of the 21st century. That’s not a random number or an exaggeration; it has to do with citation metrics collated over 20 years:
A standardized citation metrics author database annotated for scientific field
What does she want us to know?
Women’s brains age differently from men’s
This is largely, of course, due to menopause, and as such is a generalization, but it’s a statistically safe generalization, because:
- Most women go through menopause—and most women who don’t, avoid it by dying pre-menopause, so the aging also does not occur in those cases
- Menopause is very rarely treated immediately—not least of all because menopause is diagnosed officially when it has been one year since one’s last period, so there’s almost always a year of “probably” first, and often numerous years, in the case of periods slowing down before stopping
- Menopausal HRT is great, but doesn’t completely negate that menopause occurred—because of the delay in starting HRT, some damage can be done already and can take years to reverse.
Medicated and unmedicated menopause proceed very differently from each other, and this fact has historically caused obfuscation of a lot of research into age-related neurodegeneration.
For example, it is well-established that women get Alzheimer’s at nearly twice the rate than men do, and deteriorate more rapidly after onset, too.
Superficially, one might conclude “estrogen is to blame” or maybe “the xx-chromosomal karyotype is to blame”.
The opposite, however, is true with regard to estrogen—estrogen appears to be a protective factor in women’s neurological health, which is why increased neurodegeneration occurs when estrogen levels decline (for example, in menopause).
For a full rundown on this, see:
Alzheimer’s Sex Differences May Not Be What They Appear
It’s not about the extra X
Dr. Mosconi examines this in detail in her book “The XX Brain”. To summarize and oversimplify a little: the XX karyotype by itself makes no difference, or more accurately, the XY karyotype by itself makes no difference (because biologically speaking, female physiological attributes are more “default” than male ones; it is only 12,000ish* years of culture that has flipped the social script on this).
*Why 12,000ish years? It’s because patriarchalism largely began with settled agriculture, for reasons that are fascinating but beyond the scope of this article, which is about health science, not archeology.
The topic of “which is biologically default” is relevant, because the XY karyotype (usually) informs the body “ignore previous instructions about ovaries, and adjust slightly to make them into testes instead”, which in turn (usually) results in a testosterone-driven system instead of an estrogen-driven system. And that is what makes the difference to the brain.
One way we can see that it’s about the hormones not the chromosomes, is in cases of androgen insensitivity syndrome, in which the natal “congratulations, it’s a girl” pronouncement may later be in conflict with the fact it turns out she had XY chromosomes all along, but the androgenic instructions never got delivered successfully, so she popped out with fairly typical female organs. And, relevantly for Dr. Mosconi, a typically female brain that will age in a typically female fashion, because it’s driven by estrogen, regardless of the Y-chromosome.
The good news
The good news from all of this is that while we can’t (with current science, anyway) do much about our chromosomes, we can do plenty about our hormones, and also, the results of changes in same.
Remember, Dr. Mosconi is not an endocrinologist, nor a gynecologist, but a neurologist. As such, she makes the case for how a true interdisciplinary team for treating menopause should not confined to the narrow fields usually associated with “bikini medicine”, but should take into account that a lot of menopause-related changes are neurological in nature.
We recently reviewed another book by Dr. Mosconi:
The Menopause Brain – by Dr. Lisa Mosconi
…and as we noted there, many sources will mention “brain fog” as a symptom of menopause, Dr. Mosconi can (and will) point to a shadowy patch on a brain scan and say “that’s the brain fog, there”.
And so on, for other symptoms that are often dismissed as “all in your head”, as though that’s a perfectly acceptable place for problems to be.
This is critical, because it’s treating real neurological things as the real things they are.
Dr. Mosconi’s advice, beyond HRT
Dr. Mosconi notes that brain health tends to dip during perimenopause but often recovers, showing the brain’s resilience to hormonal shifts. As such, all is not lost if for whatever reason, hormone replacement therapy isn’t a viable option for you.
Estrogen plays a crucial role in brain energy, and women’s declining estrogen levels during menopause increase the need for antioxidants to protect brain health—something not often talked about.
Specifically, Dr. Mosconi tells us, women need more antioxidants and have different metabolic responses to diets compared to men.*
*Yes, even though men usually have negligible estrogen, because their body (and thus brain, being also part of their body) is running on testosterone instead, which is something that will only happen if either you are producing normal male amounts of testosterone (requires normal male testes) or you are taking normal male amounts of testosterone (requires big bottles of testosterone; this isn’t the kind of thing you can get from a low dose of testogel as sometimes prescribed as part of menopausal HRT to perk your metabolism up).
Note: despite women being a slight majority on Earth, and despite an aging population in wealthy nations, meaning “a perimenopausal woman” is thus the statistically average person in, for example, the US, and despite the biological primacy of femaleness… Medicine still mostly looks to men as the “default person”, which in this case can result in seriously low-balled estimates of what antioxidants are needed.
In terms of supplements, therefore, she recommends:
- Antioxidants: key for brain health, especially in women. Rich sources include fruits (especially berries) and vegetables. Then there’s the world’s most-consumed antioxidant, which is…
- Coffee: Italian-style espresso has the highest antioxidant power. Adding a bit of fat (e.g. oat milk) helps release caffeine more slowly, reducing jitters. Taking it alongside l-theanine also “flattens the curve” and thus improves its overall benefits.
- Flavonoids: important for both men and women but particularly essential for women. Found in many fruits and vegetables.
- Chocolate: dark chocolate is an excellent source of antioxidants and flavonoids!
- Turmeric: a natural neuroprotectant with anti-inflammatory properties, best boosted by taking with black pepper, which improves absorption as well as having many great qualities of its own.
- B Vitamins: B6, B9, and B12 are essential for anti-aging and brain health; deficiency in B6 is rare, while deficiency in B9 (folate) and especially B12 is very common later in life.
- Vitamins C & E: important antioxidants, but caution is needed with fat-soluble vitamins to avoid toxicity.
- Omega-3s: important for brain health; can be consumed in the diet, but supplements may be necessary.
- Caution with zinc: zinc can support immunity and endocrine health (and thus, indirectly, brain health) but may be harmful in excess, particularly for brain health.
- Probiotics & Prebiotics: beneficial for gut health, and in Dr. Mosconi’s opinion, hard to get sufficient amounts from diet alone.
For more pointers, you might want to check out the MIND diet, that is to say, the “Mediterranean-DASH Intervention for Neurodegenerative Delay” upgrade to make the Mediterranean diet even brain-healthier than it is by default:
Four Ways To Upgrade The Mediterranean Diet
Want to know more from Dr. Mosconi?
Here’s her TED talk:
Click Here If The Embedded Video Doesn’t Load Automatically!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Vitamin B6 is essential – but too much can be toxic. Here’s what to know to stay safe
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In recent weeks, reports have been circulating about severe reactions in people who’ve taken over-the-counter vitamin B6 supplements.
Vitamin B6 poisoning can injure nerves and lead to symptoms including numbness, tingling and even trouble walking and moving.
In some cases, those affected didn’t know the product contained any vitamin B6.
So what is vitamin B6, where is it found and how much is too much? Here’s what you need to know about this essential nutrient.
Kim Kuperkova/Shutterstock What is vitamin B6?
Vitamin B6 (also known as pyridoxine) is a group of six compounds that share a similar chemical structure.
It is an essential nutrient, meaning we need it for normal body functions, but we can’t produce it ourselves.
Adults aged 19–50 need 1.3mg of vitamin B6 per day. The recommended dose is lower for teens and children, and higher for those aged 51 and over (1.7mg for men and 1.5mg for women) and people who are breastfeeding or pregnant (1.9mg).
Most of us get this in our diet – largely from animal products, including meat, dairy and eggs.
The vitamin is also available in a range of different plant foods, including spinach, kale, bananas and potatoes, so deficiency is rare, even for vegetarians and vegans.
The vitamin B6 we consume in the diet is inactive, meaning the body can’t use it. To activate B6, the liver transforms it into a compound called pyridoxal-5’-phosphate (PLP).
In this form, vitamin B6 helps the body with more than 140 cellular functions, including building and breaking down proteins, producing red blood cells, regulating blood sugar and supporting brain function.
Vitamin B6 is important for overall health and has also been associated with reduced cancer risk and inflammation.
Despite being readily available in the diet, vitamin B6 is also widely included in various supplements, multivitamins and other products, such as Berocca and energy drinks.
Most people get enough vitamin B6 from their diet. Tatjana Baibakova/Shutterstock Should we be worried about toxicity?
Vitamin B6 toxicity is extremely rare. It almost never occurs from dietary intake alone, unless there is a genetic disorders or disease that stops nutrient absorption (such as coeliac disease).
This is because all eight vitamins in the B group are water-soluble. If you consume more of the vitamin than your body needs, it can be excreted readily and harmlessly in your urine.
However, in some rare cases, excessive vitamin B6 accumulates in the blood, resulting in a condition called peripheral neuropathy. We’re still not sure why this occurs in some people but not others.
Peripheral neuropathy occurs when the sensory nerves – those outside our brain and spinal cord that send information to the central nervous system – are damaged and unable to function. This can be caused by a wide range of diseases (and is most well known in type 2 diabetes).
The most common symptoms are numbness and tingling, though in some cases patients may experience difficulty with balance or walking.
We don’t know exactly how excess vitamin B6 causes peripheral neuropathy, but it is thought to interfere with how the neurotransmitter GABA sends signals to the sensory nerves.
Vitamin B6 can cause permanent damage to nerves. Studies have shown symptoms improved when the person stopped taking the supplement, although they didn’t completely resolve.
What is considered excessive? And has this changed?
Toxicity usually occurs only when people take supplements with high doses of B6.
Until 2022, only products with more than 50mg of vitamin B6 were required to display a warning about peripheral neuropathy. But the Therapeutic Goods Administration lowered this and now requires any product containing more than 10mg of vitamin B6 to carry a warning.
The Therapeutic Goods Administration has also halved the daily upper limit of vitamin B6 a product can provide – from 200mg to 100mg.
These changes followed a review by the administration, after receiving 32 reports of peripheral neuropathy in people taking supplements. Two thirds of these people were taking less than 50mg of vitamin B6.
The Therapeutic Goods Administration acknowledges the risk varies between individuals and a lot is unknown. Its review could not identify a minimum dose, duration of use or patient risk factors.
But I thought B vitamins were good for me?
Too much of anything can cause problems.
The updated guidelines are likely to significantly lower the risk of toxicity. They also make consumers more aware of which products contain B6, and the risks.
The Therapeutic Goods Administration will continue to monitor evidence and revise guidelines if necessary.
While vitamin B6 toxicity remains very rare, there are still many questions about why some people get peripheral neuropathy with lower dose supplements.
It could be that some specific vitamin B compounds have a stronger effect, or some people may have genetic vulnerabilities or diseases which put them at higher risk.
So what should I do?
Most people don’t need to actively seek vitamin B6 in supplements.
However, many reports to the Therapeutic Goods Administration were of vitamin B6 being added to supplements labelled as magnesium or zinc – and some weren’t aware they were consuming it.
It is important to always check the label if you are taking a new medicine or supplement, especially if it hasn’t been explicitly prescribed by a health-care professional.
Be particularly cautious if you are taking multiple supplements. While one multivitamin is unlikely to cause an issue, adding a magnesium supplement for cramping, or a zinc supplement for cold and flu symptoms, may cause an excessive vitamin B6 dose over time, and increase your risk.
Importantly, pay attention to symptoms that may indicate peripheral neuropathy, such as pins and needles, numbness, or pain in the feet or hands, if you do change or add a supplement.
Most importantly, if you need advice, you should talk to your doctor, dietitian or pharmacist.
Vasso Apostolopoulos, Distinguished Professor, Professor of Immunology, RMIT University and Jack Feehan, Vice Chancellors Senior Research Fellow in Immunology, RMIT University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
War in Ukraine affected wellbeing worldwide, but people’s speed of recovery depended on their personality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The war in Ukraine has had impacts around the world. Supply chains have been disrupted, the cost of living has soared and we’ve seen the fastest-growing refugee crisis since World War II. All of these are in addition to the devastating humanitarian and economic impacts within Ukraine.
Our international team was conducting a global study on wellbeing in the lead up to and after the Russian invasion. This provided a unique opportunity to examine the psychological impact of the outbreak of war.
As we explain in a new study published in Nature Communications, we learned the toll on people’s wellbeing was evident across nations, not just in Ukraine. These effects appear to have been temporary – at least for the average person.
But people with certain psychological vulnerabilities struggled to recover from the shock of the war.
Tracking wellbeing during the outbreak of war
People who took part in our study completed a rigorous “experience-sampling” protocol. Specifically, we asked them to report their momentary wellbeing four times per day for a whole month.
Data collection began in October 2021 and continued throughout 2022. So we had been tracking wellbeing around the world during the weeks surrounding the outbreak of war in February 2022.
We also collected measures of personality, along with various sociodemographic variables (including age, gender, political views). This enabled us to assess whether different people responded differently to the crisis. We could also compare these effects across countries.
Our analyses focused primarily on 1,341 participants living in 17 European countries, excluding Ukraine itself (44,894 experience-sampling reports in total). We also expanded these analyses to capture the experiences of 1,735 people living in 43 countries around the world (54,851 experience-sampling reports) – including in Australia.
A global dip in wellbeing
On February 24 2022, the day Russia invaded Ukraine, there was a sharp decline in wellbeing around the world. There was no decline in the month leading up to the outbreak of war, suggesting the change in wellbeing was not already occurring for some other reason.
However, there was a gradual increase in wellbeing during the month after the Russian invasion, suggestive of a “return to baseline” effect. Such effects are commonly reported in psychological research: situations and events that impact our wellbeing often (though not always) do so temporarily.
Unsurprisingly, people in Europe experienced a sharper dip in wellbeing compared to people living elsewhere around the world. Presumably the war was much more salient for those closest to the conflict, compared to those living on an entirely different continent.
Interestingly, day-to-day fluctuations in wellbeing mirrored the salience of the war on social media as events unfolded. Specifically, wellbeing was lower on days when there were more tweets mentioning Ukraine on Twitter/X.
Our results indicate that, on average, it took around two months for people to return to their baseline levels of wellbeing after the invasion.
Different people, different recoveries
There are strong links between our wellbeing and our individual personalities.
However, the dip in wellbeing following the Russian invasion was fairly uniform across individuals. None of the individual factors assessed in our study, including personality and sociodemographic factors, predicted people’s response to the outbreak of war.
On the other hand, personality did play a role in how quickly people recovered. Individual differences in people’s recovery were linked to a personality trait called “stability”. Stability is a broad dimension of personality that combines low neuroticism with high agreeableness and conscientiousness (three traits from the Big Five personality framework).
Stability is so named because it reflects the stability of one’s overall psychological functioning. This can be illustrated by breaking stability down into its three components:
- low neuroticism describes emotional stability. People low in this trait experience less intense negative emotions such as anxiety, fear or anger, in response to negative events
- high agreeableness describes social stability. People high in this trait are generally more cooperative, kind, and motivated to maintain social harmony
- high conscientiousness describes motivational stability. People high in this trait show more effective patterns of goal-directed self-regulation.
So, our data show that people with less stable personalities fared worse in terms of recovering from the impact the war in Ukraine had on wellbeing.
In a supplementary analysis, we found the effect of stability was driven specifically by neuroticism and agreeableness. The fact that people higher in neuroticism recovered more slowly accords with a wealth of research linking this trait with coping difficulties and poor mental health.
These effects of personality on recovery were stronger than those of sociodemographic factors, such as age, gender or political views, which were not statistically significant.
Overall, our findings suggest that people with certain psychological vulnerabilities will often struggle to recover from the shock of global events such as the outbreak of war in Ukraine.
Luke Smillie, Professor in Personality Psychology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: