Grains: Bread Of Life, Or Cereal Killer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Going Against The Grain?
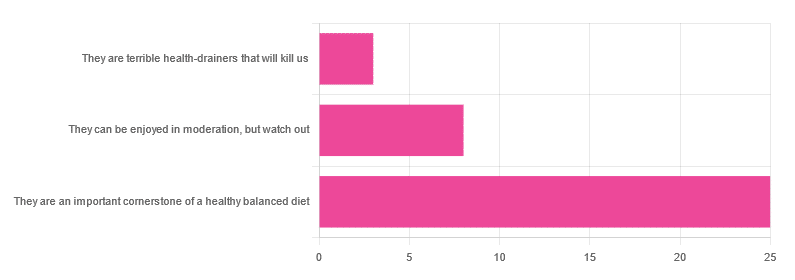
In Wednesday’s newsletter, we asked you for your health-related opinion of grains (aside from any gluten-specific concerns), and got the above-depicted, below-described, set of responses:
- About 69% said “They are an important cornerstone of a healthy balanced diet”
- About 22% said “They can be enjoyed in moderation, but watch out”
- About 8% said “They are terrible health-drainers that will kill us”
So, what does the science say?
They are terrible health-drainers that will kill us: True or False?
True or False depending on the manner of their consumption!
There is a big difference between the average pizza base and a bowl of oats, for instance. Or rather, there are a lot of differences, but what’s most critical here?
The key is: refined and ultraprocessed grains are so inferior to whole grains as to be actively negative for health in most cases for most people most of the time.
But! It’s not because processing is ontologically evil (in reality: some processed foods are healthy, and some unprocessed foods are poisonous). although it is a very good general rule of thumb.
So, we need to understand the “why” behind the “key” that we just gave above, and that’s mostly about the resultant glycemic index and associated metrics (glycemic load, insulin index, etc).
In the case of refined and ultraprocessed grains, our body gains sugar faster than it can process it, and stores it wherever and however it can, like someone who has just realised that they will be entertaining a houseguest in 10 minutes and must tidy up super-rapidly by hiding things wherever they’ll fit.
And when the body tries to do this with sugar from refined grains, the result is very bad for multiple organs (most notably the liver, but the pancreas takes quite a hit too) which in turn causes damage elsewhere in the body, not to mention that we now have urgently-produced fat stored in unfortunate places like our liver and abdominal cavity when it should have gone to subcutaneous fat stores instead.
In contrast, whole grains come with fiber that slows down the absorption of the sugars, such that the body can deal with them in an ideal fashion, which usually means:
- using them immediately, or
- storing them as muscle glycogen, or
- storing them as subcutaneous fat
👆 that’s an oversimplification, but we only have so much room here.
For more on this, see:
Glycemic Index vs Glycemic Load vs Insulin Index
And for why this matters, see:
Which Sugars Are Healthier, And Which Are Just The Same?
And for fixing it, see:
They can be enjoyed in moderation, but watch out: True or False?
Technically True but functionally False:
- Technically true: “in moderation” is doing a lot of heavy lifting here. One person’s “moderation” may be another person’s “abstemiousness” or “gluttony”.
- Functionally false: while of course extreme consumption of pretty much anything is going to be bad, unless you are Cereals Georg eating 10,000 cereals each day and being a statistical outlier, the issue is not the quantity so much as the quality.
Quality, we discussed above—and that is, as we say, paramount. As for quantity however, you might want to know a baseline for “getting enough”, so…
They are an important cornerstone of a healthy balanced diet: True or False?
True! This one’s quite straightforward.
3 servings (each being 90g, or about ½ cup) of whole grains per day is associated with a 22% reduction in risk of heart disease, 5% reduction in all-cause mortality, and a lot of benefits across a lot of disease risks:
❝This meta-analysis provides further evidence that whole grain intake is associated with a reduced risk of coronary heart disease, cardiovascular disease, and total cancer, and mortality from all causes, respiratory diseases, infectious diseases, diabetes, and all non-cardiovascular, non-cancer causes.
These findings support dietary guidelines that recommend increased intake of whole grain to reduce the risk of chronic diseases and premature mortality.❞
~ Dr. Dagfinn Aune et al.
We’d like to give a lot more sources for the same findings, as well as papers for all the individual claims, but frankly, there are so many that there isn’t room. Suffice it to say, this is neither controversial nor uncertain; these benefits are well-established.
Here’s a very informative pop-science article, that also covers some of the things we discussed earlier (it shows what happens during refinement of grains) before getting on to recommendations and more citations for claims than we can fit here:
Harvard School Of Public Health | Whole Grains
“That’s all great, but what if I am concerned about gluten?”
There certainly are reasons you might be, be it because of a sensitivity, allergy, or just because perhaps you’d like to know more.
Let’s first mention: not all grains contain gluten, so it’s perfectly possible to enjoy naturally gluten-free grains (such as oats and rice) as well as gluten-free pseudocereals, which are not actually grains but do the same job in culinary and nutritional terms (such as quinoa and buckwheat, despite the latter’s name).
Finally, if you’d like to know more about gluten’s health considerations, then check out our previous mythbusting special:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What pathogen might spark the next pandemic? How scientists are preparing for ‘disease X’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Before the COVID pandemic, the World Health Organization (WHO) had made a list of priority infectious diseases. These were felt to pose a threat to international public health, but where research was still needed to improve their surveillance and diagnosis. In 2018, “disease X” was included, which signified that a pathogen previously not on our radar could cause a pandemic.
While it’s one thing to acknowledge the limits to our knowledge of the microbial soup we live in, more recent attention has focused on how we might systematically approach future pandemic risks.
Former US Secretary of Defense Donald Rumsfeld famously talked about “known knowns” (things we know we know), “known unknowns” (things we know we don’t know), and “unknown unknowns” (the things we don’t know we don’t know).
Although this may have been controversial in its original context of weapons of mass destruction, it provides a way to think about how we might approach future pandemic threats.
Anna Shvets/Pexels Influenza: a ‘known known’
Influenza is largely a known entity; we essentially have a minor pandemic every winter with small changes in the virus each year. But more major changes can also occur, resulting in spread through populations with little pre-existing immunity. We saw this most recently in 2009 with the swine flu pandemic.
However, there’s a lot we don’t understand about what drives influenza mutations, how these interact with population-level immunity, and how best to make predictions about transmission, severity and impact each year.
The current H5N1 subtype of avian influenza (“bird flu”) has spread widely around the world. It has led to the deaths of many millions of birds and spread to several mammalian species including cows in the United States and marine mammals in South America.
Human cases have been reported in people who have had close contact with infected animals, but fortunately there’s currently no sustained spread between people.
While detecting influenza in animals is a huge task in a large country such as Australia, there are systems in place to detect and respond to bird flu in wildlife and production animals.
Scientists are continually monitoring a range of pathogens with pandemic potential. Edward Jenner/Pexels It’s inevitable there will be more influenza pandemics in the future. But it isn’t always the one we are worried about.
Attention had been focused on avian influenza since 1997, when an outbreak in birds in Hong Kong caused severe disease in humans. But the subsequent pandemic in 2009 originated in pigs in central Mexico.
Coronaviruses: an ‘unknown known’
Although Rumsfeld didn’t talk about “unknown knowns”, coronaviruses would be appropriate for this category. We knew more about coronaviruses than most people might have thought before the COVID pandemic.
We’d had experience with severe acute respiratory syndrome (SARS) and Middle Eastern respiratory syndrome (MERS) causing large outbreaks. Both are caused by viruses closely related to SARS-CoV-2, the coronavirus that causes COVID. While these might have faded from public consciousness before COVID, coronaviruses were listed in the 2015 WHO list of diseases with pandemic potential.
Previous research into the earlier coronaviruses proved vital in allowing COVID vaccines to be developed rapidly. For example, the Oxford group’s initial work on a MERS vaccine was key to the development of AstraZeneca’s COVID vaccine.
Similarly, previous research into the structure of the spike protein – a protein on the surface of coronaviruses that allows it to attach to our cells – was helpful in developing mRNA vaccines for COVID.
It would seem likely there will be further coronavirus pandemics in the future. And even if they don’t occur at the scale of COVID, the impacts can be significant. For example, when MERS spread to South Korea in 2015, it only caused 186 cases over two months, but the cost of controlling it was estimated at US$8 billion (A$11.6 billion).
COVID could be regarded as an ‘unknown known’. Markus Spiske/Pexels The 25 viral families: an approach to ‘known unknowns’
Attention has now turned to the known unknowns. There are about 120 viruses from 25 families that are known to cause human disease. Members of each viral family share common properties and our immune systems respond to them in similar ways.
An example is the flavivirus family, of which the best-known members are yellow fever virus and dengue fever virus. This family also includes several other important viruses, such as Zika virus (which can cause birth defects when pregnant women are infected) and West Nile virus (which causes encephalitis, or inflammation of the brain).
The WHO’s blueprint for epidemics aims to consider threats from different classes of viruses and bacteria. It looks at individual pathogens as examples from each category to expand our understanding systematically.
The US National Institute of Allergy and Infectious Diseases has taken this a step further, preparing vaccines and therapies for a list of prototype pathogens from key virus families. The goal is to be able to adapt this knowledge to new vaccines and treatments if a pandemic were to arise from a closely related virus.
Pathogen X, the ‘unknown unknown’
There are also the unknown unknowns, or “disease X” – an unknown pathogen with the potential to trigger a severe global epidemic. To prepare for this, we need to adopt new forms of surveillance specifically looking at where new pathogens could emerge.
In recent years, there’s been an increasing recognition that we need to take a broader view of health beyond only thinking about human health, but also animals and the environment. This concept is known as “One Health” and considers issues such as climate change, intensive agricultural practices, trade in exotic animals, increased human encroachment into wildlife habitats, changing international travel, and urbanisation.
This has implications not only for where to look for new infectious diseases, but also how we can reduce the risk of “spillover” from animals to humans. This might include targeted testing of animals and people who work closely with animals. Currently, testing is mainly directed towards known viruses, but new technologies can look for as yet unknown viruses in patients with symptoms consistent with new infections.
We live in a vast world of potential microbiological threats. While influenza and coronaviruses have a track record of causing past pandemics, a longer list of new pathogens could still cause outbreaks with significant consequences.
Continued surveillance for new pathogens, improving our understanding of important virus families, and developing policies to reduce the risk of spillover will all be important for reducing the risk of future pandemics.
This article is part of a series on the next pandemic.
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
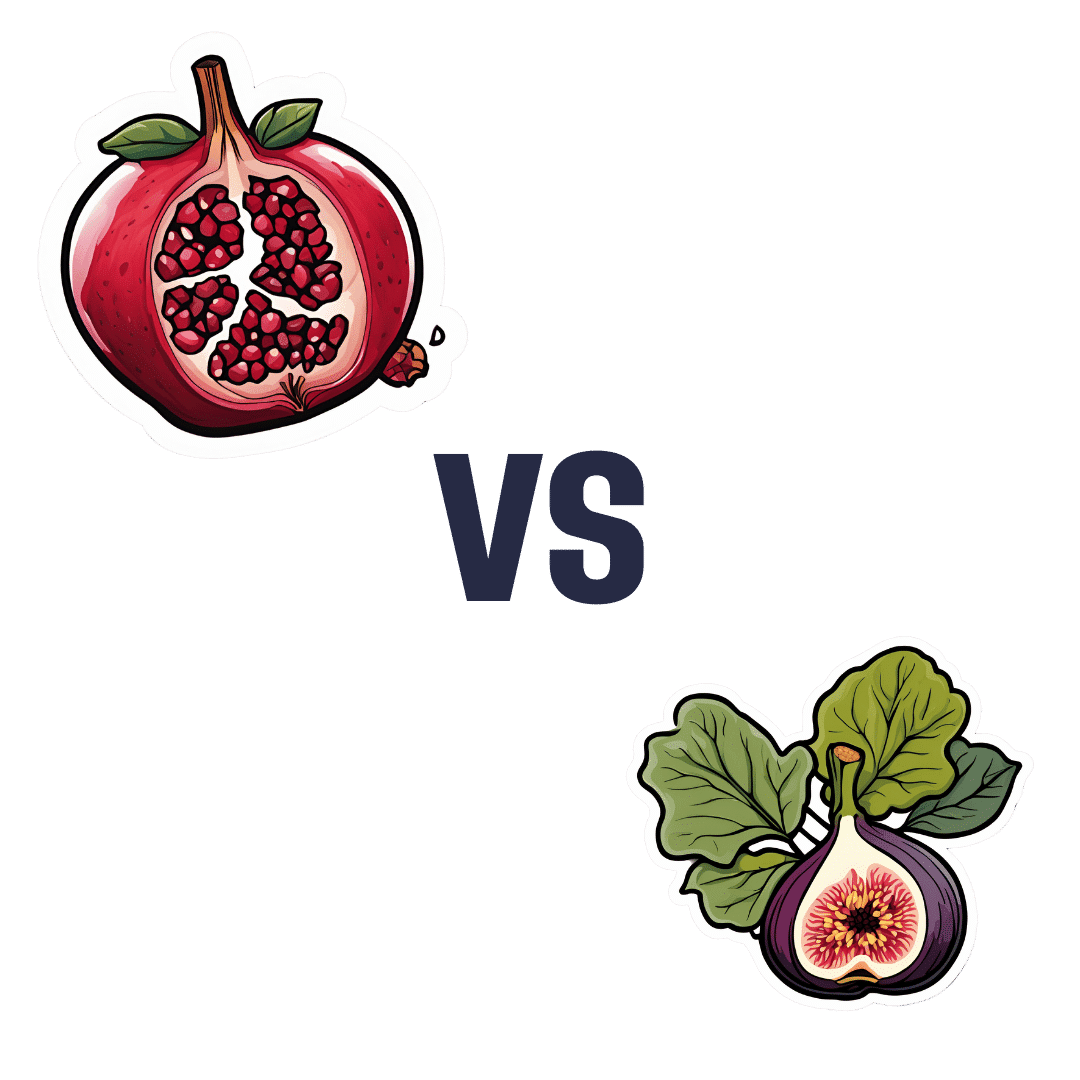
Pomegranate vs Figs – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pomegranate to figs, we picked the pomegranate.
Why?
In terms of macros, pomegranate has a lot more protein* and fiber, while the fig has more carbs. Thus, a win for pomegranate.
*Why such protein in a fruit? In both cases, it’s mostly from the seeds, which in both cases, we’re eating. However, pomegranates have a much greater seed-to-mass ratio than figs, and thus, a correspondingly higher amount of protein. Also some fats from the seeds, again more than figs, but the margin of difference is smaller, and not really enough to be of relevance.
In the category of vitamins, pomegranates lead with more of vitamins B1, B5, B9, C, E, K, and choline, while figs have more of vitamins A, B3, and B6. The largest margins of difference are in vitamins B9, E, and K, so all in pomegranate’s favor.
The minerals scene is closer to even; pomegranate has more copper, phosphorus, potassium, selenium, and zinc, while figs have more calcium, iron, magnesium, and manganese. Thus, a 5:4 lead for pomegranate, and the larger margins of difference are again for pomegranate.
In short, enjoy both, but pomegranates are the more nutritionally dense. Also, don’t throw away the peel! Dry it, and turn it into a powdered supplement—see our linked article below, for why:
Want to learn more?
You might like to read:
Pomegranate’s Health Gifts Are Mostly In Its Peel
Take care!
Share This Post
-
What’s the difference between shyness and social anxiety?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
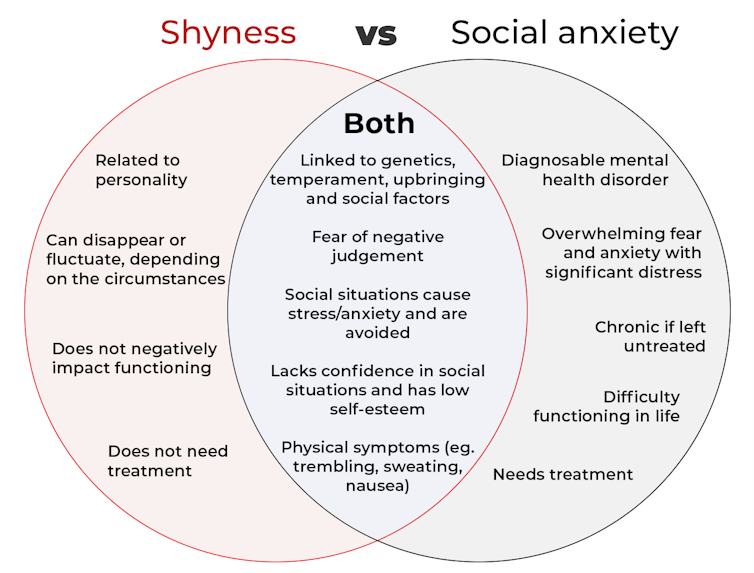
The terms “shyness” and “social anxiety” are often used interchangeably because they both involve feeling uncomfortable in social situations.
However, feeling shy, or having a shy personality, is not the same as experiencing social anxiety (short for “social anxiety disorder”).
Here are some of the similarities and differences, and what the distinction means.
pathdoc/Shutterstock How are they similar?
It can be normal to feel nervous or even stressed in new social situations or when interacting with new people. And everyone differs in how comfortable they feel when interacting with others.
For people who are shy or socially anxious, social situations can be very uncomfortable, stressful or even threatening. There can be a strong desire to avoid these situations.
People who are shy or socially anxious may respond with “flight” (by withdrawing from the situation or avoiding it entirely), “freeze” (by detaching themselves or feeling disconnected from their body), or “fawn” (by trying to appease or placate others).
A complex interaction of biological and environmental factors is also thought to influence the development of shyness and social anxiety.
For example, both shy children and adults with social anxiety have neural circuits that respond strongly to stressful social situations, such as being excluded or left out.
People who are shy or socially anxious commonly report physical symptoms of stress in certain situations, or even when anticipating them. These include sweating, blushing, trembling, an increased heart rate or hyperventilation.
How are they different?
Social anxiety is a diagnosable mental health condition and is an example of an anxiety disorder.
For people who struggle with social anxiety, social situations – including social interactions, being observed and performing in front of others – trigger intense fear or anxiety about being judged, criticised or rejected.
To be diagnosed with social anxiety disorder, social anxiety needs to be persistent (lasting more than six months) and have a significant negative impact on important areas of life such as work, school, relationships, and identity or sense of self.
Many adults with social anxiety report feeling shy, timid and lacking in confidence when they were a child. However, not all shy children go on to develop social anxiety. Also, feeling shy does not necessarily mean a person meets the criteria for social anxiety disorder.
People vary in how shy or outgoing they are, depending on where they are, who they are with and how comfortable they feel in the situation. This is particularly true for children, who sometimes appear reserved and shy with strangers and peers, and outgoing with known and trusted adults.
Individual differences in temperament, personality traits, early childhood experiences, family upbringing and environment, and parenting style, can also influence the extent to which people feel shy across social situations.
Not all shy children go on to develop social anxiety. 249 Anurak/Shutterstock However, people with social anxiety have overwhelming fears about embarrassing themselves or being negatively judged by others; they experience these fears consistently and across multiple social situations.
The intensity of this fear or anxiety often leads people to avoid situations. If avoiding a situation is not possible, they may engage in safety behaviours, such as looking at their phone, wearing sunglasses or rehearsing conversation topics.
The effect social anxiety can have on a person’s life can be far-reaching. It may include low self-esteem, breakdown of friendships or romantic relationships, difficulties pursuing and progressing in a career, and dropping out of study.
The impact this has on a person’s ability to lead a meaningful and fulfilling life, and the distress this causes, differentiates social anxiety from shyness.
Children can show similar signs or symptoms of social anxiety to adults. But they may also feel upset and teary, irritable, have temper tantrums, cling to their parents, or refuse to speak in certain situations.
If left untreated, social anxiety can set children and young people up for a future of missed opportunities, so early intervention is key. With professional and parental support, patience and guidance, children can be taught strategies to overcome social anxiety.
Why does the distinction matter?
Social anxiety disorder is a mental health condition that persists for people who do not receive adequate support or treatment.
Without treatment, it can lead to difficulties in education and at work, and in developing meaningful relationships.
Receiving a diagnosis of social anxiety disorder can be validating for some people as it recognises the level of distress and that its impact is more intense than shyness.
A diagnosis can also be an important first step in accessing appropriate, evidence-based treatment.
Different people have different support needs. However, clinical practice guidelines recommend cognitive-behavioural therapy (a kind of psychological therapy that teaches people practical coping skills). This is often used with exposure therapy (a kind of psychological therapy that helps people face their fears by breaking them down into a series of step-by-step activities). This combination is effective in-person, online and in brief treatments.
Treatment is available online as well as in-person. ImYanis/Shutterstock For more support or further reading
Online resources about social anxiety include:
- This Way Up’s online program for managing excessive shyness and fear of social situations
- Beyond Blue’s resources on social anxiety
- a guide to looking after yourself if you have social anxiety, from the Western Australian health department
- social anxiety online program for children and teens from the University of Queensland
- inroads, a self-guided online program for young adults who drink alcohol to manage their anxiety.
We thank the Black Dog Institute Lived Experience Advisory Network members for providing feedback and input for this article and our research.
Kayla Steele, Postdoctoral research fellow and clinical psychologist, UNSW Sydney and Jill Newby, Professor, NHMRC Emerging Leader & Clinical Psychologist, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
I’m So Effing Tired – by Dr. Amy Shah
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy sometimes to feel like we know more or less what we should be doing… If only we had the energy to get going!
- We know we want a better diet… But we don’t have the time/energy to cook so will go for the quickest option even when it’s not the best?
- We know we should exercise… But feel we just need to crash out on the couch for a bit first?
- We would dearly love to get better sleep… But our responsibilities aren’t facilitating that?
…and so on. Happily, Dr. Amy Shah is here with ways to cut through the Gordian Knot that is this otherwise self-perpetuating cycle of exhaustion.
Most of the book is based around tackling what Dr. Shah calls “the energy trifecta“:
- Hormone levels
- Immune system
- Gut health
You’ll note (perhaps with relief) that none of these things require an initial investment of energy that you don’t have… She’s not asking you to hit the gym at 5am, or magically bludgeon your sleep schedule into its proper place, say.
Instead, what she gives is practical, actionable, easy changes that don’t require much effort, to gently slide us back into the fast lane of actually having energy to do stuff!
In short: if you’ve ever felt like you’d like to implement a lot of very common “best practice” lifestyle advice, but just haven’t had the energy to get going, there’s more value in this handbook than in a thousand motivational pep talks.
Click here to check out “I’m So Effing Tired” and get on a better track of life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Body Scrubs: Benefits, Risks, and Guidance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering whether I should be using a body scrub in the shower, rather than just soap. What should guide me in the choice of a body scrub, and are there any risks to be aware of?❞
Body scrubs are great for giving skin a healthy glow, but are best used sparingly—over-exfoliation leads to the opposite effect (unhappy skin, premature skin aging, etc).
As for contents:
- microplastics are now banned in most places, but you might want to check any products (and their containers!) are BPA-free, pthalate free, etc.
- fragrances in body scrubs are usually a bad idea, and many essential oils have been shown to be endocrine-disruptors, which you do not want:
About the microplastics, harmful artificial chemicals in general, and what constitutes “etc”:
About the fragrances’ (including “natural” essential oils’) endocrine-disrupting shenanigans:
Endocrine-disrupting chemicals: an Endocrine Society scientific statement
So, what might you want to use instead?
If you’re feeling adventurous, you might like to try treating yourself to a pineapple-based mask instead (a muslin cloth soaked in pineapple juice will work just fine; please don’t waterboard yourself though), as the bromelain enzymes (found very generously in pineapple juice) break down dead cells without the need for scrubbing.
Another option is a homemade salt- or sugar-scrub. Put your salt or sugar into a jar, add enough warm water to cover it, leave it for about a day, adding more water if it seems in danger of drying out, until it recrystallizes with a high water content keeping it malleable to the touch; congratulations, you now have a very simple scrub. This should still not be used more than, say, once per week, though.
Last but not least, you might consider investing in a konjac sponge; they gently remove dead skin without damaging living skin. Here’s an example product on Amazon, for your convenience
For more on gentle-yet-effective skincare, you might like to read:
Clean: The New Science of Skin and the Beauty of Doing Less
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A New $16,000 Postpartum Depression Drug Is Here. How Will Insurers Handle It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A much-awaited treatment for postpartum depression, zuranolone, hit the market in December, promising an accessible and fast-acting medication for a debilitating illness. But most private health insurers have yet to publish criteria for when they will cover it, according to a new analysis of insurance policies.
The lack of guidance could limit use of the drug, which is both novel — it targets hormone function to relieve symptoms instead of the brain’s serotonin system, as typical antidepressants do — and expensive, at $15,900 for the 14-day pill regimen.
Lawyers, advocates, and regulators are watching closely to see how insurance companies will shape policies for zuranolone because of how some handled its predecessor, an intravenous form of the same drug called brexanolone, which came on the market in 2019. Many insurers required patients to try other, cheaper medications first — known as the fail-first approach — before they could be approved for brexanolone, which was shown in early trials reviewed by the FDA to provide relief within days. Typical antidepressants take four to six weeks to take effect.
“We’ll have to see if insurers cover this drug and what fail-first requirements they put in” for zuranolone, said Meiram Bendat, a licensed psychotherapist and an attorney who represents patients.
Most health plans have yet to issue any guidelines for zuranolone, and maternal health advocates worry that the few that have are taking a restrictive approach. Some policies require that patients first try and fail a standard antidepressant before the insurer will pay for zuranolone.
In other cases, guidelines require psychiatrists to prescribe it, rather than obstetricians, potentially delaying treatment since OB-GYN practitioners are usually the first medical providers to see signs of postpartum depression.
Advocates are most worried about the lack of coverage guidance.
“If you don’t have a published policy, there is going to be more variation in decision-making that isn’t fair and is less efficient. Transparency is really important,” said Joy Burkhard, executive director of the nonprofit Policy Center for Maternal Mental Health, which commissioned the study.
With brexanolone, which was priced at $34,000 for the three-day infusion, California’s largest insurer, Kaiser Permanente, had such rigorous criteria for prescribing it that experts said the policy amounted to a blanket denial for all patients, according to an NPR investigation in 2021.
KP’s written guidelines required patients to try and fail four medications and electroconvulsive therapy before they would be eligible for brexanolone. Because the drug was approved only for up to six months postpartum, and trials of typical antidepressants take four to six weeks each, the clock would run out before a patient had time to try brexanolone.
An analysis by NPR of a dozen other health plans at the time showed Kaiser Permanente’s policy on brexanolone to be an outlier. Some did require that patients fail one or two other drugs first, but KP was the only one that recommended four.
Miriam McDonald, who developed severe postpartum depression and suicidal ideation after giving birth in late 2019, battled Kaiser Permanente for more than a year to find effective treatment. Her doctors put her on a merry-go-round of medications that didn’t work and often carried unbearable side effects, she said. Her doctors refused to prescribe brexanolone, the only FDA-approved medication specifically for postpartum depression at the time.
“No woman should suffer like I did after having a child,” McDonald said. “The policy was completely unfair. I was in purgatory.”
One month after NPR published its investigation, KP overhauled its criteria to recommend that women try just one medication before becoming eligible for brexanolone.
Then, in March 2023, after the federal Department of Labor launched an investigation into the insurer — citing NPR’s reporting — the insurer revised its brexanolone guidelines again, removing all fail-first recommendations, according to internal documents recently obtained by NPR. Patients need only decline a trial of another medication.
“Since brexanolone was first approved for use, more experience and research have added to information about its efficacy and safety,” the insurer said in a statement. “Kaiser Permanente is committed to ensuring brexanolone is available when physicians and patients determine it is an appropriate treatment.”
“Kaiser basically went from having the most restrictive policy to the most robust,” said Burkhard of the Policy Center for Maternal Mental Health. “It’s now a gold standard for the rest of the industry.”
McDonald is hopeful that her willingness to speak out and the subsequent regulatory actions and policy changes for brexanolone will lead Kaiser Permanente and other health plans to set patient-friendly policies for zuranolone.
“This will prevent other women from having to go through a year of depression to find something that works,” she said.
Clinicians were excited when the FDA approved zuranolone last August, believing the pill form, taken once a day at home over two weeks, will be more accessible to women compared with the three-day hospital stay for the IV infusion. Many perinatal psychiatrists told NPR it is imperative to treat postpartum depression as quickly as possible to avoid negative effects, including cognitive and social problems in the baby, anxiety or depression in the father or partner, or the death of the mother to suicide, which accounts for up to 20% of maternal deaths.
So far, only one of the country’s six largest private insurers, Centene, has set a policy for zuranolone. It is unclear what criteria KP will set for the new pill. California’s Medicaid program, known as Medi-Cal, has not yet established coverage criteria.
Insurers’ policies for zuranolone will be written at a time when the regulatory environment around mental health treatment is shifting. The U.S. Department of Labor is cracking down on violations of the Mental Health Parity and Addiction Equity Act of 2008, which requires insurers to cover psychiatric treatments the same as physical treatments.
Insurers must now comply with stricter reporting and auditing requirements intended to increase patient access to mental health care, which advocates hope will compel health plans to be more careful about the policies they write in the first place.
In California, insurers must also comply with an even broader state mental health parity law from 2021, which requires them to use clinically based, expert-recognized criteria and guidelines in making medical decisions. The law was designed to limit arbitrary or cost-driven denials for mental health treatments and has been hailed as a model for the rest of the country. Much-anticipated regulations for the law are expected to be released this spring and could offer further guidance for insurers in California setting policies for zuranolone.
In the meantime, Burkhard said, patients suffering from postpartum depression should not hold back from asking their doctors about zuranolone. Insurers can still grant access to the drug on a case-by-case basis before they formalize their coverage criteria.
“Providers shouldn’t be deterred from prescribing zuranolone,” Burkhard said.
This article is from a partnership that includes KQED, NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: